Abstract
Purpose
The use of mesh in ventral hernia repair becomes especially challenging when associated with a contaminated field. Permanent synthetic mesh use in this setting is currently debated and this discussion is yet to be resolved clinically or in the literature. We aim to systematically assess postoperative outcomes of non-absorbable synthetic mesh (NASM) used in ventral hernia repair in the setting of contamination.
Methods
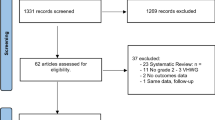
A literature search of PubMed, Embase, Scopus, Cinahl, and Cochrane Library identified all articles from 2000–2020 that examined the use of NASM for ventral hernia repair in a contaminated field. Postoperative outcomes were assessed by means of pooled analysis and meta-analysis. Qualitative analysis was completed for all included studies using a modified Newcastle–Ottawa scale.
Results
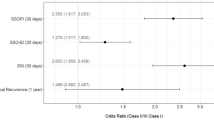
Of 630 distinct publications and 104 requiring full review, this study included 17 articles published between 2007 and 2020. Meta-analysis demonstrated absorbable mesh was associated with more HR (OR 1.89, 1.15–3.12, p = 0.008), SSO (OR 1.43, 0.96–2.11, p = 0.087), SSI (OR 2.84, 1.85–4.35, p < 0.001), and unplanned reoperation (OR 1.99, 1.19–3.32, p = 0.009) compared to NASM.
Conclusion
The use of NASM for ventral hernia repair in a contaminated field may be a safe alternative to absorbable mesh, as evidenced by lower rates of postoperative complications. This review counters the current clinical paradigm, and additional prospective randomized controlled trials are warranted.





Similar content being viewed by others
Availability of data and material
All data and materials comply with field standards.
Code availability
All statistically analysis performed using STATA.
References
Pans A, Elen P, Dewé W, Desaive C (1998) Long-term results of polyglactin mesh for the prevention of incisional hernias in obese patients. World J Surg. https://doi.org/10.1007/s002689900420
Trimbos JB, Smit IB, Holm JP, Hermans J (1992) A randomized clinical trial comparing two methods of fascia closure following midline laparotomy. Arch Surg. https://doi.org/10.1001/archsurg.1992.01420100094016
Luijendijk RW, Hop WCJ, Van Den Tol MP et al (2000) A comparison of suture repair with mesh repair for incisional hernia. N Engl J Med. https://doi.org/10.1056/NEJM200008103430603
Itani KMF, Rosen M, Vargo D et al (2012) Prospective study of single-stage repair of contaminated hernias using a biologic porcine tissue matrix: the RICH Study. Surgery. https://doi.org/10.1016/j.surg.2012.04.008
Holton LH, Kim D, Silverman RP et al (2005) Human acellular dermal matrix for repair of abdominal wall defects: Review of clinical experience and experimental data. J Long Term Eff Med Implants 15:547–558
Shankaran V, Weber DJ, Reed RL, Luchette FA (2011) A review of available prosthetics for ventral hernia repair. Ann Surg. https://doi.org/10.1097/SLA.0b013e3181f9b6e6
Rosen MJ, Krpata DM, Ermlich B, Blatnik JA (2013) A 5-year clinical experience with single-staged repairs of infected and contaminated abdominal wall defects utilizing biologic mesh. Ann Surg. https://doi.org/10.1097/SLA.0b013e3182849871
Harth KC, Krpata DM, Chawla A et al (2013) Biologic mesh use practice patterns in abdominal wall reconstruction: a lack of consensus among surgeons. Hernia. https://doi.org/10.1007/s10029-012-1029-8
Kissane NA, Itani KMF (2012) A decade of ventral incisional hernia repairs with biologic acellular dermal matrix: what have we learned? Plast Reconstr Surg 130:194S-202S
Fischer JP, Basta MN, Krishnan NM et al (2016) A cost-utility assessment of mesh selection in clean-contaminated ventral hernia repair. Plast Reconstr Surg 137(2):647–659
Köckerling F, Alam NN, Antoniou SA et al (2018) What is the evidence for the use of biologic or biosynthetic meshes in abdominal wall reconstruction? Hernia 22(2):249–269
Campanelli G, Nicolosi FM, Pettinari D, Avesani EC (2004) Prosthetic repair, intestinal resection, and potentially contaminated areas: safe and feasible? Hernia 8:190–192
Warren J, Desai SS, Boswell ND et al (2020) Safety and efficacy of synthetic mesh for ventral hernia repair in a contaminated field. J Am Coll Surg 230(4):405–413
Majumder A, Winder JS, Wen Y et al (2016) Comparative analysis of biologic versus synthetic mesh outcomes in contaminated hernia repairs. Surgery. https://doi.org/10.1016/j.surg.2016.04.041
Lee L, Mata J, Landry T et al (2014) A systematic review of synthetic and biologic materials for abdominal wall reinforcement in contaminated fields. Surg Endosc 28(9):2531–2546
Atema JJ, de Vries FEE, Boermeester MA (2016) Systematic review and meta-analysis of the repair of potentially contaminated and contaminated abdominal wall defects. Am J Surg 212:982-995.e1
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:e1000097. https://doi.org/10.1371/journal.pmed.1000097
Stroup DF, Berlin JA, Morton SC et al (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. J Am Med Assoc 283:2008–2012. https://doi.org/10.1001/jama.283.15.2008
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A (2016) Rayyan-a web and mobile app for systematic reviews. Syst Rev 5:210. https://doi.org/10.1186/s13643-016-0384-4
Stang A (2010) Critical evaluation of the Newcastle–Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25:603–605
López-Cano M, Quiles MT, Pereira JA et al (2017) Complex abdominal wall hernia repair in contaminated surgical fields: factors affecting the choice of prosthesis. Am Surg. https://doi.org/10.1177/000313481708300622
de Vries FEE, Hodgkinson JD, Claessen JJM et al (2020) Long-term outcomes after contaminated complex abdominal wall reconstruction. Hernia. https://doi.org/10.1007/s10029-020-02124-7
Nockolds CL, Hodde JP, Rooney PS (2014) Abdominal wall reconstruction with components separation and mesh reinforcement in complex hernia repair. BMC Surg. https://doi.org/10.1186/1471-2482-14-25
Gurrado A, Franco IF, Lissidini G et al (2015) Impact of pericardium bovine patch (Tutomesh®) on incisional hernia treatment in contaminated or potentially contaminated fields: retrospective comparative study. Hernia. https://doi.org/10.1007/s10029-014-1228-6
Sahoo S, Haskins IN, Huang LC et al (2017) Early wound morbidity after open ventral hernia repair with biosynthetic or polypropylene mesh. J Am Coll Surg. https://doi.org/10.1016/j.jamcollsurg.2017.07.1067
Birolini C, de Miranda JS, Tanaka EY et al (2020) The use of synthetic mesh in contaminated and infected abdominal wall repairs: challenging the dogma—a long-term prospective clinical trial. Hernia. https://doi.org/10.1007/s10029-019-02035-2
Keogh K, Slater K (2020) Comparison of biosynthetic versus synthetic mesh in clean and contaminated ventral hernia repairs. ANZ J Surg. https://doi.org/10.1111/ans.15587
Carbonell AM, Criss CN, Cobb WS et al (2013) Outcomes of synthetic mesh in contaminated ventral hernia repairs. J Am Coll Surg. https://doi.org/10.1016/j.jamcollsurg.2013.07.382
Slater NJ, Knaapen L, Bokkerink WJV et al (2015) Large contaminated ventral hernia repair using component separation technique with synthetic mesh. Plast Reconstr Surg 136(6):796e–805e
Köhler G, Weitzendorfer M, Kalcher V, Emmanuel K (2015) Synthetic mesh repair for incisional hernia treatment in high-risk patients for surgical site occurrences. Am Surg. https://doi.org/10.1177/000313481508100430
El-Gazzaz GH, Farag SH, El-Sayd MA, Mohamed HH (2012) The use of synthetic mesh in patients undergoing ventral hernia repair during colorectal resection: risk of infection and recurrence. Asian J Surg. https://doi.org/10.1016/j.asjsur.2012.06.003
Zafar H, Zaidi M, Qadir I, Memon AA (2012) Emergency incisional hernia repair: a difficult problem waiting for a solution. Ann Surg Innov Res. https://doi.org/10.1186/1750-1164-6-1
van’t Riet M, van Steenwijk PJV, Bonjer HJ et al (2007) Mesh repair for postoperative wound dehiscence in the presence of infection: is absorbable mesh safer than non-absorbable mesh? Hernia. https://doi.org/10.1007/s10029-007-0240-5
Birolini C, de Miranda JS, Utiyama EM et al (2016) Active Staphylococcus aureus infection: Is it a contra-indication to the repair of complex hernias with synthetic mesh? A prospective observational study on the outcomes of synthetic mesh replacement, in patients with chronic mesh infection caused by Stap. Int J Surg. https://doi.org/10.1016/j.ijsu.2016.02.062
Pandey H, Thakur DS, Somashekar U et al (2018) Use of polypropylene mesh in contaminated and dirty strangulated hernias: short-term results. Hernia. https://doi.org/10.1007/s10029-018-1811-3
Öberg S, Andresen K, Rosenberg J (2017) Absorbable meshes in inguinal hernia surgery: a systematic review and meta-analysis. Surg Innov 24:289–298
Pizza F, D’Antonio D, Arcopinto M et al (2020) Safety and efficacy of prophylactic resorbable biosynthetic mesh following midline laparotomy in clean/contemned field: preliminary results of a randomized double blind prospective trial. Hernia 24:85–92. https://doi.org/10.1007/s10029-019-02025-4
Wang XC, Zhang D, Yang ZX et al (2017) Mesh reinforcement for the prevention of incisional hernia formation: a systematic review and meta-analysis of randomized controlled trials. J Surg Res 209:17–29
Bondre IL, Holihan JL, Askenasy EP et al (2015) Suture, synthetic, or biologic in contaminated ventral hernia repair. J Surg Res. https://doi.org/10.1016/j.jss.2015.09.007
Breuing K, Butler CE, Ferzoco S et al (2010) Incisional ventral hernias: review of the literature and recommendations regarding the grading and technique of repair. Surgery. https://doi.org/10.1016/j.surg.2010.01.008
Rosen MJ, Bauer JJ, Harmaty M et al (2017) Multicenter, prospective, longitudinal study of the recurrence, surgical site infection, and quality of life after contaminated ventral hernia repair using biosynthetic absorbable mesh: the COBRA study. Ann Surg. https://doi.org/10.1097/SLA.0000000000001601
Leber GE, Garb JL, Alexander AI, Reed WP (1998) Long-term complications associated with prosthetic repair of incisional hernias. Arch Surg 133:378–382. https://doi.org/10.1001/archsurg.133.4.378
Cruse PJE, Foord R (1980) The epidemiology of wound infection. A 10-year prospective study of 62,939 wounds. Surg Clin North Am 60:27–40. https://doi.org/10.1016/S0039-6109(16)42031-1
Tubre DJ, Schroeder AD, Estes J et al (2018) Surgical site infection: the “Achilles Heel” of all types of abdominal wall hernia reconstruction. Hernia 22:1003–1013
Mulder IM, Deerenberg EB, Bemelman WA, et al (2015) Infection susceptibility of crosslinked and non-crosslinked biological meshes in an experimental contaminated environment. In: American Journal of Surgery. Elsevier Inc., pp 159–166
Ditzel M, Deerenberg EB, Grotenhuis N et al (2013) Biologic meshes are not superior to synthetic meshes in ventral hernia repair: an experimental study with long-term follow-up evaluation. Surg Endosc 27:3654–3662. https://doi.org/10.1007/s00464-013-2939-y
Schneeberger S, Phillips S, Huang L-C et al (2019) Cost-utility analysis of biologic and biosynthetic mesh in ventral hernia repair: when are they worth it? J Am Coll Surg. https://doi.org/10.1016/j.jamcollsurg.2018.10.009
Basta MN, Kozak GM, Broach RB et al (2019) Can we predict incisional hernia?: development of a surgery-specific decision-support interface. Ann Surg 270:544–553. https://doi.org/10.1097/SLA.0000000000003472
Funderburk CD, Batulis NS, Zelones JT et al (2019) Innovations in the plastic surgery care pathway using telemedicine for clinical efficiency and patient satisfaction. Plast Reconstr Surg. https://doi.org/10.1097/PRS.0000000000005884
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by MPM, JAM, ANC, VP, and RBB. The first draft of the manuscript was written by MM and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
JPF has received funding and consulting fees from Becton- Dickinson, Integra, Gore and Baxter.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Human and animal rights
This study does not include human or animal participants.
Informed consent
Informed consent was not required for this review study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Morris, M.P., Mellia, J.A., Christopher, A.N. et al. Ventral hernia repair with synthetic mesh in a contaminated field: a systematic review and meta-analysis. Hernia 25, 1035–1050 (2021). https://doi.org/10.1007/s10029-020-02358-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-020-02358-5