Abstract
Objective
To evaluate the effects of adjunctive delivery of a sodium hypochlorite gel in the treatment of peri-implant mucositis (PM).
Materials and methods
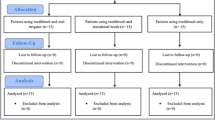
Forty-six subjects with 68 implants diagnosed with PM were randomly assigned to two treatment groups. Prior to mechanical debridement, a sodium hypochlorite gel was delivered to the implants of the test group while implants of the control group received a placebo gel. Application of both test and placebo gels was repeated 5 times at baseline. The primary outcome variable was the change in pocket probing depth (PPD) between baseline and 6 months.
Results
After 6 months, the mean PPD decreased statistically significantly from 3.93 ± 1.09 mm to 3.04 ± 0.46 mm in the test (p = 0.0001) and from 3.68 ± 0.85 mm to 3.07 ± 0.58 mm in the control (p = 0.0001) group, respectively. No statistically significant difference (p = 0.53) was observed with respect to PPD changes from baseline to 6 months between test (0.88 ± 1.04 mm) and control group (0.61 ± 0.75 mm), respectively. The number of implants with bleeding on probing (BoP) decreased statistically significantly from 33 to 18 in the test group (p = 0.0001) and from 34 to 23 in the control group (p = 0.0001) after 6 months.
Conclusions
In conclusion and within the limits of the present study, changes in PPD from baseline to 6 months were not statistically significantly different between groups. Complete resolution of mucosal inflammation was not achieved with either of the therapies.
Clinical relevance
The present outcomes have showed that a complete resolution of peri-implant mucositis is not possible to obtain by means mechanical debridement with or without a sodium hypochlorite gel application.






Similar content being viewed by others
References
Heitz-Mayfield LJ, Salvi GE (2018) Peri-implant mucositis. J Clin Periodontol 45(suppl 20):s237–s245. https://doi.org/10.1111/jcpe.12953
Pontoriero R, Tonelli MP, Carnevale G, Mombelli A, Nyman SR, Lang NP (1994) Experimentally induced peri-implant mucositis. A clinical study in humans. Clin Oral Implants Res 5:254–259
Zitzmann NU, Berglundh T, Marinello C, Lindhe J (2001) Experimental peri-implant mucositis in man. J Clin Periodontol 28:517–523. https://doi.org/10.1034/j.1600-051x.2001.028006517.x
Salvi GE, Aglietta M, Eick S, Sculean A, Lang NP, Ramseier CA (2012) Reversibility of experimental peri-implant mucositis compared with experimental gingivitis in humans. Clin Oral Implants Res 23:182–190. https://doi.org/10.1111/j.1600-0501.2011.02220.x
Meyer S, Giannopoulou C, Courvoisier D, Schimmel M, Müller F, Mombelli A (2017) Experimental mucositis and experimental gingivitis in persons aged 70 or over. Clinical and biological responses. Clin Oral Implants Res 28:1005–1012. https://doi.org/10.1111/clr.12912
Porras R, Anderson GB, Caffesse R, Narendran S, Trejo PM (2002) Clinical response to 2 different therapeutic regimens to treat peri-implant mucositis. J Periodontol 73:1118–1125
Maximo MB, de Mendonca AC, Renata Santos V, Figuereido LC, Feres M, Duarte PM (2009) Short-term clinical and microbiological evaluations of peri-implant diseases before and after mechanical anti-infective therapies. Clinl Oral Implants Res 20:99–108. https://doi.org/10.1111/j.1600-0501.2008.01618.x
Ramberg P, Lindhe J, Botticelli D, Botticelli A (2009) The effect of a triclosan dentifrice on mucositis in subjects with dental implants: a six-month clinical study. J Clin Dent 20:103–107
Thöne-Mühling M, Swierkot K, Nonnenmacher C, Mutters R, Flores-de-Jacoby L, Mengel R (2010) Comparison of two full-mouth approaches in the treatment of peri-implant mucositis: a pilot study. Clin Oral Implants Res 21:504–512. https://doi.org/10.1111/j.1600-0501.2009.01861.x
Hallström H, Persson GR, Lindgren S, Olofsson M, Renvert S (2012) Systemic antibiotics and debridement of peri-implant mucositis. A randomized clinical trial. J Clin Periodontol 39:574–581. https://doi.org/10.1111/j.1600-051X.2012.01884.x
De Siena F, Francetti L, Corbella S, Taschieri S, Del Fabbro M (2013) Topical application of 1% chlorhexidine gel versus 0.2% mouthwash in the treatment of peri-implant mucositis. An observational study. Int J Dent Hyg 11:41–47. https://doi.org/10.1111/idh.12002
Riben-Grundström C, Norderyd O, Andrè U, Renvert S (2015) Treatment of peri-implant mucositis using a glycine powder air-polishing or ultrasonic device: a randomized clinical trial. J Clin Periodontol 42:462–469. https://doi.org/10.1111/jcpe.12395
Heitz-Mayfield LJ, Salvi GE, Botticelli D, Mombelli A, Faddy M, Lang NP, Implant Complication Research Group (2011) Anti-infective treatment of peri-implant mucositis: a randomized controlled clinical trial. Clin Oral Implants Res 22:237–241. https://doi.org/10.1111/j.1600-0501.2010.02078.x
Costa FO, Takenaka-Martines S, Cota LO, Ferreira SD, Silva GL, Costa JE (2012) Peri-implant disease in subjects with and without preventive maintenance: a 5-year follow-up. J Clin Periodontol 39:173–181. https://doi.org/10.1111/j.1600-051x.2011.01819.x
Jurczyk K, Nietzsche S, Ender C, Sculean A, Eick S (2016) In-vitro activity of sodium-hypochlorite gel on bacteria associated with periodontitis. Clin Oral Investig 20:2165–2173. https://doi.org/10.1007/s00784-016-1711-9
Roos-Jansåker AM, Almhöjd US, Jansson H (2017) Treatment of peri-implantitis: clinical outcome of chloramine as an adjunctive to non-surgical therapy: a randomized clinical trial. Clin Oral Implants Res 28:43–48. https://doi.org/10.1111/clr.12612
Zitzmann NU, Berglundh T (2008) Definition and prevalence of peri-implant diseases. J Clin Periodontol 35:286–291. https://doi.org/10.1111/j.1600-051X.2008.01274.x
Lindhe J, Meyle J (2008) Peri-implant diseases: consensus report of the Sixth European Workshop on Periodontology. J Clin Periodontol 35:282–285. https://doi.org/10.1111/j.1600-051X.2008.01283.x
Silness J, Löe H (1964) Periodontal disease in pregnancy. II. Correlation between oral hygiene and periodontal condition. Acta Odontol Scand 22:121–135
Mombelli A, van Oosten MAC, Schürch E, Lang NP (1987) The microbiota associated with successful or failing osseointegrated titanium implants. Oral Microbiol Immunol 2:145–151
Lang NP, Joss A, Orsanic T, Gusberti FA, Siegrist BE (1986) Bleeding on probing. A predictor for the progression of periodontal disease? J Clin Periodontol 13:590–596
O’Leary TJ, Drake RB, Naylor JE (1972) The plaque control record. J Periodontol 43:38
Claffey N, Nylund K, Kiger R, Garrett S, Egelberg J (1990) Diagnostic predictability of scores of plaque, bleeding, suppuration and probing depth for probing attachment loss. 3 1/2 years of observation following initial periodontal therapy. J Clin Periodontol 17:108–114
Ciancio SG, Lauciello F, Shibly O, Vitello M, Mather M (1995) The effect of an antiseptic mouthrinse on implant mainteinance: plaque and peri-implant gingival tissue. J Periodontol 66:962–965
Felo A, Shibly O, Ciancio SG, Lauciello FR, Ho A (1997) Effect of subgingival chlorhexidine irrigation on peri-implant maintenance. Am J Dent 10:107–110
Ji YJ, Tang ZH, Wang R, Cao J, Jin LJ (2014) Effect of glycine powder air-polishing as an adjunct in the treatment of peri-implant mucositis: a pilot clinical trial. Clin Oral Implants Res 25:683–689
Hallström H, Lindgren S, Widen C, Renvert S, Twetman S (2016) Probiotic supplements and debridement of peri-implant mucositis: a randomized controlled trial. Acta Odontol Scand 74:60–66. https://doi.org/10.3109/00016357.2015.1040065
Galofré M, Palao D, Vicario M, Nart J, Violant D (2018) Clinical and microbiological evaluation of the effect of Lactobacillus reuteri in the treatment of mucositis and peri-implantitis: a triple-blind randomized clinical trial. J Periodontal Res 53:378–390. https://doi.org/10.1111/jre.12523
Salvi GE, Zitzmann NU (2014) The effects of anti-infective preventive measures on the occurrence of biologic implant complications and implant loss: a systematic review. Int J Oral Maxillofac Implants 29(suppl):292–307. https://doi.org/10.11607/jomi.2014suppl.g5.1.Review
Acknowledgments
The experimental materials used in the present study were provided by Regedent AG, Zürich, Switzerland.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Iorio-Siciliano, V., Blasi, A., Stratul, SI. et al. Anti-infective therapy of peri-implant mucositis with adjunctive delivery of a sodium hypochlorite gel: a 6-month randomized triple-blind controlled clinical trial. Clin Oral Invest 24, 1971–1979 (2020). https://doi.org/10.1007/s00784-019-03060-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-019-03060-2