Abstract
Objective
This randomized clinical trial aimed to compare the efficacy of an oral irrigator and an interdental brush in patients with peri-implant mucositis clinically and biochemically at different time points (at baseline and at the 2nd, 4th, and 12th weeks).
Materials and methods
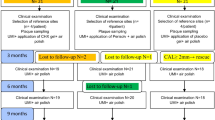
Forty-five patients with at least one implant with peri-implant mucositis were included in the present study (n = 45). The patients were divided into three groups: oral irrigator + toothbrush (OI group, n = 15), interdental brush + toothbrush (IB group, n = 15), and toothbrush only (control) (C group, n = 15). The modified plaque index (mPlI), modified sulcus bleeding index (mSBI), probing pocket depth (PPD), probing attachment level (PAL), and bleeding on probing (BOP) were recorded at baseline and at the 2nd, 4th, and 12th weeks. The levels of interleukin 1 beta (IL-1β), transforming growth factor-beta (TGF-β), tissue-type plasminogen activator (t-PA), and plasminogen activator inhibitor-1 (PAI-1) were also determined in the peri-implant crevicular fluid samples biochemically.
Results
The mSBI and t-PA at the 2nd week (p = 0.003; p = 0.003); the mPlI, mSBI, BOP, t-PA, and PAI-1 at the 4th week (p < 0.05; p < 0.001; p < 0.001; p = 0.015; p = 0.011); and the mPlI, mSBI, IL-1β, t-PA, and PAI-1 at the 12th week (p < 0.05; p < 0.001; p = 0.013; p < 0.001; p = 0.002) were significantly lower in the OI group compared with those in the C group. Meanwhile, PAI-1 at the 2nd week, mSBI at the 4th week, and t-PA at the 12th week were significantly lower in the OI group compared with those in the IB group (p < 0.001; p = 0.011; p = 0.003). At the 2nd, 4th, and 12th weeks, all other parameters were not statistically different in the three groups.
Conclusion
The clinical indexes (such as mSBI and BOP) that play an important role in the diagnosis of peri-implant mucositis showed the lowest means (although limited) in the OI group at all evaluation time points. Moreover, when the clinical and biochemistry results were interpreted altogether, it became apparent that the OI group exhibited similar or more effective results than the IB group in resolving peri-implant mucositis. In light of the foregoing, this study concluded that the use of an oral irrigator can be as effective as an interdental brush in interdental cleaning.
Clinical relevance
In this study, it is suggested that the regular use of an oral irrigator along with a toothbrush could be an appropriate alternative to other oral hygiene products such as dental floss and interdental brush for the management of peri-implant mucositis by preventing the accumulation of dental plaque (NCT03844035).




Similar content being viewed by others
References
Klinge B, Klinge A, Bertl K, Stavropoulos A (2018) Peri-implant diseases. Eur J Oral Sci 126 Suppl 1:88–94. https://doi.org/10.1111/eos.12529
Belibasakis GN (2014) Microbiological and immuno-pathological aspects of peri-implant diseases. Arch Oral Biol 59(1):66–72. https://doi.org/10.1016/j.archoralbio.2013.09.013
Ioannidis A, Thurnheer T, Hofer D, Sahrmann P, Guggenheim B, Schmidlin PR (2015) Mechanical and hydrodynamic homecare devices to clean rough implant surfaces - an in vitro polyspecies biofilm study. Clin Oral Implants Res 26(5):523–528. https://doi.org/10.1111/clr.12436
Noorlin I, Watts TL (2007) A comparison of the efficacy and ease of use of dental floss and interproximal brushes in a randomised split mouth trial incorporating an assessment of subgingival plaque. Oral Health Prev Dent 5(1):13–18
Rasines G (2009) The use of interdental brushes along with toothbrushing removes most plaque. Evid Based Dent 10(3):74. https://doi.org/10.1038/sj.ebd.6400666
Rosema NA, Hennequin-Hoenderdos NL, Berchier CE, Slot DE, Lyle DM, van der Weijden GA (2011) The effect of different interdental cleaning devices on gingival bleeding. J Int Acad Periodontol 13(1):2–10
Kotsakis GA, Lian Q, Ioannou AL, Michalowicz BS, John MT, Chu H (2018) A network meta-analysis of interproximal oral hygiene methods in the reduction of clinical indices of inflammation. J Periodontol 89(5):558–570. https://doi.org/10.1002/jper.17-0368
Lyle DM (2011) Use of a water flosser for interdental cleaning. Compend Contin Educ Dent 32(9):78 80–72
Jahn CA (2010) The dental water jet: a historical review of the literature. J Dent Hyg 84(3):114–120
Sharma PK, Gibcus MJ, van der Mei HC, Busscher HJ (2005) Influence of fluid shear and microbubbles on bacterial detachment from a surface. Appl Environ Microbiol 71(7):3668–3673
Newman MG, Flemmig TF, Nachnani S, Rodrigues A, Calsina G, Lee YS, de Camargo P, Doherty FM, Bakdash MB (1990) Irrigation with 0.06% chlorhexidine in naturally occurring gingivitis. II. 6 months microbiological observations. J Periodontol 61(7):427–433. https://doi.org/10.1902/jop.1990.61.7.427
Cutler CW, Stanford TW, Abraham C, Cederberg RA, Boardman TJ, Ross C (2000) Clinical benefits of oral irrigation for periodontitis are related to reduction of pro-inflammatory cytokine levels and plaque. J Clin Periodontol 27(2):134–143. https://doi.org/10.1034/j.1600-051x.2000.027002134.x
Barnes CM, Russell CM, Reinhardt RA, Payne JB, Lyle DM (2005) Comparison of irrigation to floss as an adjunct to tooth brushing: effect on bleeding, gingivitis, and supragingival plaque. J Clin Dent 16(3):71–77
Al-Mubarak S, Ciancio S, Aljada A, Mohanty P, Ross C, Dandona P (2002) Comparative evaluation of adjunctive oral irrigation in diabetics. J Clin Periodontol 29(4):295–300. https://doi.org/10.1034/j.1600-051x.2002.290404.x
Bunk D, Eisenburger M, Häckl S, Eberhard J, Stiesch M, Grischke J (2020) The effect of adjuvant oral irrigation on self-administered oral care in the management of peri-implant mucositis: a randomized controlled clinical trial. Clin Oral Implants Res 31(10):946–958. https://doi.org/10.1111/clr.13638
Salles MM, Oliveira VC, Macedo AP, do Nascimento C, Silva-Lovato CH, Paranhos HFO (2021) Brushing associated with oral irrigation in maintaining implants and overdentures hygiene - a randomized clinical trial. Odontology 109(1):284–294. https://doi.org/10.1007/s10266-020-00543-7
Salles MM, Oliveira VC, Macedo AP, Silva-Lovato CH, Oliveira Paranhos HF (2020)Effectiveness of brushing associated with oral irrigation in maintenance of peri-implant tissues and overdentures: clinical parameters and patient satisfaction. J Oral Implantol.https://doi.org/10.1563/aaid-joi-D-19-00092
Aboyoussef H, Carter C, Jandinski JJ, Panagakos FS (1998) Detection of prostaglandin E2 and matrix metalloproteinases in implant crevicular fluid. Int J Oral Maxillofac Implants 13(5):689–696
Buduneli N, Buduneli E, Kardeşler L, Lappin D, Kinane DF (2005) Plasminogen activator system in smokers and non-smokers with and without periodontal disease. J Clin Periodontol 32(4):417–424. https://doi.org/10.1111/j.1600-051X.2005.00694.x
Aykol G, Baser U, Maden I, Kazak Z, Onan U, Tanrikulu-Kucuk S, Ademoglu E, Issever H, Yalcin F (2011) The effect of low-level laser therapy as an adjunct to non-surgical periodontal treatment. J Periodontol 82(3):481–488. https://doi.org/10.1902/jop.2010.100195
Sarajlic J, Agis H, Kandler B, Watzek G, Gruber R (2007) Plasminogen activation by fibroblasts from periodontal ligament and gingiva is not directly affected by chemokines in vitro. Arch Oral Biol 52(7):663–668. https://doi.org/10.1016/j.archoralbio.2006.12.020
Tatakis DN (1993) Interleukin-1 and bone metabolism: a review. J Periodontol 64(5 Suppl):416–431
Gürkan A, Emingil G, Cinarcik S, Berdeli A (2006) Gingival crevicular fluid transforming growth factor-beta1 in several forms of periodontal disease. Arch Oral Biol 51(10):906–912. https://doi.org/10.1016/j.archoralbio.2006.04.008
Ghosh AK, Vaughan DE (2012) PAI-1 in tissue fibrosis. J Cell Physiol 227(2):493–507. https://doi.org/10.1002/jcp.22783
Kinnby B (2002) The plasminogen activating system in periodontal health and disease. Biol Chem 383(1):85–92. https://doi.org/10.1515/bc.2002.008
Ghassib I, Chen Z, Zhu J, Wang HL (2019) Use of IL-1 β, IL-6, TNF-α, and MMP-8 biomarkers to distinguish peri-implant diseases: a systematic review and meta-analysis. Clin Implant Dent Relat Res 21(1):190–207. https://doi.org/10.1111/cid.12694
Faot F, Nascimento GG, Bielemann AM, Campão TD, Leite FR, Quirynen M (2015) Can peri-implant crevicular fluid assist in the diagnosis of peri-implantitis? A systematic review and meta-analysis. J Periodontol 86(5):631–645. https://doi.org/10.1902/jop.2015.140603
Hall J, Pehrson NG, Ekestubbe A, Jemt T, Friberg B (2015) A controlled, cross-sectional exploratory study on markers for the plasminogen system and inflammation in crevicular fluid samples from healthy, mucositis and peri-implantitis sites. Eur J Oral Implantol 8(2):153–166
Berglundh T, Armitage G, Araujo MG, Avila-Ortiz G, Blanco J, Camargo PM, Chen S, Cochran D, Derks J, Figuero E (2018) Peri-implant diseases and conditions: consensus report of workgroup 4 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Periodontol 89:S313–S318
Renvert S, Persson GR, Pirih FQ, Camargo PM (2018) Peri-implant health, peri-implant mucositis, and peri-implantitis: case definitions and diagnostic considerations. J Periodontol 89 Suppl 1:S304-s312. https://doi.org/10.1002/jper.17-0588
Mombelli A, van Oosten MA, Schurch E Jr, Land NP (1987) The microbiota associated with successful or failing osseointegrated titanium implants. Oral Microbiol Immunol 2(4):145–151. https://doi.org/10.1111/j.1399-302x.1987.tb00298.x
Ainamo J, Bay I (1975) Problems and proposals for recording gingivitis and plaque. Int Dent J 25(4):229–235
Ohrn K, Sanz M (2009) Prevention and therapeutic approaches to gingival inflammation. J Clin Periodontol 36 Suppl 10:20–26. https://doi.org/10.1111/j.1600-051X.2009.01418.x
Javed F, BinShabaib MS, Alharthi SS, Qadri T (2017) Role of mechanical curettage with and without adjunct antimicrobial photodynamic therapy in the treatment of peri-implant mucositis in cigarette smokers: a randomized controlled clinical trial. Photodiagnosis Photodyn Ther 18:331–334. https://doi.org/10.1016/j.pdpdt.2017.04.015
Lainson PA, Bergquist JJ, Fraleigh CM (1972) A longitudinal study of pulsating water pressure cleansing devices. J Periodontol 43(7):444–446. https://doi.org/10.1902/jop.1972.43.7.444
Flemmig TF, Newman MG, Doherty FM, Grossman E, Meckel AH, Bakdash MB (1990) Supragingival irrigation with 0.06% chlorhexidine in naturally occurring gingivitis I. 6 month clinical observations. J Periodontol 61(2):112–117. https://doi.org/10.1902/jop.1990.61.2.112
Meklas JF, Stewart JL (1972) Investigation of the safety and effectiveness of an oral irrigating device. J Periodontol 43(7):441–443. https://doi.org/10.1902/jop.1972.43.7.441
Walsh M, Heckman B, Leggott P, Armitage G, Robertson PB (1989) Comparison of manual and power toothbrushing, with and without adjunctive oral irrigation, for controlling plaque and gingivitis. J Clin Periodontol 16(7):419–427. https://doi.org/10.1111/j.1600-051x.1989.tb01670.x
Brownstein CN, Briggs SD, Schweitzer KL, Briner WW, Kornman KS (1990) Irrigation with chlorhexidine to resolve naturally occurring gingivitis A methodologic study. J Clin Periodontol 17(8):588–593
Newman MG, Cattabriga M, Etienne D, Flemmig T, Sanz M, Kornman KS, Doherty F, Moore DJ, Ross C (1994) Effectiveness of adjunctive irrigation in early periodontitis: multi-center evaluation. J Periodontol 65(3):224–229. https://doi.org/10.1902/jop.1994.65.3.224
Magnuson B, Harsono M, Stark PC, Lyle D, Kugel G, Perry R (2013) Comparison of the effect of two interdental cleaning devices around implants on the reduction of bleeding: a 30-day randomized clinical trial. Compend Contin Educ Dent 34 Spec No 8:2–7
Masada MP, Persson R, Kenney JS, Lee SW, Page RC, Allison AC (1990) Measurement of interleukin-1 alpha and -1 beta in gingival crevicular fluid: implications for the pathogenesis of periodontal disease. J Periodontal Res 25(3):156–163. https://doi.org/10.1111/j.1600-0765.1990.tb01038.x
Engebretson SP, Grbic JT, Singer R, Lamster IB (2002) GCF IL-1beta profiles in periodontal disease. J Clin Periodontol 29(1):48–53. https://doi.org/10.1034/j.1600-051x.2002.290108.x
Stashenko P, Jandinski JJ, Fujiyoshi P, Rynar J, Socransky SS (1991) Tissue levels of bone resorptive cytokines in periodontal disease. J Periodontol 62(8):504–509. https://doi.org/10.1902/jop.1991.62.8.504
Engebretson SP, Lamster IB, Herrera-Abreu M, Celenti RS, Timms JM, Chaudhary AG, di Giovine FS, Kornman KS (1999) The influence of interleukin gene polymorphism on expression of interleukin-1beta and tumor necrosis factor-alpha in periodontal tissue and gingival crevicular fluid. J Periodontol 70(6):567–573. https://doi.org/10.1902/jop.1999.70.6.567
Panagakos FS, Aboyoussef H, Dondero R, Jandinski JJ (1996) Detection and measurement of inflammatory cytokines in implant crevicular fluid: a pilot study. Int J Oral Maxillofac Implants 11(6):794–799
Ataoglu H, Alptekin NO, Haliloglu S, Gursel M, Ataoglu T, Serpek B, Durmus E (2002) Interleukin-1β, tumor necrosis factor-α levels and neutrophil elastase activity in peri-implant crevicular fluid: Correlation with clinical parameters and effect of smoking. Clin Oral Implant Res 13(5):470–476
Tsalikis L, Parapanisiou E, Bata-Kyrkou A, Polymenides Z, Konstantinidis A (2002) Crevicular fluid levels of interleukin-1alpha and interleukin-1beta during experimental gingivitis in young and old adults. J Int Acad Periodontol 4(1):5–11
Schierano G, Pejrone G, Brusco P, Trombetta A, Martinasso G, Preti G, Canuto RA (2008) TNF-alpha TGF-beta2 and IL-1beta levels in gingival and peri-implant crevicular fluid before and after de novo plaque accumulation. J Clin Periodontol 35(6):532–538. https://doi.org/10.1111/j.1600-051X.2008.01224.x
Border WA, Noble NA (1994) Transforming growth factor beta in tissue fibrosis. N Engl J Med 331(19):1286–1292. https://doi.org/10.1056/nejm199411103311907
Kinnby B, Matsson L, Lecander I (1994) The plasminogen-activating system in gingival fluid from adults.: An intra-individual study before and after treatment of gingivitis. Eur J Oral Sci 102(6):334–341. https://doi.org/10.1111/j.1600-0722.1994.tb01480.x
Yin X, Bunn CL, Bartold PM (2000) Detection of tissue plasminogen activator (t-PA) and plasminogen activator inhibitor 2(PAI-2) in gingival crevicular fluid from healthy, gingivitis and periodontitis patients. J Clin Periodontol 27(3):149–156. https://doi.org/10.1034/j.1600-051x.2000.027003149.x
Olofsson A, Lindberg P, Lanke J, Matsson L, Kinnby B (2003) Relationship between fibrinolytic activity and gingival inflammatory reaction in young individuals. J Periodontal Res 38(1):104–108. https://doi.org/10.1034/j.1600-0765.2003.01370.x
Papadimitriou S, Tsantarliotou M, Makris G, Papaioannou N, Batzios C, Kokolis N, Dessiris A (2006) A clinical study of plasminogen activator activity in gingival tissue in dogs with gingivitis and periodontitis. Res Vet Sci 80(2):189–193. https://doi.org/10.1016/j.rvsc.2005.06.002
Bizzarro S, Van Der Velden U, Ten Heggeler JM, Leivadaros E, Hoek FJ, Gerdes VE, Bakker SJ, Gans RO, Ten Cate H, Loos BG (2007) Periodontitis is characterized by elevated PAI-1 activity. J Clin Periodontol 34(7):574–580
Funding
This study was supported by the Ondokuz Mayis Research Fund (Project number: PYO.DIS.1904.14.006).
Author information
Authors and Affiliations
Contributions
All authors have made substantial contributions to the conception and design of the study. S.T. and B.O.C. have been involved in data collection and B.A. has been involved in data analysis. F.P., G.C.K., and S.K.B. have been involved in data interpretation and drafting of the manuscript. M.L. has been involved in revising it critically and has given the final approval of the version to be published.
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study was approved by the ethics committee (Human Ethical Committee of Ondokuz Mayis University, protocol no: 2014/644).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tütüncüoğlu, S., Cetinkaya, B.O., Pamuk, F. et al. Clinical and biochemical evaluation of oral irrigation in patients with peri-implant mucositis: a randomized clinical trial. Clin Oral Invest 26, 659–671 (2022). https://doi.org/10.1007/s00784-021-04044-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-021-04044-x