Abstract
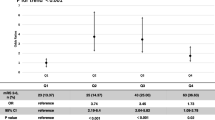
Intravenous injection of alteplase is recommended for patients with minor disabling and not non-disabling ischemic stroke symptoms within 4.5 h of ischemic stroke symptom onset. However, it is hard for clinicians to distinguish which type of minor ischemic stroke is disabled at an early stage. In this study, we aimed to demonstrate early neutrophil-to-lymphocyte ratio is a prognostic marker in acute minor stroke or transient ischemic attack. 196 patients diagnosed with acute minor stroke or transient ischemic attack within 24 h of symptom onset were enrolled. Patients were divided into three groups according to the neutrophil-to-lymphocyte ratio value (< 2, 2–3, > 3). Clinical, neuroradiological, laboratory and follow-up data were collected from electronic database. Functional outcome was assessed by modified Rankin Scale. Neutrophil-to-lymphocyte ratio associated with functional outcome of 90 days was evaluated by logistic regression analysis, and we used receiver operating characteristic curve analysis to detect the overall predictive accuracy of this marker. Early neutrophil-to-lymphocyte ratio was associated with an increased risk of short-term functional outcome (OR 4.502, 95% CI 1.533–13.046, P = 0.006). The optimal cutoff value of neutrophil-to-lymphocyte ratio for prediction of short-term unfavorable outcome was 2.94 with a sensitivity of 69.6% and a specificity of 77.1% (area under the curve: 0.767, 95% CI 0.691–0.843). Early neutrophil-to-lymphocyte ratio is associated with short-term unfavorable functional outcome in patients with acute minor stroke or transient ischemic attack. Early neutrophil-to-lymphocyte ratio is beneficial for clinicians to distinguish minor disabling ischemic stroke at an early stage.


Similar content being viewed by others
References
Wang YL, Wu D, Liao X et al (2007) Burden of stroke in China. Int J Stroke 2:211–213
Liu L, Wang D, Wong KS et al (2011) Stroke and stroke care in China: huge burden, significant workload, and a national priority. Stroke 42:3651–3654
Wang Y, Zhao X, Jiang Y et al (2015) Prevalence, knowledge, and treatment of transient ischemic attacks in China. Neurology 84:2354–2361
Kleindorfer D, Panagos P, Pancioli A et al (2005) Incidence and short-term prognosis of transient ischemic attack in a population-based study. Stroke 36:720–723
Powers WJ, Rabinstein AA, Ackerson T et al (2019) Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 50:e344–e418
Mazza MG, Lucchi S, Rossetti A et al (2019) Neutrophil–lymphocyte ratio, monocyte-lymphocyte ratio and platelet–lymphocyte ratio in non-affective psychosis: a meta-analysis and systematic review. World J Biol Psychiatry 26:1–13
Stojkovic Lalosevic M, Pavlovic Markovic A, Stankovic S et al (2019) Combined diagnostic efficacy of neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), and mean platelet volume (MPV) as biomarkers of systemic inflammation in the diagnosis of colorectal cancer. Dis Markers 2019:6036979. https://doi.org/10.1155/2019/6036979
Siniorakis EE, Tsarouhas K, Tsitsimpikou C et al (2017) Neutrophil to lymphocyte (N/L) and platelet to lymphocyte (P/L) ratios in differentiating acute heart failure from respiratory infection. Curr Vasc Pharmacol 15:477–4781
Wang F, Xu F, Quan Y et al (2019) Early increase of neutrophil-to-lymphocyte ratio predicts 30-day mortality in patients with spontaneous intracerebral hemorrhage. CNS Neurosci Ther 25:30–35
Gusdon AM, Gialdini G, Kone G et al (2017) Neutrophil–lymphocyte ratio and perihematomal edema growth in intracerebral hemorrhage. Stroke 48:2589–2592
Lattanzi S, Cagnetti C, Provinciali L et al (2016) Neutrophil-to-lymphocyte ratio predicts the outcome of acute intracerebral hemorrhage. Stroke 47:1654–1657
Wang F, Hu S, Ding Y et al (2016) Neutrophil-to-lymphocyte ratio and 30-day mortality in patients with acute intracerebral hemorrhage. J Stroke Cerebrovasc Dis 25:182–187
Lattanzi S, Cagnetti C, Rinaldi C et al (2018) Neutrophil-to-lymphocyte ratio improves outcome prediction of acute intracerebral hemorrhage. J Neurol Sci 387:98–102
Tao C, Wang J, Hu X et al (2017) Clinical value of neutrophil to lymphocyte and platelet to lymphocyte ratio after aneurysmal subarachnoid hemorrhage. Neurocrit Care 26:393–401
Lim HH, Jeong IH, An GD et al (2018) Early prediction of severity in acute ischemic stroke and transient ischemic attack using platelet parameters and neutrophil-to-lymphocyte ratio. J Clin Lab Anal 33(3):e22714
Qun S, Tang Y, Sun J et al (2017) Neutrophil-to-lymphocyte ratio predicts 3-month outcome of acute ischemic stroke. Neurotox Res 31:444–452
Xue J, Huang W, Chen X et al (2017) Neutrophil-to-lymphocyte ratio is a prognostic marker in acute ischemic stroke. J Stroke Cerebrovasc Dis 26:650–657
Wang Y, Zhao X, Liu L et al (2013) Clopidogrel with aspirin in acute minor stroke or transient ischemic attack. N Engl J Med 369:11–19
Powers WJ, Derdeyn CP, Biller J et al (2015) 2015 American Heart Association/American Stroke Association focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 46:3020–3035
Kim JY, Park J, Chang JY et al (2016) Inflammation after ischemic stroke: the role of leukocytes and glial cells. Exp Neurobiol 25:241–251
Herz J, Sabellek P, Lane TE et al (2015) Role of neutrophils in exacerbation of brain injury after focal cerebral ischemia in hyperlipidemic mice. Stroke 46:2916–2925
Anrather J, Iadecola C (2016) Inflammation and stroke: an overview. Neurotherapeutics 13:661–6670
Doyle KP, Quach LN, Sole M et al (2015) B-lymphocyte-mediated delayed cognitive impairment following stroke. J Neurosci 35:2133–2145
Lappegard J, Ellingsen TS, Skjelbakken T et al (2016) Red cell distribution width is associated with future risk of incident stroke. The Tromso Study. Thromb Haemost 115:126–134
Huang YL, Han ZJ, Hu ZD (2017) Red blood cell distribution width and neutrophil to lymphocyte ratio are associated with outcomes of adult subarachnoid haemorrhage patients admitted to intensive care unit. Ann Clin Biochem 54:696–701
Okumura K, Ohya Y, Maehara A et al (2005) Effects of blood pressure levels on case fatality after acute stroke. J Hypertens 23:1217–1223
Skalidi SJ, Manios ED, Stamatelopoulos KS et al (2013) Brain edema formation is associated with the time rate of blood pressure variation in acute stroke patients. Blood Press Monit 18:203–207
Divani AA, Liu X, Di Napoli M et al (2019) Blood pressure variability predicts poor in-hospital outcome in spontaneous intracerebral hemorrhage. Stroke 50:2023–2029
Lattanzi S, Silvestrini M (2015) Optimal achieved blood pressure in acute intracerebral hemorrhage: INTERACT2. Neurology 85:557–558
Lattanzi S, Silvestrini M (2016) Blood pressure in acute intra-cerebral hemorrhage. Ann Transl Med 4:320
Buratti L, Cagnetti C, Balucani C et al (2014) Blood pressure variability and stroke outcome in patients with internal carotid artery occlusion. J Neurol Sci 339:164–168
Di Napoli M, Slevin M, Popa-Wagner A et al (2018) Monomeric C-reactive protein and cerebral hemorrhage: from bench to bedside. Front Immunol 9:1921
Zangari R, Zanier ER, Torgano G et al (2016) Early ficolin-1 is a sensitive prognostic marker for functional outcome in ischemic stroke. J Neuroinflammation 13:16
Lattanzi S, Bartolini M, Provinciali L et al (2016) Glycosylated hemoglobin and functional outcome after acute ischemic stroke. J Stroke Cerebrovasc Dis 25:1786–1791
Jafari M, Di Napoli M, Lattanzi S et al (2019) Serum magnesium level and hematoma expansion in patients with intracerebral hemorrhage. J Neurol Sci 398:39–44
Mahmoudi J, Majdi A, Lattanzi S et al (2018) Imidazoline receptor agonists for managing hypertension may hold promise for treatment of intracerebral hemorrhage. Curr Mol Med 18:241–251
Lattanzi S, Silvestrini M, Provinciali L (2013) Elevated blood pressure in the acute phase of stroke and the role of Angiotensin receptor blockers. Int J Hypertens 2013:941783
Easton JD, Saver JL, Albers GW et al (2009) Definition and evaluation of transient ischemic attack: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association Stroke Council; Council on Cardiovascular Surgery and Anesthesia; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Nursing; and the Interdisciplinary Council on Peripheral Vascular Disease. The American Academy of Neurology affirms the value of this statement as an educational tool for neurologists. Stroke 40:2276–2293
Funding
This study was funded by Natural Science Fund of Hubei Province (Grant number 2018CFB322), Health Research Project of Hubei Province, Science and Technology Development Plan of Jingzhou, New Project and New Technology Program of The First People’s Hospital of Jingzhou (Grant number 201826).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were approved by the ethics committee of the first people’s hospital of Jingzhou, and were performed in accordance with the 1964 Declaration of Helsinki.
Informed consent
The board allowed the study to be conducted without patients' consent because of the retrospective nature of the study [11].
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Luo, Y., Xia, Lx., Li, Zl. et al. Early neutrophil-to-lymphocyte ratio is a prognostic marker in acute minor stroke or transient ischemic attack. Acta Neurol Belg 121, 1415–1421 (2021). https://doi.org/10.1007/s13760-020-01289-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13760-020-01289-3