Abstract
Background
The higher level of neutrophil on admission has been reported to predict worse 3-month outcomes in ischemic stroke patients. Our study was to explore the dynamic changes of neutrophil and lymphocyte after r-tPA thrombolysis of ischemic stroke and the relationship with parenchymal hemorrhage (PH) and 3-month function outcome.
Methods
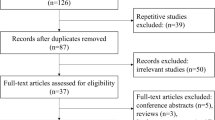
A total of 208 acute ischemic stroke (AIS) patients with intravenous thrombolysis were included and then received 3-month follow-up in the present study. Blood samples for neutrophil and lymphocyte counts were obtained on admission, at 24 h and at 7 days after r-tPA infusion. The associations of increase in neutrophil, lymphocyte, and neutrophil to lymphocyte ratio (NLR) with PH or 3-month poor outcome were examined by logistic regression.
Results
Increasing trends in the neutrophil and NLR were observed in AIS patients after r-tPA treatment. Increased level of neutrophil at 24 h after r-tPA infusion but not that on admission was associated with PH (OR = 2.86, P = 0.029) and 3-month poorer functional outcomes (OR = 2.67, P = 0.009). Moreover, patients were divided into four groups according to the percent change in neutrophil within 24 h following r-tPA treatment, and we found that there was a trend of incremental OR when compared higher increase group with lower ones.
Conclusions
Dynamic increase in neutrophil and NLR after stroke may predict PH and 3-month poor outcome in AIS patients receiving r-tPA treatment. Therefore, neutrophil and NLR may serve as activity markers for PH and 3-month poor prognosis in AIS patients with intravenous thrombolysis.


Similar content being viewed by others
Abbreviations
- PH:
-
Parenchymal hemorrhage
- HT:
-
Hemorrhagic transformation
- AIS:
-
Acute ischemic stroke
- NLR:
-
Neutrophil to lymphocyte ratio
- r-tPA:
-
Recombinant tissue plasminogen activator
- MMP-9:
-
Matrix metalloproteinase-9
- BBB:
-
Blood-brain barrier
- OTT:
-
Onset to treatment time
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- NIHSS:
-
National Institutes of Health Stroke Scale
- MRS:
-
Modified Rankin scale
- SD:
-
Standard deviation
- MCAO:
-
Middle cerebral artery occlusion
- CRP:
-
C-Reactive protein
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- IQR:
-
Interquartile ranges
- sICH:
-
Symptomatic intracerebral hemorrhages
References
Sacco RL, Kasner SE, Broderick JP et al (2013) An updated definition of stroke for the 21st century a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke -Dallas 44(7):2064–2089
Meschia JF, Bushnell C, Bodenalbala B et al (2014) Guidelines for the primary prevention of stroke: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 45(12):3754–3832
Group IC, Sandercock P, Wardlaw JM et al (2012) The benefits and harms of intravenous thrombolysis with recombinant tissue plasminogen activator within 6 h of acute ischaemic stroke (the third international stroke trial [IST-3]): a randomised controlled trial. Lancet. 379(9834):2352–2363
Hacke W, Kaste M, Bluhmki E et al (2008) Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med
Jickling GC, Liu D, Stamova B, Ander BP, Zhan X, Lu A, Sharp FR (2014) Hemorrhagic transformation after ischemic stroke in animals and humans. J Cereb Blood Flow Metab 34(2):185–199
Zhu W, Guo Z, Yu S, Leys D, Bordet R (2015) Higher neutrophil counts before thrombolysis for cerebral ischemia predict worse outcomes. Neurology 85(16):1408–1416
Guo Z, Yu S, Xiao L, Chen X, Ye R, Zheng P, Dai Q, Sun W, Zhou C, Wang S, Zhu W, Liu X (2016) Dynamic change of neutrophil to lymphocyte ratio and hemorrhagic transformation after thrombolysis in stroke. J Neuroinflammation 13(1):199
Kim JY, Park J, Ji YC, Kim SH, Lee JE. Inflammation after ischemic stroke: the role of leukocytes and glial cells. Exp Neurobiol. 2016. 25(5): 241-
Herz J, Sabellek P, Lane TE, Gunzer M, Hermann DM, Doeppner TR (2015) Role of neutrophils in exacerbation of brain injury after focal cerebral ischemia in hyperlipidemic mice. Stroke 46(10):2916–2925
Perez-De-Puig I, Miró-Mur F, Ferrer-Ferrer M et al (2015) Neutrophil recruitment to the brain in mouse and human ischemic stroke. Acta Neuropathol 129(2):239–257
Tokgoz S, Keskin S, Kayrak M, Seyithanoglu A, Ogmegul A (2014) Is neutrophil/lymphocyte ratio predict to short-term mortality in acute cerebral infarct independently from infarct volume. J Stroke Cerebrovasc Dis 23(8):2163–2168
Schwartz M, Moalem G (2001) Beneficial immune activity after CNS injury: prospects for vaccination. J Neuroimmunol 113(2):185–192
Fang YN, Tong MS, Sung PH et al (2017) Higher neutrophil counts and neutrophil-to-lymphocyte ratio predict prognostic outcomes in patients after non-atrial fibrillation-caused ischemic stroke. Biom J 40(3):154–162
Rosell A, Cuadrado E, Ortegaaznar A, Hernándezguillamon M, Lo EH, Montaner J (2008) MMP-9-positive neutrophil infiltration is associated to blood-brain barrier breakdown and basal lamina type IV collagen degradation during hemorrhagic transformation after human ischemic stroke. Stroke. 39(4):1121–1126
Mao Leilei,Li Peiying,Zhu Wen et al. Regulatory T cells ameliorate tissue plasminogen activator-induced brain haemorrhage after stroke.[J] .Brain, 2017, 140: 1914-1931
Xue J, Huang W, Chen X, Li Q, Cai Z, Yu T, Shao B (2017) Neutrophil-to-lymphocyte ratio is a prognostic marker in acute ischemic stroke. J Stroke Cerebrovasc Dis 26(3):650–657
Qun S, Tang Y, Sun J et al (2017) Neutrophil-to-lymphocyte ratio predicts 3-month outcome of acute ischemic stroke. Neurotox Res 31(3):1–9
Pektezel M Yasir,Yilmaz Ezgi,Arsava E Murat et al. Neutrophil-to-lymphocyte ratio and response to intravenous thrombolysis in patients with acute ischemic stroke.[J] .J Stroke Cerebrovasc Dis, 2019, 28: 1853–1859
Aho K, Harmsen P, Hatano S, Marquardsen J, Smirnov VE, Strasser T (1980) Cerebrovascular disease in the community: results of a WHO collaborative study. Bull World Health Organ 58(1):113–130
Jauch EC, Saver JL, Adams HP et al (2013) Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Circulation. 8(3):870–947
Churilov L, Arnup S, Johns H et al (2015) An improved method for simple, assumption-free ordinal analysis of the modified Rankin scale using generalized odds ratios. Int J Stroke 9(8):999–1005
Maestrini I, Strbian D, Gautier S, Haapaniemi E, Moulin S, Sairanen T, Dequatre-Ponchelle N, Sibolt G, Cordonnier C, Melkas S, Leys D, Tatlisumak T, Bordet R (2015) Higher neutrophil counts before thrombolysis for cerebral ischemia predict worse outcomes. Neurology. 85(16):1408–1416
Duan Z, Wang H, Wang Z, Hao Y, Zi W, Yang D, Zhou Z, Liu W, Lin M, Shi Z, Lv P, Wan Y, Xu G, Xiong Y, Zhu W, Liu X, ACTUAL Investigators (2018) Neutrophil-lymphocyte ratio predicts functional and safety outcomes after endovascular treatment for acute ischemic stroke. Cerebrovasc Dis 45(5–6):221–227
Raymond S, Connie W (2016) Ischemia, immunosuppression and infection—tackling the predicaments of post-stroke complications. Int J Mol Sci 17(1):551–556
Muhammad S, Haasbach E, Kotchourko M et al (2011) Influenza virus infection aggravates stroke outcome. Stroke 42(3):783
Mccoll BW, Allan SM, Rothwell NJ (2009) Systemic infection, inflammation and acute ischemic stroke. Neuroscience. 158(3):1049–1061
Zeller JA, Lenz A, Eschenfelder CC et al (2005) Platelet–leukocyte interaction and platelet activation in acute stroke with and without preceding infection. Arter Thromb Vas Biol 25(7):1519
Barone FC, Hillegass LM, Price WJ, White RF, Lee EV, Feuerstein GZ, Sarau HM, Clark RK, Griswold DE (1991) Polymorphonuclear leukocyte infiltration into cerebral focal ischemic tissue: myeloperoxidase activity assay and histologic verification. J Neurosci Res 29(3):336–345
Kim J, Song T, Park JH, Lee HS, Nam CM, Nam HS, Kim YD, Heo JH Different prognostic value of white blood cell subtypes in patients with acute cerebral infarction. Atherosclerosis. 2012. 222(2): 464–467
Matsuo Y, Kihara T, Ikeda M, Ninomiya M, Onodera H, Kogure K (1995) Role of neutrophils in radical production during ischemia and reperfusion of the rat brain: effect of neutrophil depletion on extracellular ascorbyl radical formation. J Cereb Blood Flow Metab 15(6):941–947
Dirnagl U (1999) Pathobiology of ischaemic stroke : an integrated view. Trends Neurosci 22(9):391–397
Buck BH, Liebeskind DS, Saver JL, Bang OY, Yun SW, Starkman S, Ali LK, Kim D, Villablanca JP, Salamon N, Razinia T, Ovbiagele B (2008) Early Neutrophilia is associated with volume of ischemic tissue in acute stroke. Stroke. 39(2):355–360
Shi J, Peng H, You S, Liu Y, Liu CF (2018) Increase in neutrophil after r-tPA thrombolysis predicts poor functional outcome of ischemic stroke: a longitudinal study. Eur J Neurol 25(4):687–e645
Gautier S, Ouk T, Tagzirt M et al (2014) Impact of the neutrophil response to granulocyte colony-stimulating factor on the risk of hemorrhage when used in combination with tissue plasminogen activator during the acute phase of experimental stroke. J Neuroinflammation 11(1):96
Mccoll BW, Rothwell NJ, Allan SM (2007) Systemic inflammatory stimulus potentiates the acute phase and CXC chemokine responses to experimental stroke and exacerbates brain damage via interleukin-1- and neutrophil-dependent mechanisms. J Neurosci 27(16):4403–4412
Garau A, Bertini R, Colotta F, Casilli F, Bigini P, Cagnotto A, Mennini T, Ghezzi P, Villa P (2005) Neuroprotection with the CXCL8 inhibitor repertaxin in transient brain ischemia. Cytokine. 30(3):125–131
Li Z, Zheng GZ, Rui LZ, Mei L, Chopp M (2003) Effects of a selective CD11b/CD18 antagonist and recombinant human tissue plasminogen activator treatment alone and in combination in a rat embolic model of stroke. Stroke 34(7):1790–1795
Harris AK, Ergul A, Kozak A, Machado LS, Johnson MH, Fagan SC (2005) Effect of neutrophil depletion on gelatinase expression, edema formation and hemorrhagic transformation after focal ischemic stroke. BMC Neurosci 6(1):49
Ludewig P, Sedlacik J, Gelderblom M, Bernreuther C, Korkusuz Y, Wagener C, Gerloff C, Fiehler J, Magnus T, Horst AK (2013) Carcinoembryonic antigen-related cell adhesion molecule 1 inhibits MMP-9-mediated blood-brain-barrier breakdown in a mouse model for ischemic stroke. Circ Res 113(8):1013–1022
Dziedzic T (2015) Systemic inflammation as a therapeutic target in acute ischemic stroke. Expert Rev Neurother 15(5):523–531
Tiainen M, Meretoja A, Strbian D, Suvanto J, Curtze S, Lindsberg PJ, Soinne L, Tatlisumak T, Helsinki Stroke Thrombolysis Registry Group (2013) Body temperature, blood infection parameters, and outcome of thrombolysis-treated ischemic stroke patients. Int J Stroke 8(8):632–638
Napoli MD, Papa F, Bocola V (2001) Prognostic influence of increased C-reactive protein and fibrinogen levels in ischemic stroke. Stroke. 32(1):133–138
Gill D, Sivakumaran P, Wilding P, Love M, Veltkamp R, Kar A (2016) Trends in C-reactive protein levels are associated with neurological change twenty-four hours after thrombolysis for acute ischemic stroke. J Stroke Cerebrovasc Dis 25(8):1966–1969
Funding
This study was supported by the National Natural Science Foundation of China (81673144).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethical approval
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ying, A., Cheng, Y., Lin, Y. et al. Dynamic increase in neutrophil levels predicts parenchymal hemorrhage and function outcome of ischemic stroke with r-tPA thrombolysis. Neurol Sci 41, 2215–2223 (2020). https://doi.org/10.1007/s10072-020-04324-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-020-04324-6