Abstract
Background
Obesity has been positively associated with gastric cancer. Excess fat impacts hormones, which have been implicated in carcinogenesis. We investigated obesity-related hormones and cardia gastric cancer (CGC) and non-cardia gastric cancer (NCGC) risk.
Methods
Nested case–control studies were conducted within the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort (61 CGCs, and 172 NCGCs and matched controls) and the Alpha-Tocopherol, Beta-Carotene Cancer Prevention (ATBC) study (100 CGCs and 65 NCGCs and matched controls); serum hormones were measured. In UK-Biobank (n = 458,713), we included 137 CGCs and 92 NCGCs. Sex-specific analyses were conducted. For EPIC and ATBC, odds ratios (ORs), and for UK-Biobank hazard ratios (HRs), were estimated using conditional logistic regression and Cox regression, respectively.
Results
Insulin-like growth-factor-1 was positively associated with CGC and NCGC in EPIC men (ORper 1-SD increase 1.94, 95% CI 1.03–3.63; ORper 1-SD increase 1.63, 95% CI 1.05–2.53, respectively), with similar findings for CGC in UK-Biobank women (HRper 1-SD increase 1.76, 95% CI 1.08–2.88). Leptin in EPIC men and C-peptide in EPIC women were positively associated with NCGC (ORT3 vs. T1 2.72, 95% CI 1.01–7.34 and ORper 1-SD increase 2.17, 95% CI 1.19–3.97, respectively). Sex hormone-binding globulin was positively associated with CGC in UK-Biobank men (HRper 1-SD increase 1.29, 95% CI 1.02–1.64). Conversely, ghrelin was inversely associated with NCGC among EPIC and ATBC men (ORper 1-SD increase 0.53, 95% CI 0.34–0.84; ORper 1-SD increase 0.22, 95% CI 0.10–0.50, respectively). In addition, dehydroepiandrosterone was inversely associated with CGC in EPIC and ATBC men combined.
Conclusions
Some obesity-related hormones influence CGC and NCGC risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastric cancer is among the most commonly diagnosed cancers globally [1]. There are striking differences in the risk factor profiles for the two gastric cancer subsites: cardia gastric cancer (CGC) and non-cardia gastric cancer (NCGC). Obesity is positively associated with CGC [2,3,4,5], and with gastro-esophageal reflux disease [6], while Helicobacter pylori infection is one of the most significant risk factors for NCGC [6]. Incidence rates for gastric cancer overall are two-fold higher in men than in women [1], but this sex imbalance is more pronounced in CGC than in NCGC [5]. Obesity can alter circulating hormone levels: insulin, leptin and sex steroid hormones are higher in obese individuals, while adiponectin levels are lower [7].
Insulin regulates glucose metabolism [8] and, in non-fasting blood samples, it can be estimated using C-peptide levels [9]. A previous nested case–control study showed a positive association between insulin and C-peptide levels and gastric cancer [10]. Insulin-like growth factor-1 (IGF-1), similar in structure to insulin, is regulated via insulin-like growth factor-binding proteins (IGFBPs) and 80% of IGF-1 is bound to IGFBP-3 [11]. Previous prospective studies investigated the associations between serum levels of IGF-1 and IGFBP-3 and risk of gastric cancer and reported no associations [12,13,14]. However, gastric cancer subsite was not previously examined.
Adiponectin and leptin are hormones produced in adipose tissue. Adiponectin regulates glucose and lipid metabolism [15] and leptin regulates appetite and energy balance [16]. Previous studies have reported lower levels of adiponectin and leptin in gastric cancer patients than controls [17, 18]. In contrast to leptin, ghrelin is produced in the stomach and stimulates appetite, increasing food intake [16]. Previous studies have reported low levels of ghrelin are associated with an increased risk of both CGC and NCGC [19, 20] but data on sex-specific associations are limited.
Sex steroid hormones influence body fat distribution [21] and adipose tissue is a major source of estrogens and androgens in obese individuals. It has been hypothesized that sex hormones may explain the male predominance in gastric cancer. Several cohort studies have investigated the associations between self-reported reproductive factors, such as hormone replacement therapy use, and gastric cancer risk [3, 4, 22, 23]. However, prospective studies examining the associations between circulating sex steroids and risk of gastric cancer by subsite are also limited [24,25,26].
We aimed to investigate the associations between a range of circulating hormones related to obesity and risk of gastric cancer by subsite in three prospective cohort studies.
Methods
Study population
The three participating prospective cohort studies were: the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort [27], the Alpha-Tocopherol, Beta-Carotene Cancer Prevention (ATBC) Study [28] and the UK-Biobank cohort [29]. The study design and rationale of each participating cohort has been described in detail previously [27,28,29].
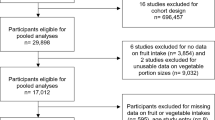
The EPIC cohort includes 521,324 men and women, recruited between 1992 and 2000 from 10 European countries; for this analysis, we had follow-up through 2012 [27]. The ATBC Study is a randomized controlled trial of 29,133 men initiated in 1985 to investigate the effects of alpha-tocopherol and beta-carotene supplementation on cancer risk in Finnish smokers; this analysis included data on incident cancers through 2012 [28]. The UK-Biobank cohort consists of 502,524 men and women from the UK enrolled between 2006 and 2010 to investigate a wide range of health conditions and illnesses, with follow-up through 2016 [29]. Characteristics of the participating cohorts are presented in Supplementary Table 1. Each study was approved by the relevant local institutional review boards.
Within EPIC and ATBC, we conducted nested case–control studies. In both cohorts, incidence-density sampling was used where one control was matched to each case (controls were alive and cancer-free at the time of case diagnosis). In EPIC, controls were matched to cases on recruitment center, sex, age at enrolment (± 3 years) and date (± 3 months) and time (± 3 h) of blood sample collection (Supplementary Table 1). In the ATBC study, case and control subjects were matched on age at randomization (± 1 year), and date of blood draw (± 30 days) (Supplementary Table 1). UK-Biobank was analyzed as a cohort study because circulating hormone levels were available on the majority of participants; we excluded participants with prevalent cancer at recruitment (n = 43,811), leaving 458,713 available for analysis.
Cancer cases were mostly identified through cancer registries. Cases were first primary incident gastric cancer coded according to the International Classification of Diseases (ICD-9 or 10). CGC and NCGC included topography codes C16.0 and C16.1–16.6, respectively. In EPIC, there were 61 CGC cases and 61 controls in men (there were too few CGC cases among women), and 172 NCGC cases and 172 controls in men and women combined. In the all-male ATBC cohort, there were 100 CGC cases matched to 100 controls and 65 NCGC cases matched to 65 controls. Of these CGC and NCGC cases and controls in ATBC, 84 CGC cases and 10 controls, and all of the 65 NCGC cases and 65 controls overlapped with a previous nested case–control study in ATBC [19]. In the UK-Biobank cohort, there were 137 CGC cases and 92 NCGC cases in men and women combined.
Data and sample collection
All three studies collected information on socio-demographic, dietary, lifestyle and medical history mainly via a self-administered questionnaire at baseline. Furthermore, anthropometric measurements and fasting serum samples were collected at baseline. Details of data and specimen collection have been described previously by the individual studies [27,28,29].
Hormone measurements
In each of the three cohorts, there were slight differences in the hormones measured due to volume availability.
EPIC: The hormones measured in EPIC for CGC and NCGC were insulin, IGF-1, IGFBP-3, C-peptide, adiponectin, leptin, ghrelin, androstenedione, dehydroepiandrosterone (DHEA), estrone, estradiol, sex hormone-binding globulin (SHBG), progesterone and testosterone.
ATBC: In ATBC, hormones measured for CGC included insulin, IGF-1, IGFBP-3, leptin and adiponectin, which were new measurements, while ghrelin, androstenedione, androsterone, DHEA, estrone, estradiol, SHBG, dihydrotestosterone and testosterone were measured as part of previous nested case–control studies [19, 24]. Furthermore, most of the hormones measured for NCGC in ATBC were new measurements including insulin, IGF-1, IGFBP-3, adiponectin, leptin, androstenedione, DHEA, estrone, estradiol, SHBG, progesterone and testosterone, while only ghrelin had been measured for a previous nested case–control study [19].
For EPIC and most of the biomarkers in ATBC mentioned above, assays were performed at the International Agency for Research on Cancer (IARC) (Lyon, France) using commercially available immunoassays: adiponectin, leptin, and insulin were measured using electrochemioluminescence assays by Meso Scale Diagnostics (Rockville, MD, USA), IGF-1 and IGFBP-3 were measured by ELISAs from R&D (Minneapolis, USA), SHBG by ELISAs from DRG Diagnostics (Marburg, Germany) and ghrelin by an ELISA kit from Merck (Fontenay sous Bois, France). In ATBC, ghrelin was measured for CGC and NCGC by radioimmunoassay using reagents obtained from Millipore Linco Research (St Charles, Missouri, USA). The intra-batch coefficients of variation (CV) values were: 5.4–7.2% for insulin, 3.4–6.4% for C-peptide, 1.8–2.4% for IGF-1, 2.1–3.3% for IGFBP-3, 11.6% for ghrelin, and 1.8–3.0% for SHBG. Sex steroids were measured for CGC and NCGC in EPIC and for NCGC in ATBC by liquid chromatography–mass spectrometry (Ultimate 3000-Q-Exactive, Thermo Scientific) at IARC using an adaptation of a previously published method [30]. In brief, serum samples were prepared by liquid–liquid extraction, derivatized by 1,2-dimethylimidazole-5-sulfonyl chloride, with separation on a reversed phase column and ionization using atmospheric pressure chemical ionization in positive polarity [30]. In ATBC, sex steroids were measured for CGC by gas chromatography–mass spectrometry performed at the Pharmacogenomics Laboratory of Laval University (Quebec, Canada). The intra-batch CV values were: 2.5–3.5% for androstenedione, 2.9–5.2% for DHEA, 5.1–7.6% for estrone, 4.5–7.2% for estradiol, 1.8–3.3% for testosterone and 3.9–7.6% for progesterone. Serum concentrations of free estradiol and free testosterone were calculated from absolute concentrations of estradiol and testosterone, respectively, and SHBG using mass action equations [31].
UK-Biobank: A wide range of biomarkers were already measured in all UK-Biobank participants [32]. In addition to IGF-1, we were able to examine glucose, as well as glycated hemoglobin (HbA1c), SHBG and testosterone. Furthermore, C-reactive protein (CRP), a marker of inflammation, was also examined as evidence shows that chronic inflammation is associated with obesity and may contribute to cancer development [33]. Details on assay methods have been published previously [32]. The within-laboratory CV for low, medium and high internal quality control samples for the examined biomarkers were: 5.3–6.2% for IGF-1, 1.5–1.8% for glucose, 1.7–2.3% for CRP, 5.2–5.7% for SHBG and 3.7–8.3% for testosterone [32].
Statistical analysis
Hormone measurements were log transformed and both categorical (tertiles) and continuous (per 1-standard deviation (SD) increase) variables were analyzed. In EPIC and ATBC, categories were defined on the distribution among control subjects, whereas in UK-Biobank, it was based on the entire cohort. For hormone variables, those with missing values were assigned to a missing category. For instance, we classified hormones into categories (IGF-1 included those with values < 82, 82–104, > 104 (ng/mL) and those who were missing IGF-1 data). Also, for covariates with missing values, missing indicators were used. Baseline characteristics among cases and controls were compared using paired sampled t-tests (continuous variables) and paired Chi-squared tests (categorical variables).
For the two nested case–control studies (EPIC and ATBC), we used conditional logistic regression models to estimate odds ratio (ORs) and 95% confidence intervals (CIs) for the association between hormones and gastric cancer by subsite. Sex-specific analyses were conducted. Models were adjusted for education (EPIC: none, primary school, technical/professional, secondary school, university; ATBC: 8th grade or less, less than high school, high school graduate or general educational development, some college or technical school, college graduate), smoking (EPIC: never smoker, current smoker of 1–15, 16–25 or 26+ cigarettes/day, former smoker who stopped ≤ 10, 11–20 or 20 + years ago, current or occasional pipe/cigar, smoking unknown/missing; ATBC: < 24, 24 to < 35, 35 to < 46, ≥ 46 pack years) and body mass index (BMI, kg/m2, continuous). In addition, a pooled analysis of EPIC men with ATBC (all men) was performed to enhance statistical power since these two studies used the same study design (nested case–control studies); this pooled analysis did not include UK-Biobank since this was analyzed as a cohort study because, unlike EPIC and ATBC, biomarkers were measured on the entire cohort. Models were adjusted for education level, study center, smoking, and BMI. Additionally, for CGC in ATBC, we conducted a sensitivity analysis to examine the exposures measured as part of a previous nested case–control study and those that were not.
For UK-Biobank, hazard ratios (HRs) and 95% CIs were computed using Cox proportional hazard regression models, with age as the primary time variable. Entry time was age at recruitment and exit time was age at diagnosis, death or last date at which follow-up was considered complete. Sex-specific analyses were conducted. Models were stratified by age at recruitment in 5-year categories, Townsend deprivation index (quintiles) and recruitment center. Mean and SD or frequencies were computed for baseline characteristics. Models were adjusted for education (none; CSEs/O levels/GCSEs or equivalent; vocational qualifications {NVQ/HND/HNC, A-levels/AS levels or equivalent}; other qualifications; college/university degree; unknown), smoking (never, former and current) and BMI (kg/m2, continuous).
Linear trend tests were conducted for hormones by assigning the median value to each category as a continuous variable in the models. Pearson correlations were computed between hormones in each study. We also examined models mutually adjusted for (1) all of the gut/adipokines and (2) all of the sex hormones. A sensitivity analysis was performed by excluding gastric cancer cases diagnosed in the first year of follow-up. Furthermore, for hormones without sex differences in EPIC and UK-Biobank, we conducted combined sex analyses. All analyses were conducted using SAS 9.4 software (SAS Institute, Cary, NC) and P values < 0.05 were considered statistically significant.
Results
The median time between blood collection and cancer diagnosis in EPIC was 8.0 years for CGC and 8.4 years for NCGC, in ATBC, it was 9.0 years for CGC and 7.0 years for NCGC, and in UK-Biobank, it was 2.8 years for CGC and 3.2 years for NCGC (Supplementary Table 2, 3 and 4, respectively). In EPIC, CGC cases had higher red meat intake than controls (P = 0.04); while NCGC cases were less educated (P = 0.006) and had lower levels of IGFBP-3 (P = 0.02) and ghrelin (P = 0.009) than controls (Supplementary Table 2). In ATBC, CGC cases had higher BMI (P = 0.02) and lower levels of adiponectin (P = 0.03) and ghrelin (P = 0.02) than controls, while NCGC cases had lower vegetable intake (P = 0.03) and lower levels of insulin (P = 0.02), and ghrelin (P < 0.0001) compared to controls (Supplementary Table 3). In UK-Biobank, CGC cases had a lower education level (P = 0.0002), were older (P < 0.0001), had higher BMI (P < 0.0001), and were more likely to be smokers (P < 0.0001) and alcohol consumers (P < 0.0001); in addition, they had higher levels of glucose (P = 0.007), HbA1c (P = 0.02), CRP (P = 0.008), and testosterone (P < 0.0001), but lower levels of SHBG (P = 0.002) than non-cases (Supplementary Table 4). For NCGC, cases were also less educated (P = 0.001), older (P < 0.0001), consumed less alcohol (P = 0.02) and had higher levels of glucose (P = 0.04), HbA1c (P = 0.001), CRP (P = 0.009) and testosterone (P = 0.006) but had lower levels of IGF-1 (P = 0.008) compared to non-cases (Supplementary Table 4).
In EPIC men, IGF-1 was positively associated with CGC and NCGC (per 1-SD increase: adjusted OR 1.94, 95% CI 1.03–3.63 and 1.63, 95% CI 1.05–2.53, respectively) (Table 1). In addition, leptin was also positively associated with NCGC but only in categorical data (OR 2.72, 95% CI 1.01–7.34 for the highest vs. lowest category), whereas ghrelin was inversely associated with NCGC (adjusted OR 0.30, 95% CI 0.11–0.87 for the highest vs. lowest category; OR 0.53, 95% CI 0.34–0.84 per 1-SD increase) (Table 1). Among EPIC women, C-peptide was positively associated with NCGC (adjusted OR 3.84, 95% CI 1.02–14.43 for the highest vs. lowest category and OR 2.17, 95% CI 1.19–3.97 per 1-SD increase) (Table 2); however, there were no other associations with CGC or NCGC. Furthermore, in sex-combined analyses (Supplementary table 5), we found IGFBP-3 and ghrelin were inversely associated with NCGC in EPIC (adjusted OR 0.70, 95% CI 0.51–0.95 and OR 0.66, 95% CI 0.49–0.89 per 1-SD increase, respectively), while leptin was positively associated with NCGC (adjusted OR 1.60, 95% CI 1.06–2.42 per 1-SD increase).
In ATBC, there were no associations between circulating hormones and CGC (Table 3). For NCGC, inverse associations were observed with ghrelin, which is consistent with the findings in EPIC, and insulin (per 1-SD increase: adjusted OR 0.22, 95% CI 0.10–0.50 and OR 0.45, 95% CI 0.22–0.91, respectively) (Table 3). There were no associations for any of the sex hormones in relation to CGC or NCGC in ATBC. Furthermore, in ATBC, sensitivity analyses found no significant difference in the association for those exposures that overlapped with the previous case–control study [19] and those that did not (data not shown).
In pooled analyses of data from men in EPIC and ATBC (Table 4), we found an inverse association between DHEA and CGC (adjusted OR 0.45, 95% CI 0.21–0.95 for the highest vs. lowest category). In addition, ghrelin was inversely associated with NCGC (adjusted OR 0.14, 95% CI 0.05–0.41 for the highest vs. lowest category and OR 0.27, 95% CI 0.16–0.47 per 1-SD increase).
In the UK-Biobank, SHBG was positively associated with CGC in men (adjusted HR 1.90, 95% CI 1.04–3.47 for the highest vs. lowest category, and HR 1.29, 95% CI 1.02–1.64 per 1-SD increase) (Table 5). For NCGC, an inverse association was observed with free testosterone in men in continuous data only (per 1-SD increase: adjusted HR 0.71, 95% CI 0.57–0.89). In UK-Biobank women, similar to EPIC men, a positive association was observed between IGF-1 and CGC (adjusted HR 5.13, 95% CI 1.26–20.88 for the highest vs. lowest category and HR 1.76, 95% CI 1.08–2.88 per 1-SD increase) (Table 6). For hormones without sex differences, no significant associations were observed in sex-combined analyses (Supplementary table 6).
In EPIC, we found strong to moderate correlations between androstenedione and DHEA (0.71), estrone and estradiol (0.76), testosterone and estradiol (0.79) and, as expected, between testosterone and free testosterone (0.99), and estradiol and free estradiol (0.99) (Supplementary table 7). Similar correlations were observed between sex hormones in ATBC (Supplementary table 8). In UK-Biobank, the only strong correlation was between testosterone and free testosterone (0.79) (Supplementary table 9). In models mutually adjusted for (1) all of the gut/adipokines and (2) all of the sex hormones, the direction and magnitude of the associations described remained the same, with the exception of IGF-1 and CGC, and of leptin and NCGC in EPIC men, and C-peptide and NCGC in EPIC women, which attenuated and were no longer statistically significant.
Sensitivity analysis excluding CGC and NCGC cases diagnosed during the first year of follow-up did not substantially change the results (data not shown).
Discussion
In our analyses, IGF-1 was positively associated with CGC and NCGC in men in EPIC; similar findings were observed for IGF-1 and CGC in women in UK-Biobank, although there was no association in ATBC. In EPIC, leptin was positively associated with NCGC in men, while C-peptide was positively associated with NCGC in women. For ghrelin, we observed inverse associations for NCGC among men in EPIC and ATBC. In addition, insulin was inversely associated with NCGC in men in ATBC. With regard to sex hormones, DHEA was inversely associated with CGC in EPIC and ATBC men combined, and free testosterone was inversely associated with NCGC in men in UK-Biobank only. In contrast, SHBG was positively associated with CGC in UK-Biobank men only.
Results from previous nested case–control studies and a cohort study reported no association between IGF-1 and gastric cancer risk [12,13,14], although these studies did not examine the associations for CGC and NCGC separately. In our study, findings for IGF-1 were intriguing but inconsistent, with positive associations observed for both CGC and NCGC subsites in EPIC men but only for CGC among women in UK-Biobank, and no associations in ATBC. Experimental studies suggest IGF-1 may play a role in the development of gastric cancer [34, 35]. IGF-1 is thought to promote cancer development by stimulating cell proliferation and inhibiting apoptosis [34, 35].
Ghrelin was inversely associated with NCGC in men in EPIC and ATBC. Two previous nested case–control studies observed this same effect [19, 20]. Our results for ghrelin and NCGC in ATBC replicate findings of a previous ATBC study, which investigated the association between serum ghrelin concentration and risk of gastric non-cardia adenocarcinoma (n = 261 cases) and esophagogastric junctional adenocarcinoma (n = 98 cases) [19]. The potential mechanisms underlying an association between ghrelin and gastric cancer are unclear; however, a recent study found that ghrelin inhibits cell proliferation, migration, and invasion in gastric cancer cells [36]. Conversely, in another study, ghrelin induced cell proliferation, migration and invasion in gastric cancer cells [37]. For leptin, a satiety hormone, we observed a positive association with NCGC in EPIC men only. Case–control studies have reported lower serum leptin levels in gastric cancer patients compared to controls [18, 38] but these studies did not provide data on the association between leptin levels and gastric cancer risk and did not examine leptin and gastric cancer subsite. Mechanistically, leptin can stimulate cell proliferation in gastric cancer cells, which may contribute to cancer development [39].
Insulin was inversely associated with NCGC only in ATBC, whereas C-peptide was positively associated with NCGC in EPIC women. A prospective case–control study reported a positive association between insulin and early gastric cancer risk [40] but did not analyze by cancer subtype; although a nested case–control study showed a positive association between both C-peptide and insulin for NCGC but the risk estimates were not significant [10]. Regarding CGC, a large prospective cohort study (NIH-AARP Diet and Health study) has previously shown a positive association between self-reported diabetes and CGC [41] but there is little data on insulin and CGC [42]. The role of insulin in other malignancies was established with a meta-analysis reporting an increased risk for colorectal and pancreatic cancers with higher levels of insulin and C-peptide [43]. Despite the lack of epidemiological data, a recent in vitro study demonstrated that insulin exhibits direct cancer-promoting effects on gastric cancer cells [44].
For the sex hormones in our study, DHEA was inversely associated with CGC in men from EPIC and ATBC combined. A previous nested case–control study in men showed DHEA was associated with a 38% decreased risk of esophageal/gastric adenocarcinoma combined [24]; whilst a case–control study reported an inverse association between DHEA and NCGC in sex-combined analysis [45]. DHEA has been shown to have a protective role against cancer [46, 47]. Experimental studies have demonstrated that DHEA inhibits proliferation of cancer cells [46] and derivatives of DHEA exhibit anti-tumor activity against gastric cancer cells [47].
We also observed an inverse association between free testosterone and NCGC among men in UK-Biobank only, although a previous nested case–control study showed no association between testosterone and NCGC [25]. For SHBG, we observed a positive association with CGC among men in UK-Biobank only. A study nested within three US cohort studies showed no association between SHBG and esophageal and gastric adenocarcinoma combined [24], whilst a previous UK-Biobank study and a nested case–control study showed a positive association between SHBG concentrations and NCGC [25, 26]. Few studies have examined the association between free testosterone or SHBG with risk of CGC and NCGC. SHBG is a glycoprotein, which binds circulating androgens and estrogens and regulates the bioavailability of androgens and estrogens [48]. Estrogen can decrease cell viability and induce apoptosis in gastric cancer cells [49]. Additionally, polymorphisms in SHBG and catechol-O-methyltransferase, involved in estrogen inactivation, have been associated with gastric cancer risk [50].
Evidence from both experimental and observational studies suggest plausible mechanisms to explain observed associations between circulating hormones and gastric cancer risk. However, consistent with the fact that risk factor profiles differ by cancer subsite, some of the hormone associations also appear to vary by gastric cancer subsite.
Our study had many strengths, including its prospective design with serum samples and questionnaire data collected before cancer diagnosis, data available on potential confounders, and the opportunity to measure several hormones. Nevertheless, there are limitations in our study. Residual confounding may affect our data; in particular, we had no information on Helicobacter pylori infection, which is a well-known risk factor for NCGC. The enrollment years vary across the three studies, which could have influenced risk factor exposure: the changing prevalence of Helicobacter pylori infection over time [51], and the rise in obesity and its implication for CGC cancer [3]. In the ATBC study, participants were male smokers, which may limit the generalizability of findings from that study. Most importantly, despite using three large cohorts with long follow-up periods, the number of cases and controls in some analyses remained small; hence, our results should be interpreted with caution. Although we examined several variables, we did not adjust for multiple comparisons given that the analytes were selected a-priori, and each had specific proposed mechanisms through which they may be associated with gastric cancer. Finally, hormone levels were measured only at one time-point (baseline), which could lead to misclassification if hormone levels changed over the course of follow-up.
In conclusion, we found IGF-1 and SHBG were positively associated with CGC, while IGF-1, C-peptide and leptin were positively associated with NCGC. Furthermore, DHEA was inversely associated with CGC, whereas ghrelin and free testosterone were inversely associated with NCGC. Our findings suggest that some obesity-related hormones may influence CGC and NCGC risk. Further prospective studies with larger sample size are needed to examine endogenous hormones measurements in relation to gastric cancer risk by subsite.
Data availability
For information on how to submit an application for gaining access to EPIC data and/or biospecimens, please follow the instructions at http://epic.iarc.fr/access/index.php. The UK Biobank is an open access resource and bona fide researchers can apply to use the UK Biobank data set by registering and applying at http://ukbiobank.ac.uk/register-apply/. Further information is available from the corresponding author upon request.
Abbreviations
- ATBC:
-
Alpha-tocopherol, beta-carotene cancer prevention
- BMI:
-
Body mass index
- CGC:
-
Cardia gastric cancer
- CRP:
-
C-reactive protein
- CI:
-
Confidence intervals
- DHEA:
-
Dehydroepiandrosterone
- EPIC:
-
European Prospective Investigation into Cancer and Nutrition
- HR:
-
Hazard ratio
- HbA1c:
-
Glycated hemoglobin
- IGF-1:
-
Insulin-like growth factor 1
- IGFBP-3:
-
Insulin-like growth factor-binding protein 3
- NCGC:
-
Non-cardia gastric cancer
- OR:
-
Odds ratio
- SD:
-
Standard deviation
- SHBG:
-
Sex hormone-binding globulin
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. https://doi.org/10.3322/caac.21492.
Lauby-Secretan B, Scoccianti C, Loomis D, Grosse Y, Bianchini F, Straif K. Body fatness and cancer-viewpoint of the IARC Working Group. N Engl J Med. 2016;375(8):794–8. https://doi.org/10.1056/NEJMsr1606602.
Sanikini H, Muller DC, Sophiea M, Rinaldi S, Agudo A, Duell EJ, et al. Anthropometric and reproductive factors and risk of esophageal and gastric cancer by subtype and subsite: results from the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort. Int J Cancer. 2020;146(4):929–42. https://doi.org/10.1002/ijc.32386.
Sanikini H, Muller DC, Chadeau-Hyam M, Murphy N, Gunter MJ, Cross AJ. Anthropometry, body fat composition and reproductive factors and risk of oesophageal and gastric cancer by subtype and subsite in the UK Biobank cohort. PLoS ONE. 2020;15(10):e0240413. https://doi.org/10.1371/journal.pone.0240413.
Wang SM, Katki HA, Graubard BI, Kahle LL, Chaturvedi A, Matthews CE, et al. Population Attributable risks of subtypes of esophageal and gastric cancers in the United States. Am J Gastroenterol. 2021;116(9):1844–52. https://doi.org/10.14309/ajg.0000000000001355.
Rawla P, Barsouk A. Epidemiology of gastric cancer: global trends, risk factors and prevention. Prz Gastroenterol. 2019;14(1):26–38. https://doi.org/10.5114/pg.2018.80001.
Murphy N, Jenab M, Gunter MJ. Adiposity and gastrointestinal cancers: epidemiology, mechanisms and future directions. Nat Rev Gastroenterol Hepatol. 2018;15(11):659–70. https://doi.org/10.1038/s41575-018-0038-1.
Qaid MM, Abdelrahman MM. Role of insulin and other related hormones in energy metabolism—a review. Cogent Food Agric. 2016;2(1):1267691. https://doi.org/10.1080/23311932.2016.1267691.
Jones AG, Hattersley AT. The clinical utility of C-peptide measurement in the care of patients with diabetes. Diabet Med. 2013;30(7):803–17. https://doi.org/10.1111/dme.12159.
Hidaka A, Sasazuki S, Goto A, Sawada N, Shimazu T, Yamaji T, et al. Plasma insulin, C-peptide and blood glucose and the risk of gastric cancer: the Japan Public Health Center-based prospective study. Int J Cancer. 2015;136(6):1402–10. https://doi.org/10.1002/ijc.29098.
Samani AA, Yakar S, LeRoith D, Brodt P. The role of the IGF system in cancer growth and metastasis: overview and recent insights. Endocr Rev. 2007;28(1):20–47. https://doi.org/10.1210/er.2006-0001.
Pham TM, Fujino Y, Kikuchi S, Tamakoshi A, Yatsuya H, Matsuda S, et al. A nested case-control study of stomach cancer and serum insulin-like growth factor (IGF)-1, IGF-2 and IGF-binding protein (IGFBP)-3. Eur J Cancer (Oxford, England : 1990). 2007;43(10):1611–6. https://doi.org/10.1016/j.ejca.2007.04.014.
Yatsuya H, Toyoshima H, Tamakoshi K, Tamakoshi A, Kondo T, Hayakawa N, et al. Serum levels of insulin-like growth factor I, II, and binding protein 3, transforming growth factor beta-1, soluble fas ligand and superoxide dismutase activity in stomach cancer cases and their controls in the JACC Study. J Epidemiol. 2005;15(Suppl 2):S120–5. https://doi.org/10.2188/jea.15.s120.
Qian F, Huo D. Circulating insulin-like growth factor-1 and risk of total and 19 site-specific cancers: cohort study analyses from the UK biobank. Cancer Epidemiol Biomark Prev. 2020;29(11):2332–42. https://doi.org/10.1158/1055-9965.Epi-20-0743.
Nigro E, Scudiero O, Monaco ML, Palmieri A, Mazzarella G, Costagliola C, et al. New insight into adiponectin role in obesity and obesity-related diseases. BioMed Res Int. 2014;2014:658913. https://doi.org/10.1155/2014/658913.
Klok MD, Jakobsdottir S, Drent ML. The role of leptin and ghrelin in the regulation of food intake and body weight in humans: a review. Obes Rev. 2007;8(1):21–34. https://doi.org/10.1111/j.1467-789X.2006.00270.x.
Ishikawa M, Kitayama J, Kazama S, Hiramatsu T, Hatano K, Nagawa H. Plasma adiponectin and gastric cancer. Clin Cancer Res. 2005;11(2 Pt 1):466–72.
Tas F, Karabulut S, Erturk K, Duranyildiz D. Clinical significance of serum leptin level in patients with gastric cancer. Eur Cytokine Netw. 2018;29(2):52–8. https://doi.org/10.1684/ecn.2018.0408.
Murphy G, Kamangar F, Dawsey SM, Stanczyk FZ, Weinstein SJ, Taylor PR, et al. The relationship between serum ghrelin and the risk of gastric and esophagogastric junctional adenocarcinomas. J Natl Cancer Inst. 2011;103(14):1123–9. https://doi.org/10.1093/jnci/djr194.
Pritchett NR, Maziarz M, Shu X-O, Kamangar F, Dawsey SM, Fan J-H, et al. Serum ghrelin and esophageal and gastric cancer in two cohorts in China. Int J Cancer. 2020;146(10):2728–35. https://doi.org/10.1002/ijc.32597.
Frank AP, de Souza SR, Palmer BF, Clegg DJ. Determinants of body fat distribution in humans may provide insight about obesity-related health risks. J Lipid Res. 2019;60(10):1710–9. https://doi.org/10.1194/jlr.R086975.
Green J, Roddam A, Pirie K, Kirichek O, Reeves G, Beral V. Reproductive factors and risk of oesophageal and gastric cancer in the Million Women Study cohort. Br J Cancer. 2012;106(1):210–6. https://doi.org/10.1038/bjc.2011.525.
Duell EJ, Travier N, Lujan-Barroso L, Boutron-Ruault MC, Clavel-Chapelon F, Palli D, et al. Menstrual and reproductive factors, exogenous hormone use, and gastric cancer risk in a cohort of women from the European Prospective Investigation Into Cancer and Nutrition. Am J Epidemiol. 2010;172(12):1384–93. https://doi.org/10.1093/aje/kwq321.
Petrick JL, Hyland PL, Caron P, Falk RT, Pfeiffer RM, Dawsey SM, et al. associations between prediagnostic concentrations of circulating sex steroid hormones and esophageal/gastric cardia adenocarcinoma among men. J Natl Cancer Inst. 2019;111(1):34–41. https://doi.org/10.1093/jnci/djy082.
Zhu Z, Chen Y, Ren J, Dawsey SM, Yin J, Freedman ND, et al. Serum levels of androgens, estrogens, and sex hormone binding globulin and risk of primary gastric cancer in chinese men: a nested case-control study. Cancer Prev Res (Phila). 2021;14(6):659–66. https://doi.org/10.1158/1940-6207.Capr-20-0497.
McMenamin ÚC, Liu P, Kunzmann AT, Cook MB, Coleman HG, Johnston BT, et al. Circulating sex hormones are associated with gastric and colorectal cancers but not esophageal adenocarcinoma in the UK biobank. Am J Gastroenterol. 2021;116(3):522–9. https://doi.org/10.14309/ajg.0000000000001045.
Riboli E, Hunt KJ, Slimani N, Ferrari P, Norat T, Fahey M, et al. European prospective investigation into cancer and nutrition (EPIC): study populations and data collection. Public Health Nutr. 2002;5(6b):1113–24. https://doi.org/10.1079/phn2002394.
The alpha-tocopherol, beta-carotene lung cancer prevention study: design, methods, participant characteristics, and compliance. The ATBC Cancer Prevention Study Group. Ann Epidemiol. 1994;4(1):1–10. https://doi.org/10.1016/1047-2797(94)90036-1
Sudlow C, Gallacher J, Allen N, Beral V, Burton P, Danesh J, et al. UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 2015;12(3):e1001779. https://doi.org/10.1371/journal.pmed.1001779.
Keski-Rahkonen P, Desai R, Jimenez M, Harwood DT, Handelsman DJ. Measurement of estradiol in human serum by LC-MS/MS using a novel estrogen-specific derivatization reagent. Anal Chem. 2015;87(14):7180–6. https://doi.org/10.1021/acs.analchem.5b01042.
Rinaldi S, Geay A, Déchaud H, Biessy C, Zeleniuch-Jacquotte A, Akhmedkhanov A, et al. Validity of free testosterone and free estradiol determinations in serum samples from postmenopausal women by theoretical calculations. Cancer Epidemiol Biomark Prev. 2002;11(10 Pt 1):1065–71.
Biobank U. UK Biobank Biomarker Project - Companion Document to Accompany Serum Biomarker Data. Prepared for: UK Biobank Showcase. 2019.
Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002;420(6917):860–7. https://doi.org/10.1038/nature01322.
Pavelić K, Kolak T, Kapitanović S, Radošević S, Spaventi Š, Krušlin B, et al. Gastric cancer: the role of insulin-like growth factor 2 (IGF 2) and its receptors (IGF 1R and M6-P/IGF 2R). J Pathol. 2003;201(3):430–8. https://doi.org/10.1002/path.1465.
Kang BW, Chau I. Molecular target: pan-AKT in gastric cancer. ESMO Open. 2020;5(5):e000728. https://doi.org/10.1136/esmoopen-2020-000728.
Hu XL, Zhu YJ, Hu CH, You L, Wu J, He XY, et al. Ghrelin affects gastric cancer progression by activating AMPK signaling pathway. Biochem Genet. 2021;59(3):652–67. https://doi.org/10.1007/s10528-020-10022-x.
Tian C, Zhang L, Hu D, Ji J. Ghrelin induces gastric cancer cell proliferation, migration, and invasion through GHS-R/NF-κB signaling pathway. Mol Cell Biochem. 2013;382(1–2):163–72. https://doi.org/10.1007/s11010-013-1731-6.
Begenik H, Aslan M, Dulger AC, Emre H, Kemik A, Kemik O, et al. Serum leptin levels in gastric cancer patients and the relationship with insulin resistance. Arch Med Sci. 2015;11(2):346–52. https://doi.org/10.5114/aoms.2015.50967.
Lee KN, Choi HS, Yang SY, Park HK, Lee YY, Lee OY, et al. The role of leptin in gastric cancer: clinicopathologic features and molecular mechanisms. Biochem Biophys Res Commun. 2014;446(4):822–9. https://doi.org/10.1016/j.bbrc.2014.02.072.
Kwon HJ, Park MI, Park SJ, Moon W, Kim SE, Kim JH, et al. Insulin resistance is associated with early gastric cancer: a prospective multicenter case control study. Gut and liver. 2019;13(2):154–60. https://doi.org/10.5009/gnl17556.
Lin SW, Freedman ND, Hollenbeck AR, Schatzkin A, Abnet CC. Prospective study of self-reported diabetes and risk of upper gastrointestinal cancers. Cancer Epidemiol Biomark Prev. 2011;20(5):954–61. https://doi.org/10.1158/1055-9965.Epi-10-1244.
Choi YJ. Insulin resistance: a hidden risk factor for gastric cancer? Gut and liver. 2019;13(2):133–4. https://doi.org/10.5009/gnl19060.
Pisani P. Hyper-insulinaemia and cancer, meta-analyses of epidemiological studies. Arch Physiol Biochem. 2008;114(1):63–70. https://doi.org/10.1080/13813450801954451.
Saisana M, Griffin SM, May FEB. Insulin and the insulin receptor collaborate to promote human gastric cancer. Gastr Cancer. 2021. https://doi.org/10.1007/s10120-021-01236-y.
Leal YA, Song M, Zabaleta J, Medina-Escobedo G, Caron P, Lopez-Colombo A, et al. Circulating levels of sex steroid hormones and gastric cancer. Arch Med Res. 2021;52(6):660–4. https://doi.org/10.1016/j.arcmed.2021.03.001.
Liu L, Wang D, Li L, Ding X, Ma H. Dehydroepiandrosterone inhibits cell proliferation and improves viability by regulating S phase and mitochondrial permeability in primary rat Leydig cells. Mol Med Rep. 2016;14(1):705–14. https://doi.org/10.3892/mmr.2016.5343.
Ke S, Wei Y, Shi L, Yang Q, Yang Z. Synthesis of novel steroid derivatives derived from dehydroepiandrosterone as potential anticancer agents. Anticancer Agents Med Chem. 2013;13(8):1291–8. https://doi.org/10.2174/18715206113139990323.
Rosner W, Hryb DJ, Khan MS, Nakhla AM, Romas NA. Sex hormone-binding globulin: anatomy and physiology of a new regulatory system. J Steroid Biochem Mol Biol. 1991;40(4–6):813–20. https://doi.org/10.1016/0960-0760(91)90307-q.
Qin J, Liu M, Ding Q, Ji X, Hao Y, Wu X, et al. The direct effect of estrogen on cell viability and apoptosis in human gastric cancer cells. Mol Cell Biochem. 2014;395(1):99–107. https://doi.org/10.1007/s11010-014-2115-2.
Freedman ND, Ahn J, Hou L, Lissowska J, Zatonski W, Yeager M, et al. Polymorphisms in estrogen- and androgen-metabolizing genes and the risk of gastric cancer. Carcinogenesis. 2009;30(1):71–7. https://doi.org/10.1093/carcin/bgn258.
Vyse AJ, Gay NJ, Hesketh LM, Andrews NJ, Marshall B, Thomas HI, et al. The burden of Helicobacter pylori infection in England and Wales. Epidemiol Infect. 2002;128(3):411–7. https://doi.org/10.1017/s0950268802006970.
Acknowledgements
Coordination of EPIC is financially supported by International Agency for Research on Cancer (IARC) and by the Department of Epidemiology and Biostatistics, School of Public Health, Imperial College London, with infrastructure support provided by the NIHR Imperial Biomedical Research Centre (BRC). National cohorts are supported by: Danish Cancer Society (Denmark); Ligue Contre le Cancer, Institut Gustave Roussy, Mutuelle Générale de l’Education Nationale, Institut National de la Santé et de la Recherche Médicale (INSERM) (France); German Cancer Aid, German Cancer Research Center (DKFZ), German Institute of Human Nutrition Potsdam-Rehbruecke (DIfE), Federal Ministry of Education and Research (BMBF) (Germany); Associazione Italiana per la Ricerca sul Cancro-AIRC-Italy, Compagnia di SanPaolo and National Research Council (Italy); Dutch Ministry of Public Health, Welfare and Sports (VWS), Netherlands Cancer Registry (NKR), LK Research Funds, Dutch Prevention Funds, Dutch ZON (Zorg Onderzoek Nederland), World Cancer Research Fund (WCRF), Statistics Netherlands (The Netherlands); Health Research Fund (FIS)—Instituto de Salud Carlos III (ISCIII), Regional Governments of Andalucía, Asturias, Basque Country, Murcia and Navarra, and the Catalan Institute of Oncology—ICO (Spain); Swedish Cancer Society, Swedish Research Council and County Councils of Skåne and Västerbotten (Sweden); Cancer Research UK (14136 to EPIC-Norfolk; C8221/A29017 to EPIC-Oxford), Medical Research Council (1000143 to EPIC-Norfolk; MR/M012190/1 to EPIC-Oxford) (United Kingdom). The ATBC Study is supported by the Intramural Research Program of the U.S. National Cancer Institute, National Institutes of Health (NIH), Department of Health and Human Services.
Funding
Research was funded by the Stand Up to Cancer campaign for Cancer Research UK; award number: C53889/A20189.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have any conflicts of interest to disclose.
Ethics statement
All participants provided written informed consent. Ethical approval of the EPIC cohort study was obtained from the ethical review committees of the IARC and EPIC centers. The ATBC study was approved by the Institutional Review Boards of both the NIH in the United States and the National Public Health Institutes in Finland. The UK Biobank cohort study was approved by Northwest Multi-center Research Ethics Committee, the National Information Governance Board for Health and Social Care in England and Wales, and the Community Health Index Advisory Group in Scotland.
Disclaimer
Where authors are identified as personnel of the IARC/World Health Organization, the authors alone are responsible for the views expressed in this article and they do not necessarily represent the decisions, policy or views of the IARC/World Health Organization.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sanikini, H., Biessy, C., Rinaldi, S. et al. Circulating hormones and risk of gastric cancer by subsite in three cohort studies. Gastric Cancer 26, 969–987 (2023). https://doi.org/10.1007/s10120-023-01414-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10120-023-01414-0