Abstract
Objective
The aim of this study is to investigate the efficacy of delivering low-level laser therapy (LLLT) in the management of dry socket at University Dental Hospital Sharjah.
Materials and method
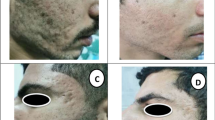
Forty-five patients with dry socket were divided into two treatment groups. Group I dry socket patients (n = 30) received conventional treatment while group II patients (n = 15) were irradiated with LLLT at a setting of 200-mW, 6-J, continuous-wave mode using an R02 tipless handpiece (Fotona Er:YAG, Europe), on the buccal, lingual, and middle surfaces of the socket for 30 s from a delivery distance of 1 cm. Pain score and quantification of granulation tissue in the socket were recorded at 0, 4, and 7 days post-dry socket treatment.
Results
Results showed that the LLLT-irradiated group II sockets showed a much lower VAS pain score of 1–2 as early as day 4, and a richer amount of granulation tissue compared to the conventional treated group I socket. The amount and rate of granulation tissue formation in the dry socket are inversely proportional to the pain score showing significant clinical effectiveness of LLLT on promoting the healing of the dry socket, with improvement in symptoms (P = .001). Conventionally treated dry sockets take at least 7 days to match the effective healing of an LLLT-irradiated dry socket.
Conclusion
LLLT irradiation influences biomodulation of dry socket healing by dampening inflammation, promoting vascularization, stimulating granulation, and controlling pain symptoms.
Clinical relevance
LLLT may be an additional effective tool for managing dry sockets in general dental practice.
Similar content being viewed by others
References
Hamad SA, Naif JS, Abdullah MA (2016) Effect of diode laser on healing of tooth extraction socket: an experimental study in rabbits. J Maxillofac Oral Surg 15:308–314
Eshghpour M, Ahrari F, Najjarkar NT et al (2015) Comparison of the effect of low level laser therapy with alvogyl on the management of alveolar osteitis. Med Oral Patol Oral Cir Bucal 20:e386–e392
Mamoun J (2018) Dry socket etiology, diagnosis, and clinical treatment techniques. J Korean Assoc Oral Maxillofac Surg 44:52–58
Helei VM, Zhero NI, Helei NI et al (2019) Choice of the treatment method of the inflammatory process in the alveolar tooth socket. Wiad Lek 72:1957–1960
Ansari A, Joshi S, Garad A et al (2019) A study to evaluate the efficacy of honey in the management of dry socket. Contemp Clin Dent 10:52
Lone PA, Ahmed SW, Prasad V et al (2018) Role of turmeric in management of alveolar osteitis (dry socket): a randomised clinical study. J Oral Biol Craniofac Res 8:44–47
Çebi AT (2020) Evaluation of the effects of intra-alveolar irrigation with clindamycin, rifampicin and sterile saline in alveolar osteitis treatment. J Stomatol Oral Maxillof Surg S2468-7855(20):30028–30028
Zorina O, Petrukhina N, Boriskina O (2019) Alveolar osteitis treatment using Holisal gel. Stomatologiia 98:58
McCarthy TL, Ji C, Centrella M (2000) Links among growth factors, hormones, and nuclear factors with essential roles in bone formation. Crit Rev Oral Biol Med 11:409–422
Chung H, Dai T, Sharma SK (2012) The nuts and bolts of low-level laser (light) therapy. Ann Biomed Eng 40:516–533
Farivar S, Malekshahabi T, Shiari R (2014) Biological effects of low level laser therapy. J Lasers Med Sci 5:58
Kesler G, Shvero DK, Tov YS, Romanos G (2011) Platelet derived growth factor secretion and bone healing after Er:YAG laser bone irradiation. J Oral Implantol 37:195–204
Ozcelik O, Cenk Haytac M, Kunin A, Seydaoglu G (2008) Improved wound healing by low-level laser irradiation after gingivectomy operations: a controlled clinical pilot study. J Clin Periodontol 35:250–254
Saygun I, Karacay S, Serdar M, Ural AU, Sencimen M, Kurtis B (2008) Effects of laser irradiation on the release of basic fibroblast growth factor (bFGF), insulin like growth factor-1 (IGF-1), and receptor of IGF-1 (IGFBP3) from gingival fibroblasts. Lasers Med Sci 23:211–215
Baird A, Walicke PA (1989) Fibroblast growth factors. Br Med Bull 45:438–452
Calabrese EJ (2016) The emergence of the dose–response concept in biology and medicine. Int J Mol Sci 17:2034
Clokie C, Bentley K, Head T (1991) The effects of the helium-neon laser on postsurgical discomfort: a pilot study. J (Can Dent Assoc) 57:584–586
Nanami T, Shiba H, Ikeuchi S, Nagai T, Asanami S, Shibata T (1993) Clinical applications and basic studies of laser in dentistry and oral surgery. Keio J Med 42:199–201
Lim W, Lee S, Kim I, Chung M, Kim M, Lim H, Park J, Kim O, Choi H (2007) The anti-inflammatory mechanism of 635 nm light-emitting-diode irradiation compared with existing COX inhibitors. Lasers Surg Med 39:614–621
Aimbire F, Albertini R, Pacheco MT et al (2006) Low-level laser therapy induces dose-dependent reduction of TNFα levels in acute inflammation. Photomed Laser Surg 24:33–37
Yıldız ED, Arslan H (2018) Effect of low-level laser therapy on postoperative pain in molars with symptomatic apical periodontitis: a randomized placebo-controlled clinical trial. J Endod 44:610–1615
Parihar AS, Pathak R (2018) Effect of low level laser therapy (LLLT) on post extraction wound healing. J Adv Med Dent Sci Res 6:6–14
Kreisler M, Christoffers AB, Willershausen B, d'Hoedt B (2003) Effect of low-level GaAlAs laser irradiation on the proliferation rate of human periodontal ligament fibroblasts: an in vitro study. J Clin Periodontol 30:353–358
Beckmann KH, Meyer-Hamme G, Schröder S (2014) Low level laser therapy for the treatment of diabetic foot ulcers: a critical survey. Evid Based Complement Alternat Med 30:353–358
Khadra M, Lyngstadaas SP, Haanaes HR et al (2005) Effect of laser therapy on attachment, proliferation and differentiation of human osteoblast-like cells cultured on titanium implant material. Biomaterials 26:3503–3509
Santinoni CD, Oliveira HF, Batista VE et al (2017) Influence of low-level laser therapy on the healing of human bone maxillofacial defects: a systematic review. J Photochem Photobiol B 169:83–89
Kim YD, Kim SS, Hwang DS, Kim SG, Kwon YH, Shin SH, Kim UK, Kim JR, Chung IK (2007) Effect of low-level laser treatment after installation of dental titanium implant-immunohistochemical study of RANKL, RANK, OPG: an experimental study in rats. Lasers Surg Med 39:441–450
Ustaoglu G, Goller Bulut D, Gumus KC (2019) Evaluation of different platelet-rich concentrates effects on early soft tissue healing and socket preservation after tooth extraction. J Stomatol Oral Maxillofac Surg (19):30218–30216
Fortunato L, Bennardo F, Buffone C, Giudice A (2020) Is the application of platelet concentrates effective in the prevention and treatment of medication-related osteonecrosis of the jaw? A systematic review. J Cranio-Maxillofac Surg 48:268–285
Saenko YV, Glushchenko ES, Zolotovskii IO, Sholokhov E, Kurkov A (2016) Mitochondrial dependent oxidative stress in cell culture induced by laser radiation at 1265 nm. Lasers Med Sci 31:405–413
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics
Ethics approval has been obtained from Research Ethics Committee University of Sharjah REC-17-02-14-01-S dated October 24, 2017.
Consent
In this case report, the patient is sufficiently anonymized according to ICMJE guidelines.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kamal, A., Salman, B., AR, N.H. et al. Management of dry socket with low-level laser therapy. Clin Oral Invest 25, 1029–1033 (2021). https://doi.org/10.1007/s00784-020-03393-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-020-03393-3