Abstract
Objectives
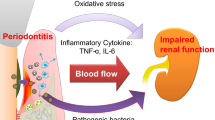
Several factors have been associated with hyperglycemia after kidney transplantation (KTx), including systemic inflammation. This study aimed to investigate the relationship between periodontal status and hyperglycemia in KTx patients.
Materials and methods
Forty-four KTx patients were included in this cross-sectional study. Periodontitis severity was categorized into stage I to IV. Fasting blood glucose (FBG) was measured, and hyperglycemia was analyzed at different FBG cutoff points (100 mg/dL, 110 mg/dL, 120 mg/dL, 126 mg/dL, 140 mg/dL). Age, history of smoking, prior type 2 diabetes (T2D), and prior cardiovascular disease (CVD) were considered cofounders. Multivariable logistic regression modelling was performed with periodontitis as the exposure and hyperglycemia as the outcome. Pathway analysis was performed with FBG as a continuous outcome.
Results
Periodontitis had increased odds of hyperglycemia from 120 mg/dL FBG cutoff, even after adjustment. In addition, periodontitis severity was positively associated with FBG level (β = 0.323, SE = 0.127, P = 0.011).
Conclusion
The findings suggest that periodontitis may be related to increase of hyperglycemia and FBG levels in KTx patients.
Clinical relevance
Periodontitis severity and cardiovascular disease were positively associated with FBG levels in KTx patients. Clinicians and patients should be aware of the potential benefit of periodontal care for better glycemic control management.


Similar content being viewed by others
References
Bikbov B, Levey PCA, AS, et al (2017) Global, regional, and national burden of chronic kidney disease, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 395:709–733. https://doi.org/10.1016/S0140-6736(20)30045-3
Jansz TT, Bonenkamp AA, Boereboom FT, Van Reekum FE, Verhaar MC, Van Jaarsveld BC (2018) Health-related quality of life compared between kidney transplantation and nocturnal hemodialysis. PLoS ONE 13:e0204405. https://doi.org/10.1371/journal.pone.0204405
Tonelli M, Wiebe N, Knoll G et al (2011) Systematic review: kidney transplantation compared with dialysis in clinically relevant outcomes. Am J Transplant 11:2093–2109. https://doi.org/10.1111/j.1600-6143.2011.03686.x
Hart A, Smith JM, Skeans MA et al (2019) OPTN/SRTR 2017 annual data report: kidney. Am J Transplant 19:19–123. https://doi.org/10.1111/ajt.15274
Martins SBS, Ferreira BA, Gonçalves VAC, De Marco R, De Lima MG, Medina-Pestana JO, Tedesco-Silva H (2019) Kidney allocation system for transplantation in Brazil. Cur Transplant Rep 6:209–213. https://doi.org/10.1007/s40472-019-00247-0
Galindo RJ, Wallia A (2016) Hyperglycemia and diabetes mellitus following organ transplantation. Cur Diab Rep 16:14. https://doi.org/10.1007/s11892-015-0707-1
Galindo RJ, Fried M, Breen T, Tamler R (2016) Hyperglycemia management in patients with posttransplantation diabetes. Endocr Pract 22:454–465. https://doi.org/10.4158/EP151039.RA
Sharif A, Baboolal K (2012) Complications associated with new-onset diabetes after kidney transplantation. Nat Rev Nephrol 8:34–42. https://doi.org/10.1038/nrneph.2011.174
Hecking M, Werzowa J, Haidinger M et al (2013) Novel views on new-onset diabetes after transplantation: development, prevention and treatment. Nephrol Dial Transplant 28:550–566. https://doi.org/10.1093/ndt/gfs583
Montero N, Pascual J (2015) Immunosuppression and post-transplant hyperglycemia. Cur Diab Rev 11:144–154. https://doi.org/10.2174/1573399811666150331160846
Chanchlani R, Kim SJ, Kim ED et al (2017) Incidence of hyperglycemia and diabetes and association with electrolyte abnormalities in pediatric solid organ transplant recipients. Nephrol Dial Transplant 32:1579–1586. https://doi.org/10.1093/ndt/gfx205
Cantarin MPM, Keith SW, Lin Z et al (2016) Association of inflammation prior to kidney transplantation with post-transplant diabetes mellitus. Cardiorenal Med 6:289–300. https://doi.org/10.1159/000446294
Reine TM, Kolseth IBM, Meen AJ et al (2015) Effects of restoring normoglycemia in type 1 diabetes on inflammatory profile and renal extracellular matrix structure after simultaneous pancreas and kidney transplantation. Diab Res Clin Pract 107:46–53. https://doi.org/10.1016/j.diabres.2014.10.006
Grossman A, Ayalon-Dangur I, Cooper L et al (2018) Association between anemia at three different time points and new-onset diabetes after kidney transplantation––a retrospective cohort study. Endocr Res 43:90–96. https://doi.org/10.1080/07435800.2017.1422516
Nunes-dos-Santos DL, Gomes SV, Rodrigues VP, Pereira AL (2020) Periodontal status and clinical outcomes in kidney transplant recipients: a systematic review. Oral Dis 26:22–34. https://doi.org/10.1111/odi.13040
Kinane DF, Stathopoulou PG, Papapanou PN (2017) Periodontal diseases Nat Rev Dis Prim 3:17038. https://doi.org/10.1038/nrdp.2017.38
Preshaw PM, Alba AL, Herrera D et al (2012) Periodontitis and diabetes: a two-way relationship. Diabetol 55:21–31. https://doi.org/10.1007/s00125-011-2342-y
Casanova L, Hughes FJ, Preshaw PM (2014) Diabetes and periodontal disease: a two-way relationship. Brit Dent J 217:433. https://doi.org/10.1038/sj.bdj.2014.907
Teeuw WJ, Gerdes VE, Loos BG (2010) Effect of periodontal treatment on glycemic control of diabetic patients: a systematic review and meta-analysis. Diab Care 33:421–427. https://doi.org/10.2337/dc09-1378
Cao R, Li Q, Wu Q, Yao M, Chen Y, Zhou H (2019) Effect of non-surgical periodontal therapy on glycemic control of type 2 diabetes mellitus: a systematic review and Bayesian network meta-analysis. BMC Oral Heal 19:176. https://doi.org/10.1186/s12903-019-0829-y
Teeuw WJ, Slot DE, Susanto H et al (2014) Treatment of periodontitis improves the atherosclerotic profile: a systematic review and meta-analysis. J Clin Periodontol 41:70–79. https://doi.org/10.1111/jcpe.12171
Simpson TC, Weldon JC, Worthington HV, et al (2015) Treatment of periodontal disease for glycaemic control in people with diabetes mellitus. Cochr Database Syst Rev 11:CD004714. https://doi.org/10.1002/14651858.CD004714.pub3
D’Aiuto F, Gkranias N, Bhowruth D et al (2018) Systemic effects of periodontitis treatment in patients with type 2 diabetes: a 12 month, single-centre, investigator-masked, randomised trial. Lancet Diab Endocrinol 6:954–965. https://doi.org/10.1016/S2213-8587(18)30038-X
Chen LP, Hsu SP, Peng YS, Chiang CK, Hung KY (2011) Periodontal disease is associated with metabolic syndrome in hemodialysis patients. Nephrol Dial Transplant 26:4068–4073. https://doi.org/10.1093/ndt/gfr209
Ainamo J, Bay I (1975) Problems and proposals for recording gingivitis and plaque. Int Dent J 25:229–235
Tonetti MS, Greenwell H, Kornman KS (2018) Staging and grading of periodontitis: framework and proposal of a new classification and case definition. J Periodontol 89:S159–S172. https://doi.org/10.1002/JPER.18-0006
Chang CC, Lee WT, Hsiao JR et al (2019) Oral hygiene and the overall survival of head and neck cancer patients. Canc Med 8:1854–1864. https://doi.org/10.1002/cam4.2059
Heldal TF, Ueland T, Jenssen T et al (2018) Inflammatory and related biomarkers are associated with post-transplant diabetes mellitus in kidney recipients: a retrospective study. Transplant Int 31:510–519. https://doi.org/10.1111/tri.13116
Kim YG, Ihm CG, Lee TW et al (2012) Association of genetic polymorphisms of interleukins with new-onset diabetes after transplantation in renal transplantation. Transplantat 93:900–907. https://doi.org/10.1097/TP.0b013e3182497534
Kim JS, Kim SK, Park JY et al (2016) Significant association between toll-like receptor gene polymorphisms and posttransplantation diabetes mellitus. Nephron 133:279–286. https://doi.org/10.1159/000446570
Wauters RP, Cosio FG, Fernandez MLS, Kudva Y, Shah P, Torres VE (2012) Cardiovascular consequences of new-onset hyperglycemia after kidney transplantation. Transplant 94:377–382. https://doi.org/10.1097/TP.0b013e3182584831
Kocher T, König J, Borgnakke WS, Pink C (2000) Meisel P (2018) Periodontal complications of hyperglycemia/diabetes mellitus: epidemiologic complexity and clinical challenge. Periodontol 78:59–97. https://doi.org/10.1111/prd.12235
Passoja A, Puijola I, Knuuttila M et al (2010) (2010) Serum levels of interleukin-10 and tumour necrosis factor-α in chronic periodontitis. J Clin Periodontol 37:881–887. https://doi.org/10.1111/j.1600-051X.2010.01602.x
Acharya AB, Thakur S, Muddapur MV, Kulkarni RD (2018) Systemic cytokines in type 2 diabetes mellitus and chronic periodontitis. Cur Diab Rev 14:182–188. https://doi.org/10.2174/1573399812666161220144011
Miranda TS, Heluy SL, Cruz DF et al (2019) (2019) The ratios of pro-inflammatory to anti-inflammatory cytokines in the serum of chronic periodontitis patients with and without type 2 diabetes and/or smoking habit. Clin Oral Inv 23:641–650. https://doi.org/10.1007/s00784-018-2471-5
Liu Z, Liu Y, Song Y, Zhang X, Wang S, Wang Z (2014) Systemic oxidative stress biomarkers in chronic periodontitis: a meta-analysis. Dis Mark 2014:931083. https://doi.org/10.1155/2014/931083
Żukowski P, Maciejczyk M, Waszkiel D (2018) Sources of free radicals and oxidative stress in the oral cavity. Arch Oral Biol 92:8–17. https://doi.org/10.1016/j.archoralbio.2018.04.018
Almerich-Silla JM, Pastor S, Serrano F, Puig-Silla M, Dasí F (2015) Oxidative stress parameters in saliva and its association with periodontal disease and types of bacteria. Dis Mark 2015:653537. https://doi.org/10.1155/2015/653537
Tomofuji T, Ekuni D, Irie K et al (2011) Relationships between periodontal inflammation, lipid peroxide and oxidative damage of multiple organs in rats. Biomed Res 32:343–349. https://doi.org/10.2220/biomedres.32.343
Ioannidou E, Shaqman M, Burleson J, Dongari-Bagtzoglou A (2010) Periodontitis case definition affects the association with renal function in kidney transplant recipients. Oral Dis 16:636–642. https://doi.org/10.1111/j.1601-0825.2010.01665.x
Blach A, Franek E, Witula A et al (2009) The influence of chronic periodontitis on serum TNF-α, IL-6 and hs-CRP concentrations, and function of graft and survival of kidney transplant recipients. Clin Transplant 23:213–219. https://doi.org/10.1111/j.1399-0012.2008.00931.x
Franek E, Blach A, Witula A et al (2005) Association between chronic periodontal disease and left ventricular hypertrophy in kidney transplant recipients. Transplant 80:3–5. https://doi.org/10.1097/01.TP.0000158716.12065.24
Zwiech R, Bruzda-Zwiech A (2013) Does oral health contribute to post-transplant complications in kidney allograft recipients? Acta Odontol Scand 71:756–763. https://doi.org/10.3109/00016357.2012.715203
Simmons EM, Langone A, Sezer MT et al (2005) Effect of renal transplantation on biomarkers of inflammation and oxidative stress in end-stage renal disease patients. Transplantation 79:914–919. https://doi.org/10.1097/01.TP.0000157773.96534.29
Aouad LJ, Clayton P, Wyburn KR, Gracey DM, Chadban SJ (2018) Evolution of glycemic control and variability after kidney transplant. Transplant 102:1563–1568. https://doi.org/10.1097/TP.0000000000002155
Jin HY, Lee K, Kim YJ et al (2019) The degree of hyperglycemia excursion in patients of kidney transplantation (KT) or liver transplantation (LT) assessed by continuous glucose monitoring (CGM): Pilot Study. J Diab Res 2019:1757182. https://doi.org/10.1155/2019/1757182
Ruiz S, Zhao H, Chandakkar P et al (2020) Correcting Smad1/5/8, mTOR, and VEGFR2 treats pathology in hereditary hemorrhagic telangiectasia models. J Clin Invest 130:942–957. https://doi.org/10.1172/JCI127425
Albiñana V, Sanz-Rodríguez F, Recio-Poveda L, Bernabéu C, Botella LM (2011) Immunosuppressor FK506 increases endoglin and activin receptor-like kinase 1 expression and modulates transforming growth factor-β1 signaling in endothelial cells. Mol Pharmacol 79:833–843. https://doi.org/10.1124/mol.110.067447
Albiñana V, Cuesta AM, Rojas-P ID, Gallardo-Vara E, Recio-Poveda L, Bernabéu C, Botella LM (2020) Review of pharmacological strategies with repurposed drugs for hereditary hemorrhagic telangiectasia related bleeding. J Clin Med 9:1766. https://doi.org/10.3390/jcm9061766
Ruiz S, Chandakkar P, Zhao H, Papoin J, Chatterjee PK, Christen E, Blanc L, Campagne F, Marambaud P (2017) Tacrolimus rescues the signaling and gene expression signature of endothelial ALK1 loss-of-function and improves HHT vascular pathology. Hum Mol Genet 26:4786–4798. https://doi.org/10.1093/hmg/ddx358
Acknowledgements
The authors thank the hospital staff for their help with data collection.
Funding
This study was supported in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior Brasil (CAPES) [Finance Code 001 and PROCAD grant 88881.357834/2019–01].
Author information
Authors and Affiliations
Contributions
SVG, VPR, DLNS, and ALAP designed the study. SVG and D.L.N.S. contributed to data acquisition. VPR, ALAP, and MAP performed statistical analysis and interpreted the data. VPR, SVG, and MAP drafted the manuscript. All authors revised the manuscript and approved the final version.
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by the Research Ethics Committee of the Federal University of Maranhão (no. 1.572.392, CAAE: 55991616.6.0000.5087).
Informed consent
All participants signed informed consent forms prior to the present study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gomes, S.V., Rodrigues, V., Nunes-dos-Santos, D.L. et al. The relationship between periodontal status and hyperglycemia after kidney transplantation. Clin Oral Invest 26, 397–406 (2022). https://doi.org/10.1007/s00784-021-04011-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-021-04011-6