Abstract
The link between inflammatory disorders, such as asthma, and attention deficit hyperactivity disorder (ADHD) is attracting increasing attention but few studies have examined cross-generational associations. We sought to examine associations of maternal asthma and asthma exacerbation during pregnancy, as well as paternal asthma, with the risk of ADHD in children. This population-based cohort study used data from the Taiwan National Health Insurance Research Database from 2004 to 2017. Cox regression models compared the risk of ADHD in children of parents with and without asthma, adjusting for parental sociodemographic, physical, and mental health conditions, as well as the child’s birth weight, and number of births. A sibling control approach was employed to compensate for unmeasured confounders of asthma exacerbation during pregnancy. In the fully adjusted models, maternal and paternal asthma were both significantly associated with an increased risk of ADHD in offspring, with hazard ratios (HRs) of 1.36 (1.31-1.40) and 1.10 (1.05-1.14), respectively. Acute asthma exacerbation during pregnancy was not associated with the risk of further offspring ADHD (adjusted HR 1.00, 95% CI: 0.75-1.34). Both maternal and paternal asthma are associated with an increased risk of ADHD in offspring. The risk was higher from maternal asthma. However, no such association was found with maternal asthma exacerbation during pregnancy of sibling comparison.
Similar content being viewed by others
Data availability
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Code availability
Not applicable.
References
American Psychiatric Association (2013) Diagnostic and statistical manual of mental diseases. American Psychiatric Publishing, Washington, DC
Brew BK, Gong T (2020) Modelling paternal exposure as a negative control. Int J Epidemiol 49:1053–1054. https://doi.org/10.1093/ije/dyaa054
Chen W, Zhou K, Sham P, Franke B, Kuntsi J, Campbell D, Fleischman K, Knight J, Andreou P, Arnold R, Altink M, Boer F, Boholst MJ, Buschgens C, Butler L, Christiansen H, Fliers E, Howe-Forbes R, Gabriëls I, Heise A, Korn-Lubetzki I, Marco R, Medad S, Minderaa R, Müller UC, Mulligan A, Psychogiou L, Rommelse N, Sethna V, Uebel H, McGuffin P, Plomin R, Banaschewski T, Buitelaar J, Ebstein R, Eisenberg J, Gill M, Manor I, Miranda A, Mulas F, Oades RD, Roeyers H, Rothenberger A, Sergeant J, Sonuga-Barke E, Steinhausen HC, Taylor E, Thompson M, Faraone SV, Asherson P (2008) DSM-IV combined type ADHD shows familial association with sibling trait scores: a sampling strategy for QTL linkage. Am J Med Genet B Neuropsychiatr Genet 147b:1450–1460. https://doi.org/10.1002/ajmg.b.30672
Class QA, Rickert ME, Larsson H, Lichtenstein P, D’Onofrio BM (2014) Fetal growth and psychiatric and socioeconomic problems: population-based sibling comparison. Br J Psychiatry 205:355–361. https://doi.org/10.1192/bjp.bp.113.143693
Cowell WJ, Bellinger DC, Wright RO, Wright RJ (2019) Antenatal active maternal asthma and other atopic disorders is associated with ADHD behaviors among school-aged children. Brain Behav Immun 80:871–878. https://doi.org/10.1016/j.bbi.2019.05.040
Dalsgaard S, Hansen N, Mortensen PB, Damm D, Thomsen PH (2001) Reassessment of ADHD in a historical cohort of children treated with stimulants in the period 1969–1989. Eur Child Adolesc Psychiatry 10:230–239. https://doi.org/10.1007/s007870170012
Dalsgaard S, Østergaard SD, Leckman JF, Mortensen PB, Pedersen MG (2015) Mortality in children, adolescents, and adults with attention deficit hyperactivity disorder: a nationwide cohort study. Lancet 385:2190–2196. https://doi.org/10.1016/s0140-6736(14)61684-6
Demontis D, Walters RK, Martin J, Mattheisen M, Als TD, Agerbo E, Baldursson G, Belliveau R, Bybjerg-Grauholm J, Bækvad-Hansen M, Cerrato F, Chambert K, Churchhouse C, Dumont A, Eriksson N, Gandal M, Goldstein JI, Grasby KL, Grove J, Gudmundsson OO, Hansen CS, Hauberg ME, Hollegaard MV, Howrigan DP, Huang H, Maller JB, Martin AR, Martin NG, Moran J, Pallesen J, Palmer DS, Pedersen CB, Pedersen MG, Poterba T, Poulsen JB, Ripke S, Robinson EB, Satterstrom FK, Stefansson H, Stevens C, Turley P, Walters GB, Won H, Wright MJ, Andreassen OA, Asherson P, Burton CL, Boomsma DI, Cormand B, Dalsgaard S, Franke B, Gelernter J, Geschwind D, Hakonarson H, Haavik J, Kranzler HR, Kuntsi J, Langley K, Lesch KP, Middeldorp C, Reif A, Rohde LA, Roussos P, Schachar R, Sklar P, Sonuga-Barke EJS, Sullivan PF, Thapar A, Tung JY, Waldman ID, Medland SE, Stefansson K, Nordentoft M, Hougaard DM, Werge T, Mors O, Mortensen PB, Daly MJ, Faraone SV, Børglum AD, Neale BM (2019) Discovery of the first genome-wide significant risk loci for attention deficit/hyperactivity disorder. Nat Genet 51:63–75. https://doi.org/10.1038/s41588-018-0269-7
Faraone SV, Perlis RH, Doyle AE, Smoller JW, Goralnick JJ, Holmgren MA, Sklar P (2005) Molecular genetics of attention-deficit/hyperactivity disorder. Biol Psychiatry 57:1313–1323. https://doi.org/10.1016/j.biopsych.2004.11.024
Grizenko N, Osmanlliu E, Fortier M, Joober R (2015) Increased risk of asthma in children with ADHD: role of Prematurity and maternal stress during pregnancy. J Can Acad Child Adolesc Psychiatry 24:109–115
Halmøy A, Klungsøyr K, Skjærven R, Haavik J (2012) Pre- and perinatal risk factors in adults with attention-deficit/hyperactivity disorder. Biol Psychiatry 71:474–481. https://doi.org/10.1016/j.biopsych.2011.11.013
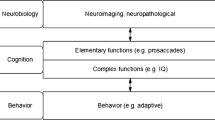
Hinshaw SP (2018) Attention deficit hyperactivity disorder (ADHD): controversy, Developmental mechanisms, and multiple levels of analysis. Annu Rev Clin Psychol 14:291–316. https://doi.org/10.1146/annurev-clinpsy-050817-084917
Indredavik MS, Vik T, Evensen KA, Skranes J, Taraldsen G, Brubakk AM (2010) Perinatal risk and psychiatric outcome in adolescents born preterm with very low birth weight or term small for gestational age. J Dev Behav Pediatr 31:286–294. https://doi.org/10.1097/DBP.0b013e3181d7b1d3
Instanes JT, Halmøy A, Engeland A, Haavik J, Furu K, Klungsøyr K (2017) Attention-Deficit/Hyperactivity disorder in offspring of mothers with inflammatory and Immune System diseases. Biol Psychiatry 81:452–459. https://doi.org/10.1016/j.biopsych.2015.11.024
Lee YC, Yang HJ, Chen VC, Lee WT, Teng MJ, Lin CH, Gossop M (2016) Meta-analysis of quality of life in children and adolescents with ADHD: by both parent proxy-report and child self-report using PedsQL™. Res Dev Disabil 51–52:160–172. https://doi.org/10.1016/j.ridd.2015.11.009
Li C-Y, Chen L-H, Chiou M-J, Liang F-W, Lu T-H (2016) Set-up and future applications of the Taiwan Maternal and Child Health Database (TMCHD). Taiwan J Public Health 35:209–220. https://doi.org/10.6288/TJPH201635104053
Li DJ, Tsai CS, Hsiao RC, Chen YL, Yen CF (2022) Associations between allergic and autoimmune diseases with Autism Spectrum disorder and Attention-Deficit/Hyperactivity disorder within families: a Population-based Cohort Study. Int J Environ Res Public Health 19. https://doi.org/10.3390/ijerph19084503
Linnet KM, Wisborg K, Agerbo E, Secher NJ, Thomsen PH, Henriksen TB (2006) Gestational age, birth weight, and the risk of hyperkinetic disorder. Arch Dis Child 91:655–660. https://doi.org/10.1136/adc.2005.088872
Linnet KM, Wisborg K, Secher NJ, Thomsen PH, Obel C, Dalsgaard S, Henriksen TB (2009) Coffee consumption during pregnancy and the risk of hyperkinetic disorder and ADHD: a prospective cohort study. Acta Paediatr 98:173–179. https://doi.org/10.1111/j.1651-2227.2008.00980.x
Liu X, Dalsgaard S, Munk-Olsen T, Li J, Wright RJ, Momen NC (2019) Parental asthma occurrence, exacerbations and risk of attention-deficit/hyperactivity disorder. Brain Behav Immun 82:302–308. https://doi.org/10.1016/j.bbi.2019.08.198
Moffatt MF, Cookson WO (1998) The genetics of asthma. Maternal effects in atopic disease. Clin Exp Allergy 28 Suppl 156–61 discussion 65 – 56. https://doi.org/10.1046/j.1365-2222.1998.0280s1056.x
Mohr-Jensen C, Vinkel Koch S, Briciet Lauritsen M, Steinhausen HC (2016) The validity and reliability of the diagnosis of hyperkinetic disorders in the Danish Psychiatric Central Research Registry. Eur Psychiatry 35:16–24. https://doi.org/10.1016/j.eurpsy.2016.01.2427
NHIRD (2006) National Health Insurance Research Database, Taiwan. Introduction to the National Health Insurance Research Database (NHIRD), Taiwan (http://www.nhri.org.tw/nhird/en/index.htm>). Accessed 20 January 2010. https://
Nigg JT, Breslau N (2007) Prenatal smoking exposure, low birth weight, and disruptive behavior disorders. J Am Acad Child Adolesc Psychiatry 46:362–369. https://doi.org/10.1097/01.chi.0000246054.76167.44
Pettersson E, Sjölander A, Almqvist C, Anckarsäter H, D’Onofrio BM, Lichtenstein P, Larsson H (2015) Birth weight as an independent predictor of ADHD symptoms: a within-twin pair analysis. J Child Psychol Psychiatry 56:453–459. https://doi.org/10.1111/jcpp.12299
Sayal K, Prasad V, Daley D, Ford T, Coghill D (2018) ADHD in children and young people: prevalence, care pathways, and service provision. Lancet Psychiatry 5:175–186. https://doi.org/10.1016/s2215-0366(17)30167-0
Schans JV, Çiçek R, de Vries TW, Hak E, Hoekstra PJ (2017) Association of atopic diseases and attention-deficit/hyperactivity disorder: a systematic review and meta-analyses. Neurosci Biobehav Rev 74:139–148. https://doi.org/10.1016/j.neubiorev.2017.01.011
Thapar A, Stergiakouli E (2008) An overview on the Genetics of ADHD. Xin Li Xue Bao 40:1088–1098. https://doi.org/10.3724/sp.J.1041.2008.01088
Thapar A, Cooper M, Eyre O, Langley K (2013) What have we learnt about the causes of ADHD? J Child Psychol Psychiatry 54:3–16. https://doi.org/10.1111/j.1469-7610.2012.02611.x
Willcutt EG (2012) The prevalence of DSM-IV attention-deficit/hyperactivity disorder: a meta-analytic review. Neurotherapeutics 9:490–499. https://doi.org/10.1007/s13311-012-0135-8
Yang IV (2014) Epigenetics and prenatal influences on asthma and allergic airways disease. Breathe 10:24–31. https://doi.org/10.1183/20734735.000814
Funding
This work was supported by (i) the NIHR Maudsley Biomedical Research Centre at the South London and Maudsley NHS Foundation Trust and King’s College London; (ii) the National Institute for Health Research (NIHR) Applied Research Collaboration South London (NIHR ARC South London) at King’s College Hospital NHS Foundation Trust; (iii) UKRI – Medical Research Council through the DATAMIND HDR UK Mental Health Data Hub (Grant Numbers: MR/W014386); (iv) the UK Prevention Research Partnership Violence, Health and Society ( Grant Numbers: MR-VO49879/1), an initiative funded by UK Research and Innovation Councils, the Department of Health and Social Care (England) and the UK devolved administrations, and leading health research charities.
Author information
Authors and Affiliations
Contributions
Yi-Feng Ho, Vincent Chin-Hung Chen and Tsai-Ching Hsu contributed to the study conception and design. Material preparation, data collection and analysis were performed by Yi-Lung Chen. The first draft of the manuscript was written by Yi-Feng Ho and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Chang Gung Medical Foundation (Date2020.05.25/No.202000880B0).
Informed consent
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ho, YF., Chen, YL., Stewart, R. et al. Maternal asthma and asthma exacerbation during pregnancy and attention-deficit/hyperactivity disorder in offspring: a population-based cohort study. Eur Child Adolesc Psychiatry (2024). https://doi.org/10.1007/s00787-024-02426-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00787-024-02426-6