Abstract
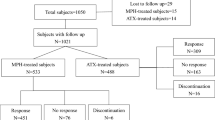
This Taiwan study examined the associations of parental age and mental disorders with the offspring risks of attention-deficit/hyperactivity disorder (ADHD), autism spectrum disorder (ASD), major depressive disorder (MDD), and bipolar disorder (BD). Children born between January 1991 and December 2004 in Taiwan were enrolled as the birth cohort (n = 4,138,151) and followed up until December 2011. A logistic regression analysis was performed to identify the odds ratio (OR). The advanced age effects were significant in ADHD (range of OR: 1.04 to 1.49) and ASD (range of OR: 1.35 to 2.27). Teenage mothers, teenage fathers, and fathers ≥ 50 years had higher offspring risks of MDD (range of OR: 1.24 to 1.46); and teenage mothers and fathers ≥ 50 years had increased offspring risks of BD (range of OR: 1.23 to 1.87). Both paternal and maternal mental disorders were associated with higher risks of within-disorder transmission for ADHD, ASD, MDD, and BD (range of OR: 2.64 to 30.41). Besides, parents with one of these four mental disorders (ADHD, ASD, MDD, and BD) might have higher risk of cross-disorder transmission to at least one of the other three mental disorders in the offspring (range of OR: 1.35 to 7.15). Parental age and mental disorders had complex and nuanced patterns in association with offspring mental disorders.
Similar content being viewed by others
References
WHO (2014) Health for the World’s Adolescents—a second chance in the second decade. World Health Organisation; Geneva, Switzerland
Erskine HE, Moffitt TE, Copeland WE, Costello EJ, Ferrari AJ, Patton G, Degenhardt L, Vos T, Whiteford HA, Scott JG (2015) A heavy burden on young minds: the global burden of mental and substance use disorders in children and youth. Psychol Med 45(7):1551–1563. https://doi.org/10.1017/S0033291714002888
Erskine HE, Ferrari AJ, Polanczyk GV, Moffitt TE, Murray CJ, Vos T, Whiteford HA, Scott JG (2014) The global burden of conduct disorder and attention-deficit/hyperactivity disorder in 2010. J Child Psychol Psychiatry 55(4):328–336. https://doi.org/10.1111/jcpp.12186
Nock MK, Green JG, Hwang I, McLaughlin KA, Sampson NA, Zaslavsky AM, Kessler RC (2013) Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiat 70(3):300–310. https://doi.org/10.1001/2013.jamapsychiatry.55
Halfon N, Labelle R, Cohen D, Guile JM, Breton JJ (2013) Juvenile bipolar disorder and suicidality: a review of the last 10 years of literature. Eur Child Adolesc Psychiatry 22(3):139–151. https://doi.org/10.1007/s00787-012-0328-z
D’Onofrio BM, Rickert ME, Frans E, Kuja-Halkola R, Almqvist C, Sjolander A, Larsson H, Lichtenstein P (2014) Paternal age at childbearing and offspring psychiatric and academic morbidity. JAMA Psychiat 71(4):432–438. https://doi.org/10.1001/jamapsychiatry.2013.4525
de Kluiver H, Buizer-Voskamp JE, Dolan CV, Boomsma DI (2017) Paternal age and psychiatric disorders: a review. Am J Med Genet B Neuropsychiatr Genet 174(3):202–213. https://doi.org/10.1002/ajmg.b.32508
Sandin S, Hultman CM, Kolevzon A, Gross R, MacCabe JH, Reichenberg A (2012) Advancing maternal age is associated with increasing risk for autism: a review and meta-analysis. J Am Acad Child Adolesc Psychiatry 51(5):477–486. https://doi.org/10.1016/j.jaac.2012.02.018
Tearne JE (2015) Older maternal age and child behavioral and cognitive outcomes: a review of the literature. Fertil Steril 103(6):1381–1391. https://doi.org/10.1016/j.fertnstert.2015.04.027
McGrath JJ, Petersen L, Agerbo E, Mors O, Mortensen PB, Pedersen CB (2014) A comprehensive assessment of parental age and psychiatric disorders. JAMA Psychiat 71(3):301–309. https://doi.org/10.1001/jamapsychiatry.2013.4081
van Santvoort F, Hosman CM, Janssens JM, van Doesum KT, Reupert A, van Loon LM (2015) The impact of various parental mental disorders on children’s diagnoses: a systematic review. Clin Child Fam Psychol Rev 18(4):281–299. https://doi.org/10.1007/s10567-015-0191-9
Chen MH, Pan TL, Huang KL, Hsu JW, Bai YM, Su TP, Li CT, Tsai SJ, Cheng CM, Chen TJ (2019) Coaggregation of major psychiatric disorders in first-degree relatives of individuals with attention-deficit/hyperactivity disorder: a nationwide population-based study. J Clin Psychiatry. https://doi.org/10.4088/JCP.18m12371
Wang HE, Cheng CM, Bai YM, Hsu JW, Huang KL, Su TP, Tsai SJ, Li CT, Chen TJ, Leventhal BL, Chen MH (2020) Familial coaggregation of major psychiatric disorders in first-degree relatives of individuals with autism spectrum disorder: a nationwide population-based study. Psychol Med. https://doi.org/10.1017/S0033291720003207
Cheng CM, Chang WH, Chen MH, Tsai CF, Su TP, Li CT, Tsai SJ, Hsu JW, Huang KL, Lin WC, Chen TJ, Bai YM (2018) Co-aggregation of major psychiatric disorders in individuals with first-degree relatives with schizophrenia: a nationwide population-based study. Mol Psychiatry 23(8):1756–1763. https://doi.org/10.1038/mp.2017.217
Chen MH, Hsu JW, Huang KL, Bai YM, Ko NY, Su TP, Li CT, Lin WC, Tsai SJ, Pan TL, Chang WH, Chen TJ (2018) Sexually transmitted infection among adolescents and young adults with attention-deficit/hyperactivity disorder: a nationwide longitudinal study. J Am Acad Child Adolesc Psychiatry 57(1):48–53. https://doi.org/10.1016/j.jaac.2017.09.438
Liang CS, Bai YM, Hsu JW, Huang KL, Ko NY, Chu HT, Yeh TC, Tsai SJ, Chen TJ, Chen MH (2020) the risk of sexually transmitted infections following first-episode schizophrenia among adolescents and young adults: a cohort study of 220 545 subjects. Schizophr Bull. https://doi.org/10.1093/schbul/sbz126
Huang JS, Yang FC, Chien WC, Yeh TC, Chung CH, Tsai CK, Tsai SJ, Yang SS, Tzeng NS, Chen MH, Liang CS (2021) Risk of substance use disorder and its associations with comorbidities and psychotropic agents in patients with autism. JAMA Pediatr 175(2):e205371. https://doi.org/10.1001/jamapediatrics.2020.5371
Rai D, Lewis G, Lundberg M, Araya R, Svensson A, Dalman C, Carpenter P, Magnusson C (2012) Parental socioeconomic status and risk of offspring autism spectrum disorders in a Swedish population-based study. J Am Acad Child Adolesc Psychiatry 51(5):467–476. https://doi.org/10.1016/j.jaac.2012.02.012
Lauritsen MB, Astrup A, Pedersen CB, Obel C, Schendel DE, Schieve L, Yeargin-Allsopp M, Parner ET (2014) Urbanicity and autism spectrum disorders. J Autism Dev Disord 44(2):394–404. https://doi.org/10.1007/s10803-013-1875-y
Russell G, Ford T, Rosenberg R, Kelly S (2014) The association of attention deficit hyperactivity disorder with socioeconomic disadvantage: alternative explanations and evidence. J Child Psychol Psychiatry 55(5):436–445. https://doi.org/10.1111/jcpp.12170
Hultman CM, Sandin S, Levine SZ, Lichtenstein P, Reichenberg A (2011) Advancing paternal age and risk of autism: new evidence from a population-based study and a meta-analysis of epidemiological studies. Mol Psychiatry 16(12):1203–1212. https://doi.org/10.1038/mp.2010.121
Janecka M, Hansen SN, Modabbernia A, Browne HA, Buxbaum JD, Schendel DE, Reichenberg A, Parner ET, Grice DE (2019) Parental age and differential estimates of risk for neuropsychiatric disorders: findings from the Danish birth cohort. J Am Acad Child Adolesc Psychiatry 58(6):618–627. https://doi.org/10.1016/j.jaac.2018.09.447
Chudal R, Joelsson P, Gyllenberg D, Lehti V, Leivonen S, Hinkka-Yli-Salomaki S, Gissler M, Sourander A (2015) Parental age and the risk of attention-deficit/hyperactivity disorder: a nationwide, population-based cohort study. J Am Acad Child Adolesc Psychiatry 54(6):487–494. https://doi.org/10.1016/j.jaac.2015.03.013
Hvolgaard Mikkelsen S, Olsen J, Bech BH, Obel C (2017) Parental age and attention-deficit/hyperactivity disorder (ADHD). Int J Epidemiol 46(2):409–420. https://doi.org/10.1093/ije/dyw073
Chang Z, Lichtenstein P, D’Onofrio BM, Almqvist C, Kuja-Halkola R, Sjolander A, Larsson H (2014) Maternal age at childbirth and risk for ADHD in offspring: a population-based cohort study. Int J Epidemiol 43(6):1815–1824. https://doi.org/10.1093/ije/dyu204
Polanczyk G, de Lima MS, Horta BL, Biederman J, Rohde LA (2007) The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry 164(6):942–948. https://doi.org/10.1176/ajp.2007.164.6.942
Youngstrom EA, Birmaher B, Findling RL (2008) Pediatric bipolar disorder: validity, phenomenology, and recommendations for diagnosis. Bipolar Disord 10(1 Pt 2):194–214. https://doi.org/10.1111/j.1399-5618.2007.00563.x
Goldstein BI (2012) Recent progress in understanding pediatric bipolar disorder. Arch Pediatr Adolesc Med 166(4):362–371. https://doi.org/10.1001/archpediatrics.2011.832
Cross-Disorder Group of the Psychiatric Genomics Consortium. Electronic address pmhe, Cross-Disorder Group of the Psychiatric Genomics C (2019) Genomic relationships, novel loci, and pleiotropic mechanisms across eight psychiatric disorders. Cell 179(7):1469–1482. https://doi.org/10.1016/j.cell.2019.11.020
Andersen CH, Thomsen PH, Nohr EA, Lemcke S (2018) Maternal body mass index before pregnancy as a risk factor for ADHD and autism in children. Eur Child Adolesc Psychiatry 27(2):139–148. https://doi.org/10.1007/s00787-017-1027-6
Moreno D, Moreno-Iniguez M, Vigil D, Castro-Fornieles J, Ortuno F, Gonzalez-Pinto A, Parellada M, Baeza I, Otero S, Graell M, Aldama A, Arango C (2009) Obstetric complications as a risk factor for first psychotic episodes in childhood and adolescence. Eur Child Adolesc Psychiatry 18(3):180–184. https://doi.org/10.1007/s00787-008-0692-x
Laucht M, Esser G, Schmidt MH (1994) Parental mental disorder and early child development. Eur Child Adolesc Psychiatry 3(3):125–137. https://doi.org/10.1007/BF02720321
Grinde B, Tambs K (2016) Effect of household size on mental problems in children: results from the Norwegian Mother and Child Cohort study. BMC Psychol 4(1):31. https://doi.org/10.1186/s40359-016-0136-1
Wilson CE, Gillan N, Spain D, Robertson D, Roberts G, Murphy CM, Maltezos S, Zinkstok J, Johnston K, Dardani C, Ohlsen C, Deeley PQ, Craig M, Mendez MA, Happe F, Murphy DG (2013) Comparison of ICD-10R, DSM-IV-TR and DSM-5 in an adult autism spectrum disorder diagnostic clinic. J Autism Dev Disord 43(11):2515–2525. https://doi.org/10.1007/s10803-013-1799-6
Funding
The study was supported by grant from Taipei Veterans General Hospital (V106B-020, V107B-010, V107C-181, V107C-052) and Ministry of Science and Technology, Taiwan (107–2314-B-075–063-MY3). The funding source had no role in any process of study.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
None of the authors had any conflicts of interest related to this study.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Liang, CS., Bai, YM., Hsu, JW. et al. Associations of parental mental disorders and age with childhood mental disorders: a population-based cohort study with four million offspring. Eur Child Adolesc Psychiatry 32, 825–833 (2023). https://doi.org/10.1007/s00787-021-01914-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-021-01914-3