Abstract
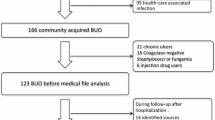
A total of 118 patients with Elizabethkingia meningoseptica bacteremia at a medical center in Taiwan from 1999 to 2006 were studied. Minimum inhibitory concentrations (MICs) of 99 preserved isolates were determined. The incidence (per 100,000 admissions) of E. meningoseptica bacteremia increased from 7.5 in 1996 to 35.6 in 2006 (p = 0.006). Among them, 84% presented with fever, 86% had nosocomial infections, and 60% had acquired the infection in intensive care units (ICUs). The most common underlying diseases were malignancy (36%) and diabetes mellitus (25%). Seventy-eight percent of patients had primary bacteremia, followed by pneumonia (9%), soft tissue infection, and catheter-related bacteremia (6%). Forty-five patients (38%) had polymicrobial bacteremia. Overall, the 14-day mortality was 23.4%. Multivariate analysis revealed E. meningoseptica bacteremia acquired in an ICU (p = 0.048, odds ratio [OR] 4.23) and presence of effective antibiotic treatment after the availability of culture results (p = 0.049, OR 0.31) were independent predictors of 14-day mortality. The 14-day mortality was higher among patients receiving carbapenems (p = 0.046) than fluoroquinolones or other antimicrobial agents. More than 80% of the isolates tested were susceptible to trimethoprim-sulfamethoxzole, moxifloxacin, and levofloxacin. The MIC50 and MIC90 of the isolates to tigecycline and doxycycline were both 4 μg/mL and 8 μg/ml, respectively.

Similar content being viewed by others
References
Vandamme P, Bernardet JF, Segers P et al (1994) New perspectives in the classification of the flavobacteria: description of Chryseobacterium gen. nov., Bergeyella gen. nov., and Empedobacter nom. Rev. Int J Syst Bacteriol 44:827–831
Schreckenberger PC (2003) Acinetobacter, Achromobacter, Chryseobacterium, Moraxella, and other nonfermentative gram-negative rods. In: Murray PR, Baron EJ, Jorgensen JH, Pfaller MA, Yolken RH (eds) Manual of clinical microbiology, 8th edn. American Society for Microbiology, Washington, DC, pp 749–779
Kim KK, Kim MK, Lim JH (2005) Transfer of Chryseobacterium meningosepticum and Chryseobacterium miricola to Elizabethkingia gen. nov. as Elizabethkingia meningoseptica comb. nov. and Elizabethkingia miricola comb. nov. Int J Syst Evol Microbiol 55:1287–1293
Gungor S, Ozen M, Akinci A et al (2003) A Chryseobacterium menigosepticum outbreak in a neonatal ward. Infect Control Hosp Epidemiol 24:613–617
Tekerekoglu MS, Durnaz R, Ayan M et al (2003) Analysis of an outbreak due to Chryseobacterium meningosepticum in a neonatal intensive care unit. New Microbiol 26:57–63
Spangler SK, Visalli MA, Jacobs MR et al (1996) Susceptibilities of non-Pseudomonas aeruginosa gram-negative nonfermentative rods to ciprofloxacin, ofloxacin, levofloxacin, D-ofloxacin, sparfloxacin, ceftazidime, piperacillin, piperacillin-tazobactam, trimethoprim-sulfamethoxazole, and imipenem. Anitmicrob Agents Chemother 40:772–775
Fraser SL, Jorgensen JH (1997) Reappraisal of the antimicrobial susceptibilities of Chryseobacterium and Flavobacterium species and methods for reliable susceptibility testing. Anitmicrob Agents Chemother 41:2738–2741
Yabuuchi E, Kaneko T, Yano I et al (1983) Sphingobacterieum gen. nov., Sphingobacterium spiritivorum comb. nov., Sphingobacterium mizutae sp. nov., and Flavobacterium indologenes sp. nov.: glucose-nonfermenting, gram-negative rods in CDC group like-2 and IIb. Int J Syst Bacteriol 33:580–598
Clinical and Laboratory Standards Institute (2010) Performance standards for antimicrobial susceptibility testing; twentieth informational supplement. M100-S20. CLSI, Wayne, PA, USA, 2010
Garner JS, Jarvis WR, Emori TG et al (1988) CDC definition for nosocomial infections, 1988. Am J Infect Control 16:128–140
Liao CH, Sheng WH, Chen YC et al (2007) Predictive value of the serum bactericidal test for mortality in patients infected with multidrug-resistant Acinetobacter baumannii. J Infect 55:149–157
Carmeli Y, Akova M, Cornaglia G et al (2010) Controlling the spread of carbapenemase-producing Gram-negatives: therapeutic approach and infection control. Clin Microbiol Infect 16:102–111
Sader HS, Jones RN (2005) Antimicrobial susceptibility of uncommonly isolated non-enteric Gram-negative bacilli. Int J Antimicrob Agents 25:95–109
Kirby JT, Sader HS, Walsh TR et al (2004) Antimicrobial susceptibility and epidemiology of a worldwide collection of Chryseobacterium spp report from the SENTRY Antimicrobial Surveillance Program (1997–2001). J Clin Microbiol 42:445–448
Chiu CH, Waddingdon M, Hsieh WS et al (2000) Atypical Chryseobacterium meningosepticum and meningitis and sepsis in newborns and the immunocompromised, Taiwan. Emerg Infect Dis 6:481–486
Bloch KC, Nadarajah R, Jacobs R (1997) Chryseobacterium meningoseptiucm: an emerging pathogen among immunocompromised adults. Medicine 76:30–41
Lin PY, Chu C, Su LH et al (2004) Clinical and microbiological analysis of bloodstream infections caused by Chryseobacterium meningosepticum in nonneonatal patients. J Clin Microbiol 42:3353–3355
Fujita J, Hata Y, Irino S (1990) Respiratory infection caused by Flaveobacterium meningosepticum. Lancet 335:544
Hirsh BE, Wong B, Kiehn TE et al (1989) Flavobacterium meningoseptiucm bacteremia in an adult with acute leukemia. Use of rifampin to clear persistent infection. Diagn Microbiol Infect Dis 4:65–69
Hung PP, Lin YH, Lin CF et al (2008) Chryseobacterium meningosepticum infection: antibiotic susceptibility and risk factors for mortality. J Microbiol Immunol Infect 41:137–144
Pokrywka M, Viazanko K, Medvick J et al (1993) A Flavobacterium meningosepticum outbreak among intensive care patients. Am J Infect Control 21:139–145
Lin YT, Chan YJ, Chiu CH et al (2009) Tigecycline and colistin susceptibility of Chryseobacterium meningsepticum isolated from blood in Taiwan. Int J Antimicrob Agents 34:99–102
Wisplinghoff H, Bischoff T, Tallent SM et al (2004) Nosocomial bloodstream infections in US hospitals: analysis of 24,179 cases from a prospective nationwide surveillance study. Clin Infect Dis 39:309–317
Giamarellos-Bourboulis EJ, Karnesis L, Galani I et al (2002) In vitro killing effect of moxifloxacin on clinical isolates of Stenotrophomonas maltophilia resistant to trimethoprim-sulfamethoxazole. Antimicrob Agents Chemother 46:3997–3999
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hsu, MS., Liao, CH., Huang, YT. et al. Clinical features, antimicrobial susceptibilities, and outcomes of Elizabethkingia meningoseptica (Chryseobacterium meningosepticum) bacteremia at a medical center in Taiwan, 1999–2006. Eur J Clin Microbiol Infect Dis 30, 1271–1278 (2011). https://doi.org/10.1007/s10096-011-1223-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-011-1223-0