Abstract
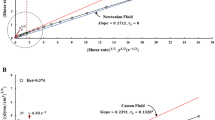
Artificial cardiovascular devices, such as vascular stents, artificial valves, and artificial hearts, can rebuild human cardiovascular functionalities via rebuilding the blood flow passing through these devices. To evaluate the red blood cells (RBCs) damage induced by a non-physiological blood flow in these devices, many hemolysis models have been proposed, of which the most popular one is a power function model. However, it was found that the newly obtained experimental data often did not match the existing power function model. In addition, the experimental period was usually short and the summarized power function model cannot reflect the RBCs damage after long-term exposure to shear stress. To address this issue, in this study a shear device was established on a torque rheometer; the changes of plasma free hemoglobin (FHB) of sheep blood under the shear stress from 10 to 70 Pa and exposure time from 5 to 30 min were recorded and compared. The results showed that as the shear stress and exposure time increased, FHB also increased, but the increase rate gradually decreased. As a result, after undergoing high shear stress or a long period of exposure time, FHB eventually became stable. Obviously, the existing power function model cannot describe this FHB change. In the current study, we used a sigmoidal logistic function model to describe the FHB increment upon the increase of shear stress and long exposure time. The results showed that the proposed model can provide better predictions of hemolysis, particularly in these cases under long exposure time.







Similar content being viewed by others
References
Oyre S, Pedersen EM, Ringgaard S, et al. In vivo wall shear stress measured by magnetic resonance velocity mapping in the normal human abdominal aorta. Eur J Vasc Endovasc Surg. 1997;13:263.
Oyre S, Ringgaard S, Kozerke S, et al. Accurate noninvasive quantitation of blood flow, cross-sectional lumen vessel area and wall shear stress by three-dimensional paraboloid modeling of magnetic resonance imaging velocity data. J Am Coll Cardiol. 1998;32:128–34.
Sheng PW, Ringgaard S, Oyre S, et al. Wall shear rates differ between the normal carotid, femoral, and brachial arteries: an in vivo MRI study. J Magn Reson Imaging. 2004;19:188–93.
Koutsiaris AG, Tachmitzi SV, Batis N, et al. Volume flow and wall shear stress quantification in the human conjunctival capillaries and post-capillary venules in vivo. Biorheology. 2007;44:375–86.
Osinnski JN, Ku DN, Mukundan S Jr, et al. Determination of wall shear stress in the aorta with the use of MR phase velocity mapping. J Magn Reson Imaging. 2010;5:640–7.
Yu H, Engel S, Janiga G, et al. A review of hemolysis prediction models for computational fluid dynamics. Artif Organs. 2017;41:603–21.
Zhang T, Taskin ME, Fang HB, et al. Study of flow-induced hemolysis using novel Couette-type blood-shearing devices. Artif Organs. 2015;35:1180–6.
Giersiepen M, Wurzinger LJ, Opitz R, et al. Estimation of shear stress-related blood damage in heart valve prostheses–in vitro comparison of 25 aortic valves. Int J Artif Organs. 1990;13:300.
Li DH, Wu QY, Liu SH, et al. Lactic dehydrogenase in the in vitro evaluation of hemolytic properties of ventricular assist device. Artif Organs. 2017;41:274–84.
Leverett LB, Hellums JD, Alfrey CP, et al. Red blood cell damage by shear stress. Biophys J. 1972;12:257–73.
Paul R, Apel J, Klaus S, et al. Shear stress related blood damage in laminar Couette flow. Artif Organs. 2015;27:517–29.
Maruyama O, Numata Y, Nishida M, et al. Hemolysis caused by surface roughness under shear flow. J Artif Organs. 2005;8:228–36.
Mankad AK, Flattery M, Tang DG, et al. Persistent anemia in patients supported with the total artificial heart: hemolysis and ineffective erythropoiesis. J Card Fail. 2011;17:S42–S42.
Mankad AK, Tang DG, Clark WB, et al. Persistent anemia after implantation of the total artificial heart. J Card Fail. 2012;18:433–8.
Chan CHH, Pieper IL, Robinson CR, et al. Shear stress-induced total blood trauma in multiple species. Artif Organs. 2017;41:934–47.
Ogoh S, Fadel PJ, Nissen P, et al. Baroreflex-mediated changes in cardiac output and vascular conductance in response to alterations in carotid sinus pressure during exercise in humans. J Physiol. 2010;550:317–24.
Perhonen MA, Franco F, Lane LD, et al. Cardiac atrophy after bed rest and spaceflight. J Appl Physiol. 2001;91:645–53.
Gao L, Schultz HD, Patel KP, et al. Augmented input from cardiac sympathetic afferents inhibits the baroreflex in heart failure. Hypertension. 2005;9:S16–S16.
Williams AR, Escoffery CT, Gorst DW. The fragility of normal and abnormal erythrocytes in a controlled hydrodynamic shear field. Br J Haematol. 2010;37:379–89.
Kent BB, Drane JW, Blumenstein BB, et al. A mathematical model to assess changes in the baroreceptor reflex. Cardiology. 1972;57:295–310.
Acknowledgements
This research is supported by Tsinghua University (School of Medicine)—RocketHeart Co. Ltd Joint Research Center for Artificial Heart (No. 2018291174), Tsinghua University Initiative Scientific Research Program (No. 20182000306), and Tsinghua-Foshan Innovation Special Fund (TFISF, No. 20197050026).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhao, X., Yu, Y., Zhao, L. et al. The red blood cell damage after long-term exposure to shear stresses. J Artif Organs 25, 298–304 (2022). https://doi.org/10.1007/s10047-022-01326-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10047-022-01326-3