Abstract
Background
Infections caused by extended spectrum β-lactamase (ESβL) producing bacteria are common and problematic. When they cause bloodstream infections, they are associated with significant morbidity and mortality.
Methods
A retrospective cross-sectional observational study was conducted in a single center in Pereira, Colombia. It included people hospitalized with bacteremia due to gram-negative bacilli with the extended-spectrum β-lactamase producing phenotype. A logistic regression analysis was constructed. Clinical characteristics and risk factors for death from sepsis were established.
Results
The prevalence of bacteremia due to Enterobacterales with extended-spectrum β-lactamase producing phenotype was 17%. 110 patients were analyzed. Most patients were men (62%) with a median age of 58 years, hospital mortality was 38%. Admission to intensive care was 45%. The following risk factors for mortality were established: shock requiring vasoactive support, Pitt score > 3 points, and not having an infectious disease consultation (IDC).
Conclusions
bacteremia due to Enterobacterales with extended-spectrum β-lactamase producing phenotype have a high mortality. Early recognition of sepsis, identification of risk factors for antimicrobial resistance, and prompt initiation of appropriate empiric antibiotic treatment are important. An infectious disease consultation may help improve outcomes.
Similar content being viewed by others
Background
Resistance in gram-negative bacteria has gained great importance in recent decades and one of the reasons is the increase in extended-spectrum β-lactamase-producing bacteria (ESβL) as a growing problem throughout the world [1,2,3,4]. ESβL are β-lactamases that can hydrolyze penicillins and cephalosporins [5]. High prevalence rates of ESβL-producing Enterobacterales (ESβL-E) have been reported in Escherichia coli and Klebsiella pneumoniae [6].
The prevalence of ESβL-producing K. pneumoniae and E. coli have steadily increased over the last decades. ESβL expression by Enterobacterales in Latin American hospitals became endemic since 1990 [7]. In 2002, CTX-M-12 from a strain of K. pneumoniae was detected in Colombia, representing the first description of a CTX-M in our country [8]. Currently, hospitals in Latin America face the problem of high infection rates by ESβL-producing Enterobacterales. It is important to note that ESβL-E infections are associated with higher mortality (up to 70%) compared to patients with bacterial infections without production of ESβL-E [9]. Patients have a survival advantage when the correct antimicrobial agent is chosen as initial therapy [7].
The aim of the study was to describe the clinical characteristics of hospitalized patients with ESβL-E bacteremia. This was a single center study, developed at the Hospital Universitario San Jorge, from the city of Pereira, in Colombia. Pereira is one of the main cities of the coffee region, with a population of more than 500,000 inhabitants.
Methods
Study design and data collection
This was a retrospective, cross-sectional, observational study conducted at the Hospital Universitario San Jorge de Pereira, Colombia, a tertiary referral center with more than 300 beds, located in the city of Pereira, Colombia. The study was approved by the Ethics Committee of the Universidad Tecnológica de Pereira. The study period was from January 2012 to December 2017. All patients with ESβL-E bacteremia were included. Those patients with incomplete clinical records or those who did not die from sepsis were excluded. Electronic medical records were reviewed. Data on the clinical characteristics of the patients, comorbidities, symptoms, and laboratory tests at hospital admission were collected. A logistic regression analysis was constructed. Risk factors for sepsis mortality were established.
Definitions
Hospital-acquired bacteremia was considered if the blood culture (BC) sample was taken 48 h after hospital admission [10]. The criteria of Friedman et al. were used to determine which infections were healthcare associated [11]. Infections acquired in the community were considered when the first positive culture was obtained < 48 h from the patient's admission to the hospital [12]. Primary bacteremia was defined as bacteremia for which no source of infection was documented [12]. Secondary bacteremia was considered when a source of infection was found, at the same time or up to 3 days before the bacteremia [12]. The source of the bacteremia was confirmed by the clinical characteristics of each patient, the clinical evaluation performed by the physician, and the reports of cultures taken from other anatomic sites. Catheter related bloodstream infection (CRBSI) was defined based on the positivity time of the BCs obtained at the same time, one from the catheter and the other from peripheral venipuncture, processed in a continuous monitoring system. If both BCs grow the same organism and the BC drawn from the device becomes positive > 2 h before the BC drawn by venipuncture, CRBSI was considered [13].
Febrile neutropenia was considered when the neutrophil count was < 500 cells/mm3 [14]. The Charlson comorbidity index was used to assess the impact of comorbidities in the study population. Sepsis and septic shock were defined according to The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) [15]. Mortality was defined as inpatient death due to bacterial sepsis. Only mortality attributed to sepsis was taken into account. Complete medical records were reviewed to establish the cause of death. All patients with septic shock and/or acute respiratory failure were considered for admission to critical care.
Empiric antibiotic therapy consisted of antibiotics administered within 24 h of identifying a case of bacterial sepsis. Definitive therapy was defined as antibiotics instituted after the results of the blood culture and antibiogram were known. Empirical treatment was considered adequate when a carbapenem was administered, any other β-lactam antibiotic was considered inappropriate regardless of in vitro susceptibility. The dose, frequency, and route of antibiotics were not taken into account when assessing suitability. All study definitions were established prior to data analysis.
Laboratory methods
The samples analyzed included blood, urine, and respiratory tract samples (sputum expectorated by the patient or orotracheal tube aspirate). The detection of ESβL was performed by an automated method. The Vitek 2 system (bioMérieux SA) was used. All isolates showed sensitivity to carbapenems according to the CLSI (Clinical & Laboratory Standards Institute) cut-off points for each year.
Collection and processing of blood samples
The volume of blood that was obtained, for adults, was 20–30 mL of blood per culture set, > 2 culture bottles were used. For neonates and adolescents, an age- and weight- appropriate volume of blood was cultured according to guidelines [13]. Inoculated blood culture bottles were incubated at 37 °C and inspected for 5 consecutive days [16]. Blood cultures that showed signs of bacterial growth were subcultured on blood agar and MacConkey agar [16]. Agar plates were incubated at 37 °C for 48 h. Gram-negative rod colonies were pre-identified by their colony appearance and morphology on Gram stain [16]. All isolates were confirmed by the automated Vitek2 system (Biomerieux, France).
Laboratory tests included complete blood count, liver function tests, renal function tests, urinalysis, urine gram stain, urine culture. Chest X-rays, computed tomography (CT) of the chest, and CT of the abdomen were performed when deemed necessary.
Statistic analysis
Descriptive statistics were calculated. Normality was assessed using the Kolmogorov Smirnov test or the Shapiro Wilk test when appropriate. For the continuous variables, the assumptions of normality were verified and for those that met them, Student’s t tests were performed. Nonparametric tests were used for those that did not meet the assumptions of normality (Wilcoxon or Man Whitney U). Continuous variables were presented as mean ± standard deviation or as medians and interquartile ranges (IQRs) when appropriate. Categorical variables were presented as frequency and percentage. Categorical variables were analyzed using the Chi-square test or Fisher’s exact test when appropriate. Variables with a p value < 0.1 on bivariate analysis were then entered into a logistic regression model to identify risk factors for death from sepsis. A stepwise logistic regression was constructed. A value of p < 0.05 was considered as the cut-off point for statistical significance. The odds ratio was calculated with 95% confidence intervals.
The Hosmer and Lemeshow test was used to verify compliance with the necessary assumptions for the implementation of logistic regression, a value of p > 0.005 was considered a good fit.
IBM SPSS Statistics version 20 software was used for all statistical analyses.
Results
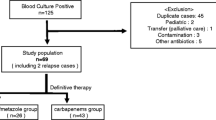
110 patients were included. Figure 1 shows the flowchart for patient selection. The median age was 58 years, with an interquartile range (IQR) of 35 to 73, only 14 patients were < 18 years old, 62% (n = 69) were men, and 40% (n = 45) were from rural areas. Hospital mortality was 38% (n = 42). The most frequent comorbidities were high blood pressure (48%), cancer (28%), type 2 diabetes mellitus (24%) and chronic obstructive pulmonary disease (COPD) (19%). See Table 1.
Primary bacteremias were 11%, CRBSI were 10%, and secondary bacteremias were 78%. The most common source of infection in secondary bacteremia was abdominal sepsis in 34% (due to peritonitis in 5 patients and cholangitis in 25 patients), urinary tract infection in 29%, pneumonia in 20%, and febrile neutropenia in 14%. Urinary tract infection was more common in the surviving group of patients (37% vs 16%, p = 0.02). Death was more common when the source of infection was not from a urinary tract infection (75% vs 55%, p = 0.04). Bladder catheterization was very common (41%) and the prevalence of biliary stents was 19%.
The population served was quite ill. The Charlson comorbidity index had a median of 4 points (IQR of 2–6 points). Admission to critical care was high (45%) and ventilatory support was provided in 37%. In the population that survived a Pitt score of 0–1 points was found more frequently compared to the group that died of sepsis (48% vs 23%, p = 0.01), on the other hand, a Pitt score > 3 points was more common in the group that died from sepsis (45% vs 13%, p = 0.001). There was no difference between the groups in the abnormal qSOFA scale (> 1 point). See Table 1.
The hospital stay was prolonged (median 26 days, IQR 13–46), also, the days of stay in intensive care were prolonged (median 8 days, IQR 3–20). The creatinine value at admission was 0.8 mg (IQR 0.6–1.2), 40% developed acute kidney injury. There was no difference between groups in the incidence of acute kidney injury. There were also no differences between groups in lactate levels.
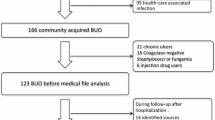
Antibiotic treatment
Most patients received empirical treatment. There were 6 patients (5.4%) who did not receive empirical antibiotic treatment. Empirical treatment was appropriate in 42% (n = 44/104). The remaining 60% (n = 66/110) of the population were amenable to carbapenem treatment (appropriate treatment) when culture results (susceptibility testing) were available. There were no differences between groups in the proportion of patients who received empirical treatment (95% vs 92%, p = 0.6), nor in the adequacy of treatment (whether or not they received a carbapenem) (41% vs 43%, p = 0.8). The most empirically used non-carbapenem β-lactam antibiotics were piperacillin tazobactam (27%), cefepime (13%) and ampicillin-sulbactam (11%). See Table 1. The median number of days from recognition of sepsis to death from sepsis was 3 days (IQR 1–8). About 52% of deaths occurred in the first 3 days from recognition of sepsis. Empirical treatment was given for a median of 3 days (IQR 2–5 days). See Fig. 2. Death was less common in those who completed > 7 days of carbapenem treatment.
Targeted therapy (based on the result of the antibiogram) was possible in 77% of patients (n = 51/66) who were amenable to carbapenem treatment when the antibiogram was finally known.
When the results of blood cultures with antibiograms were known, it was more common to receive antibiotic treatment with a carbapenem in the group of patients who survived compared to the group who died of sepsis (95% vs 48%, p = 0.001, OR 0.04, 95% CI 0.01–0.24). This finding firstly suggested a case of therapeutic inertia for antibiotic prescription based on the interpretative reading of the antibiogram. However, the data show that in the group of patients who died from sepsis (n = 42/110), 59.5% (n = 25/42) of the patients did not receive empirical carbapenem treatment (appropriate treatment) and 48% (n = 12/25) of them died in the first 72 h from the recognition of sepsis, therefore, doctors did not get to know the results of blood cultures while the patients were still alive. Figure 2 shows how most deaths occurred in the first 3 days after recognition of sepsis.
70% (n = 77/110) of the patients did not receive an infectious disease consultation (IDC). Absence of IDC was more common in the group that died from sepsis compared with those that survived (85% vs 60%, P = 0.005, OR 3.9, 95% CI 1.4–10.6). Follow-up blood cultures (FUBC) were taken in 23 patients (21%), 34% (n = 8/23) showed persistent bacterial growth.
Klebsiella pneumoniae was identified in 51% and Escherichia coli in 49%. The minimum inhibitory concentration (MIC) of ciprofloxacin had a median of 4 µg/mL (IQR 4–4), the MIC of gentamicin had a median of 1 µg/mL (IQR 1–16), and the MIC of amikacin had a median 3 µg/mL (IQR 2–8). No Clostridium difficile infection was diagnosed, but this was not routinely screened for in the patients.
On the use of piperacillin tazobactam
The MIC of piperacillin-tazobactam had a median of 16 µg/mL (IQR 8–64), mean of 42 µg/mL. 27.8% (n = 29/104) of the patients had empirical treatment with Piperacillin tazobactam, later 75% (n = 22/29) were escalated to carbapenems when the results of the blood cultures were known, 20.6% (n = 6/29) died in the first 72 h, before knowing the result of the antibiogram. The mortality of the group that received piperacillin tazobactam as empirical treatment was 37.9% (n = 11/29).
Logistic regression
The stepwise logistic regression analysis showed that the variables associated with death from sepsis are a Pitt score > 3 points, a state of septic shock requiring vasoactive support and not received an IDC. See Table 2.
Discussion
The present study described the clinical characteristics and risk factors for death from ESβL-E bloodstream infections (BSI). The population was quite morbid, we found high rates of admission to critical care, presence of renal failure at admission, and requirement of ventilatory support. The mortality in our study was very high. Many scientific publications have reported different levels of mortality in BSI caused by ESβL-E. In most reports, mortality is high, but with a wide range, for example, Lim et al. reported a 20% mortality [10] but, Namikawa et al. reported a 9.7% mortality [17], Scheuerman et al. reported an ESβL-producing K. pneumoniae BSI mortality of 33% and, an ESβL-producing E. coli BSI mortality of 17% [18], also, Tuon et al. reported a mortality from ESβL-producing K. pneumoniae of 49% [19]. The enormous heterogeneity that exists between the characteristics of the population of each mortality report may explains this notable variation in mortality from ESβL.
In considering the explanation of the high mortality found, we found no differences in mortality due to sepsis regarding the source of infection (primary bacteremia, secondary bacteremia, or CRBSI), the qSOFA, the initial lactate value and, the Charlson score. We found no differences between groups regarding the empirical administration of treatment with a carbapenem (41% vs 43%, p = 0.8), data similar to those shown by Lim et al. [10], who also analyzed the impact of empiric treatment in similar infections. In our cohort, there is a mortality peak in the first 3 days after recognition of sepsis (see Fig. 2). We observed that a high percentage of patients did not receive treatment based on the antibiogram. This was mainly observed in patients who died within the first 3 days from recognition of sepsis. These results would favor the use of rapid molecular diagnostic tests based on positive blood cultures to strengthen the appropriate prescription of antibiotics in bacteremia [20]. However, the population that died was more severely ill and probably benefited more from received empiric carbapenem therapy since initial evaluation. This is evidence of a poor perception of the risk of ESβL-E infection by clinicians when prescribing empirical antibiotic treatment.
In our cohort there was a high prevalence of risk factors for healthcare-associated infections and the group that died due to sepsis was more compromised in their health status: they were most commonly affected by septic shock, they had higher admission to critical care, they had higher requirement of ventilatory support and they had higher Pitt bacteremia score; therefore, based on current recommendations [21, 22], these patients should have received a higher proportion of treatment with carbapenems, however only 43% of this group received it. Similar findings were reported by Tuon et al., where the authors found that only 52% received adequate treatment within 48 h of bacteremia [19].
An IDC may play a role that can impact the outcome of mortality. This finding has been shown in bacteremia due to Staphylococcus aureus [23] and now we observe it in ESβL-E bacteremia (see Fig. 2). In the case S. aureus bacteremia, in the study of Bai et al. [24], it was shown that patients who received an IDC were more likely to have an echocardiogram, FUBCs, receive appropriate empiric antibiotic treatment and, have a longer duration of antibiotic therapy. As we know, there is no evidence on the benefit of an echocardiography in Gram-negative bacterial bloodstream infection caused by ESβL-E. Echocardiogram should be performed for infections caused by the HACEK gram-negative bacteria, but those are very rare infections [25, 26].
One of the reasons why an IDC could reduce the in-hospital mortality due to sepsis is due to the appropriate selection of empiric antibiotic treatment from the moment sepsis was first suspected or recognized. In our study, 51% (n = 17/33) of the patients who had an IDC had appropriate empirical antibiotic treatment with carbapenems, compared to 35% (n = 27/71) in the group of patients that did not have an IDC; however, this difference did not reach statistical significance (P = 0.195, OR 0.57, 95% CI 0.25–1.33). For the period in which the study was carried out, our institution did not have restrictions on the use of carbapenems, it had an antimicrobial stewardship program under construction, but with poor administrative support and low human resources. There is enough evidence to support the importance and enormous impact that an Infectious Disease Service can have on the management of bloodstream infection [27], decreased mortality [28], lower healthcare costs and lower readmission rates [29].
In our study, FUBCs were taken in 21% of patients (n = 23) and 34% (n = 8/23) showed persistent bacterial growth. In the initial statistical analysis, it was observed that performing FUBCs behaved as a protective factor for the outcome of in-hospital mortality due to sepsis (OR 0.27, 95% CI 0.08–0.86, P = 0.021), however it did not reached statistical significance in logistic regression analysis. FUBCs appear to add little value in the management of gram-negative bacteremia [30], but recently, in a systematic review and meta-analysis by Thaden et al., it was found that positive FUBCs were associated with increased mortality in Gram-negative bacterial bloodstream infection relative to negative blood cultures (odds ratio, 2.27; 95% CI 1.54–3.34) [31].
Limitations
This study had several limitations. First, the results were obtained retrospectively from a single center which may limit the generalisability of the results, however our findings are in line with other reported analyses. Second, most of the clinical and laboratory variables were based on the first measurements performed on each patient at the time of the initial presentation of sepsis, and whether there was variation in the laboratory variables, during the course of the disease, was not considered. Third, the analysis did not take into account the dose used and the rate of infusion of the antibiotic administered to each patient, factors that may be decisive in the outcomes according to pharmacokinetic and pharmacodynamic studies [32]. Fourth, the presence of ESβL was established by conventional laboratory methods and no genotypic confirmation was performed.
Conclusions
Mortality after a bacteremic ESβL-E infection is very high. A low frequency of prescription of carbapenems in patients with severe clinical compromise, due to septic shock requiring vasoactive support and Pitt bacteremia score > 3 were identified as risk factors for in-hospital death. These findings have serious implications for antibiotic prescription. Involvement of an infectious disease specialist may help improve outcomes.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ESβL:
-
Extended spectrum β-lactamases
- ESβL-E:
-
ESβL-producing Enterobacterales
- CRBSI:
-
Catheter-related blood stream infection
- IQR:
-
Interquartile ranges
- COPD:
-
Chronic obstructive pulmonary disease
- CLSI:
-
Clinical & Laboratory Standards Institute
- MIC:
-
Minimum inhibitory concentration
- IDC:
-
Infectious disease consultation
- BC:
-
Blood culture
- FUBCs:
-
Follow-up blood cultures
- HACEK:
-
Haemophilus spp., Actinobacillus actinomycetemcomitans, Cardiobacterium hominis, Eikenella corrodens, Kingella spp.
References
Chioro A, Coll-Seck AM, Høie B, Moeloek N, Motsoaledi A, Rajatanavin R, Touraine M. Antimicrobial resistance: a priority for global health action. Bull World Health Organ. 2015;93:439.
Vasoo S, Barreto JN, Tosh PK. Emerging issues in gram-negative bacterial resistance: an update for the practicing clinician. Mayo Clin Proc. 2015;90(3):395–403.
Blom A, Ahl J, Månsson F, Resman F, Tham J. The prevalence of ESBL-producing Enterobacteriaceae in a nursing home setting compared with elderly living at home: a cross-sectional comparison. BMC Infect Dis. 2016;16(1):111.
Fernández-Canigia L, Dowzicky MJ. Susceptibility of important Gram-negative pathogens to tigecycline and other antibiotics in Latin America between 2004 and 2010. Ann Clin Microbiol Antimicrob. 2012;11(1):29.
Doi Y, Iovleva A, Bonomo RA. The ecology of extended-spectrum beta-lactamases (ESBLs) in the developed world. J Travel Med. 2017;24(suppl_1):S44–51.
Jones RN, Guzman-Blanco M, Gales AC, Gallegos B, Castro AL, Martino MD, et al. Susceptibility rates in Latin American nations: report from a regional resistance surveillance program (2011). Braz J Infect Dis. 2013;17(6):672–81.
Guzmán-Blanco M, Labarca JA, Villegas MV, Gotuzzo E. Extended spectrum β-lactamase producers among nosocomial Enterobacteriaceae in Latin America. Braz J Infect Dis. 2014;18(4):421–33.
Villegas MV, Correa A, Perez F, Zuluaga T, Radice M, Gutkind G, et al. CTX-M-12 beta-lactamase in a Klebsiella pneumoniae clinical isolate in Colombia. Antimicrob Agents Chemother. 2004;48(2):629–31.
Ling W, Furuya-Kanamori L, Ezure Y, Harris PNA, Paterson DL. Adverse clinical outcomes associated with infections by Enterobacterales producing ESBL (ESBL-E): a systematic review and meta-analysis. JAC Antimicrob Resist. 2021;3(2): dla068.
Lim CL, Spelman D. Mortality impact of empirical antimicrobial therapy in ESBL- and AmpC-producing Enterobacteriaceae bacteremia in an Australian tertiary hospital. Infect Dis Health. 2019;24(3):124–33.
Friedman ND, Kaye KS, Stout JE, McGarry SA, Trivette SL, Briggs JP, et al. Health care–associated bloodstream infections in adults: a reason to change the accepted definition of community-acquired infections. Ann Intern Med. 2002;137(10):791–7.
Lenz R, Leal JR, Church DL, Gregson DB, Ross T, Laupland KB. The distinct category of healthcare associated bloodstream infections. BMC Infect Dis. 2012;12(1):85.
Miller JM, Binnicker MJ, Campbell S, Carroll KC, Chapin KC, Gilligan PH, et al. A guide to utilization of the microbiology laboratory for diagnosis of infectious diseases: 2018 update by the infectious diseases Society of America and the American Society for Microbiology. Clin Infect Dis. 2018;67(6):e1–94.
Freifeld AG, Bow EJ, Sepkowitz KA, Boeckh MJ, Ito JI, Mullen CA, et al. Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 update by the infectious diseases Society of America. Clin Infect Dis. 2011;52(4):e56–93.
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA. 2016;315(8):801–10.
Alebel M, Mekonnen F, Mulu W. Extended-spectrum β-lactamase and carbapenemase producing gram-negative Bacilli infections among patients in intensive care units of Felegehiwot referral hospital: a prospective cross-sectional study. Infect Drug Resist. 2021;14:391–405.
Namikawa H, Yamada K, Fujimoto H, Oinuma KI, Tochino Y, Takemoto Y, et al. Clinical characteristics of bacteremia caused by extended-spectrum beta-lactamase-producing Escherichia coli at a tertiary hospital. Intern Med. 2017;56(14):1807–15.
Scheuerman O, Schechner V, Carmeli Y, Gutiérrez-Gutiérrez B, Calbo E, Almirante B, et al. Comparison of predictors and mortality between bloodstream infections caused by ESBL-producing Escherichia coli and ESBL-producing Klebsiella pneumoniae. Infect Control Hosp Epidemiol. 2018;39(6):660–7.
Francisco Tuon F, Kruger M, Terreri M, Penteado-Filho SR, Gortz L. Klebsiella ESBL bacteremia-mortality and risk factors. Braz J Infect Dis. 2011;15(6):594–8.
Peker N, Couto N, Sinha B, Rossen JW. Diagnosis of bloodstream infections from positive blood cultures and directly from blood samples: recent developments in molecular approaches. Clin Microbiol Infect. 2018;24(9):944–55.
Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med. 2017;43(3):304–77.
Gudiol C, Cuervo G, Carratalà J. Optimizing therapy of bloodstream infection due to extended-spectrum β-lactamase-producing Enterobacteriaceae. Curr Opin Crit Care. 2019;25(5):438–48.
Vogel M, Schmitz RPH, Hagel S, Pletz MW, Gagelmann N, Scherag A, et al. Infectious disease consultation for Staphylococcus aureus bacteremia—a systematic review and meta-analysis. J Infect. 2016;72(1):19–28.
Bai AD, Showler A, Burry L, Steinberg M, Ricciuto DR, Fernandes T, et al. Impact of infectious disease consultation on quality of care, mortality, and length of stay in Staphylococcus aureus bacteremia: results from a large multicenter cohort study. Clin Infect Dis. 2015;60(10):1451–61.
Raza SS, Sultan OW, Sohail MR. Gram-negative bacterial endocarditis in adults: state-of-the-heart. Expert Rev Anti Infect Ther. 2010;8(8):879–85.
Cahill TJ, Prendergast BD. Infective endocarditis. Lancet. 2016;387(10021):882–93.
Fluckiger U, Zimmerli W, Sax H, Frei R, Widmer AF. Clinical impact of an infectious disease service on the management of bloodstream infection. Eur J Clin Microbiol Infect Dis. 2000;19(7):493–500.
Schmitt S, McQuillen DP, Nahass R, Martinelli L, Rubin M, Schwebke K, et al. Infectious diseases specialty intervention is associated with decreased mortality and lower healthcare costs. Clin Infect Dis. 2014;58(1):22–8.
Schmitt S, MacIntyre AT, Bleasdale SC, Ritter JT, Nelson SB, Berbari EF, et al. Early infectious diseases specialty intervention is associated with shorter hospital stays and lower readmission rates: a retrospective cohort study. Clin Infect Dis. 2019;68(2):239–46.
Canzoneri CN, Akhavan BJ, Tosur Z, Andrade PEA, Aisenberg GM. Follow-up blood cultures in gram-negative bacteremia: are they needed? Clin Infect Dis. 2017;65(11):1776–9.
Thaden JT, Cantrell S, Dagher M, Tao Y, Ruffin F, Maskarinec SA, et al. Association of follow-up blood cultures with mortality in patients with gram-negative bloodstream infections: a systematic review and meta-analysis. JAMA Netw Open. 2022;5(9):e2232576.
Tsai D, Lipman J, Roberts JA. Pharmacokinetic/pharmacodynamic considerations for the optimization of antimicrobial delivery in the critically ill. Curr Opin Crit Care. 2015;21(5):412–20.
Acknowledgements
All authors are grateful to the study center and to Dr. Carmen Elisa Llanos Uribe for her unconditional support.
Funding
The mentioned authors are not currently receiving and have not received any financial support for the development of the manuscript mentioned above. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. DAR was responsible for the development of the research and writing of the entire manuscript. JAHP, GAMG and JAA contributed to the methodological development and many of the ideas that were raised in the discussion and conclusions. JCOG, ICB and CVM contributed to the methodological development and some of the ideas that were raised in the discussion. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This retrospective, single-institution study was approved by the ethics and bioethics committee of the Universidad Tecnológica de Pereira, Colombia. This committee considered that the investigation was risk-free and gave authorization for the development of this investigation. The requirement for informed consent was waived because of the retrospective nature of the research. Administrative permissions were required to access the raw data, so we obtained authorization to handle raw data from the study center. The data of each patient were handled anonymously. All human data of patients’ records were confirmed for collection in accordance with the relevant guidelines and regulations.
Competing interests
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Arias Ramos, D., Alzate, J.A., Moreno Gómez, G.A. et al. Empirical treatment and mortality in bacteremia due to extended spectrum β-lactamase producing Enterobacterales (ESβL-E), a retrospective cross-sectional study in a tertiary referral hospital from Colombia. Ann Clin Microbiol Antimicrob 22, 13 (2023). https://doi.org/10.1186/s12941-023-00566-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12941-023-00566-2