Abstract
Objective
To examine the association between periodontitis, diabetes, and prediabetes, assessed by fasting plasma glucose (FPG).
Materials and methods
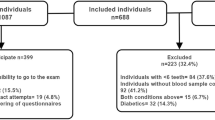
Workers’ Oral Health Study is a cross-sectional survey conducted on a representative sample of the Spanish employed population including 5154 participants (59.5% men, aged 16–65). Examination of periodontal status assessed Community Periodontal Index (CPI) and clinical attachment levels (CAL). Biochemical determinations included fasting plasma glucose (FPG), triglycerides, and total cholesterol. Logistic regression analysis with adjustment for potential confounders was used to evaluate the association between periodontitis and abnormal glucose regulation.
Results
Ninety-five participants (2.2%) of the study population had diabetes, while 373 (8.8%) presented prediabetes. Prediabetes was not associated with CPI or CAL in fully adjusted multivariate logistic regressions models. Diabetes was significantly associated with subjects having a CPI 4 after adjustment for potential confounders (odds ratio OR = 1.9, 95% confidence interval (CI) 1.1–3.1). This association was stronger in subjects < 45 years (OR = 4.0, 95% CI 1.2–12.7).
Conclusion
Periodontitis was associated with diabetes mellitus, but not with prediabetes, in a representative sample of the Spanish employed population. The association was stronger for younger subjects, which emphasizes the need for early detection of diabetes in younger patients affected by periodontitis, particularly because periodontal therapy may help to improve glycemic control.
Clinical relevance
Periodontitis is associated with diabetes mellitus, having at the same time a negative effect on glycemic control. It is important to develop proper early diagnosis strategies for both conditions, particularly in young male adults.

Similar content being viewed by others
References
Nathan DM, Davidson MB, DeFronzo RA, Heine RJ, Henry RR, Pratley R, Zinman B, American Diabetes A (2007) Impaired fasting glucose and impaired glucose tolerance: implications for care. Diabetes Care 30:753–759. https://doi.org/10.2337/dc07-9920
Tabak AG, Herder C, Rathmann W, Brunner EJ, Kivimaki M (2012) Prediabetes: a high-risk state for diabetes development. Lancet 379:2279–2290. https://doi.org/10.1016/S0140-6736(12)60283-9
Danaei G, Finucane MM, Lu Y, Singh GM, Cowan MJ, Paciorek CJ, Lin JK, Farzadfar F, Khang YH, Stevens GA, Rao M, Ali MK, Riley LM, Robinson CA, Ezzati M, Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating G (2011) National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2.7 million participants. Lancet 378:31–40. https://doi.org/10.1016/S0140-6736(11)60679-X
Federation ID (2017) IDF diabetes atlas. Brussels, Belgium
Soriguer F, Goday A, Bosch-Comas A, Bordiu E, Calle-Pascual A, Carmena R, Casamitjana R, Castano L, Castell C, Catala M, Delgado E, Franch J, Gaztambide S, Girbes J, Gomis R, Gutierrez G, Lopez-Alba A, Martinez-Larrad MT, Menendez E, Mora-Peces I, Ortega E, Pascual-Manich G, Rojo-Martinez G, Serrano-Rios M, Valdes S, Vazquez JA, Vendrell J (2012) Prevalence of diabetes mellitus and impaired glucose regulation in Spain: the Di@bet.es study. Diabetologia 55:88–93. https://doi.org/10.1007/s00125-011-2336-9
Fonseca VA (2009) Defining and characterizing the progression of type 2 diabetes. Diabetes Care 32(Suppl 2):S151–S156. https://doi.org/10.2337/dc09-S301
Shaye K, Amir T, Shlomo S, Yechezkel S (2012) Fasting glucose levels within the high normal range predict cardiovascular outcome. Am Heart J 164:111–116. https://doi.org/10.1016/j.ahj.2012.03.023
Eke PI, Dye BA, Wei L, Slade GD, Thornton-Evans GO, Borgnakke WS, Taylor GW, Page RC, Beck JD, Genco RJ (2015) Update on prevalence of periodontitis in adults in the United States: NHANES 2009 to 2012. J Periodontol 86:611–622. https://doi.org/10.1902/jop.2015.140520
Konig J, Holtfreter B, Kocher T (2010) Periodontal health in Europe: future trends based on treatment needs and the provision of periodontal services--position paper 1. Eur J Dent Educ 14(Suppl 1):4–24. https://doi.org/10.1111/j.1600-0579.2010.00620.x
Schutzhold S, Kocher T, Biffar R, Hoffmann T, Schmidt CO, Micheelis W, Jordan R, Holtfreter B (2015) Changes in prevalence of periodontitis in two German population-based studies. J Clin Periodontol 42:121–130. https://doi.org/10.1111/jcpe.12352
Carasol M, Llodra JC, Fernandez-Meseguer A, Bravo M, Garcia-Margallo MT, Calvo-Bonacho E, Sanz M, Herrera D (2016) Periodontal conditions among employed adults in Spain. J Clin Periodontol 43:548–556. https://doi.org/10.1111/jcpe.12558
Tonetti MS, Jepsen S, Jin L, Otomo-Corgel J (2017) Impact of the global burden of periodontal diseases on health, nutrition and wellbeing of mankind: a call for global action. J Clin Periodontol 44:456–462. https://doi.org/10.1111/jcpe.12732
Montero J, Yarte JM, Bravo M, Lopez-Valverde A (2011) Oral health-related quality of life of a consecutive sample of Spanish dental patients. Med Oral Patol Oral Cir Bucal 16:e810–e815
Borgnakke WS, Ylostalo PV, Taylor GW, Genco RJ (2013) Effect of periodontal disease on diabetes: systematic review of epidemiologic observational evidence. J Clin Periodontol 40(Suppl 14):S135–S152. https://doi.org/10.1111/jcpe.12080
Chapple IL, Genco R (2013) Diabetes and periodontal diseases: consensus report of the Joint EFP/AAP Workshop on Periodontitis and Systemic Diseases. J Clin Periodontol 40(Suppl 14):S106–S112. https://doi.org/10.1111/jcpe.12077
Graziani F, Gennai S, Solini A, Petrini M (2018) A systematic review and meta-analysis of epidemiologic observational evidence on the effect of periodontitis on diabetes an update of the EFP-AAP review. J Clin Periodontol 45:167–187. https://doi.org/10.1111/jcpe.12837
Polak D, Shapira L (2018) An update on the evidence for pathogenic mechanisms that may link periodontitis and diabetes. J Clin Periodontol 45:150–166. https://doi.org/10.1111/jcpe.12803
Demmer RT, Desvarieux M, Holtfreter B, Jacobs DR Jr, Wallaschofski H, Nauck M, Volzke H, Kocher T (2010) Periodontal status and A1C change: longitudinal results from the study of health in Pomerania (SHIP). Diabetes Care 33:1037–1043. https://doi.org/10.2337/dc09-1778
Saito T, Shimazaki Y, Kiyohara Y, Kato I, Kubo M, Iida M, Koga T (2004) The severity of periodontal disease is associated with the development of glucose intolerance in non-diabetics: the Hisayama study. J Dent Res 83:485–490
Choi YH, McKeown RE, Mayer-Davis EJ, Liese AD, Song KB, Merchant AT (2011) Association between periodontitis and impaired fasting glucose and diabetes. Diabetes Care 34:381–386. https://doi.org/10.2337/dc10-1354
Lalla E, Cheng B, Kunzel C, Burkett S, Ferraro A, Lamster IB (2015) Six-month outcomes in dental patients identified with hyperglycaemia: a randomized clinical trial. J Clin Periodontol 42:228–235. https://doi.org/10.1111/jcpe.12358
Hong JW, Noh JH, Kim DJ (2016) The prevalence and associated factors of periodontitis according to fasting plasma glucose in the Korean adults: the 2012-2013 Korea National Health and Nutrition Examination Survey. Medicine (Baltimore) 95:e3226. https://doi.org/10.1097/MD.0000000000003226
Noack B, Jachmann I, Roscher S, Sieber L, Kopprasch S, Luck C, Hanefeld M, Hoffmann T (2000) Metabolic diseases and their possible link to risk indicators of periodontitis. J Periodontol 71:898–903. https://doi.org/10.1902/jop.2000.71.6.898
Arora N, Papapanou PN, Rosenbaum M, Jacobs DR Jr, Desvarieux M, Demmer RT (2014) Periodontal infection, impaired fasting glucose and impaired glucose tolerance: results from the Continuous National Health and Nutrition Examination Survey 2009-2010. J Clin Periodontol 41:643–652. https://doi.org/10.1111/jcpe.12258
Kowall B, Holtfreter B, Volzke H, Schipf S, Mundt T, Rathmann W, Kocher T (2015) Pre-diabetes and well-controlled diabetes are not associated with periodontal disease: the SHIP Trend Study. J Clin Periodontol 42:422–430. https://doi.org/10.1111/jcpe.12391
Eke PI, Wei L, Thornton-Evans GO, Borrell LN, Borgnakke WS, Dye B, Genco RJ (2016) Risk indicators for periodontitis in US adults: NHANES 2009 to 2012. J Periodontol 87:1174–1185. https://doi.org/10.1902/jop.2016.160013
WHO (1997) Oral health surveys: basic methods. World Health Organization, Geneva
Sanchez-Chaparro MA, Roman-Garcia J, Calvo-Bonacho E, Gomez-Larios T, Fernandez-Meseguer A, Sainz-Gutierrez JC, Cabrera-Sierra M, Garcia-Garcia A, Rueda-Vicente J, Galvez-Moraleda A, Gonzalez-Quintela A (2006) Prevalence of cardiovascular risk factors in the Spanish working population. Rev Esp Cardiol 59:421–430
Sanchez-Chaparro MA, Calvo-Bonacho E, Gonzalez-Quintela A, Fernandez-Labandera C, Cabrera M, Sainz JC, Fernandez-Meseguer A, Banegas JR, Ruilope LM, Valdivielso P, Roman-Garcia J, Ibermutuamur Cardiovascular Risk Assessment Study G (2008) Occupation-related differences in the prevalence of metabolic syndrome. Diabetes Care 31:1884–1885. https://doi.org/10.2337/dc08-0431
Valdivielso P, Sanchez-Chaparro MA, Calvo-Bonacho E, Cabrera-Sierra M, Sainz-Gutierrez JC, Fernandez-Labandera C, Fernandez-Meseguer A, Quevedo-Aguado L, Moraga MR, Galvez-Moraleda A, Gonzalez-Quintela A, Roman-Garcia J, group Is (2009) Association of moderate and severe hypertriglyceridemia with obesity, diabetes mellitus and vascular disease in the Spanish working population: results of the ICARIA study. Atherosclerosis 207:573–578. https://doi.org/10.1016/j.atherosclerosis.2009.05.024
Sanchez-Chaparro MA, Calvo Bonacho E, Gonzalez Quintela A, Cabrera M, Sainz JC, Fernandez-Labander C, Quevedo-Aguado L, Gelpi JA, Fernandez Meseguer A, Brotons C, de Teresa E, Gonzalez Santos P, Roman Garcia J, Icaria Study Group (2011) High cardiovascular risk in Spanish workers. Nutr Metab Cardiovasc Dis 21:231–236. https://doi.org/10.1016/j.numecd.2009.10.001
Estadística INd (2008) Encuesta de Población Activa 2° Trimestre (EPA 2008TII). Book title., Available at: http://www.ine.es/daco/daco42/daco4211/epa0208.pdf [Accessed 15 March 2015]
WHO (2000) Global strategy for the prevention and control of noncommunicable diseases. World Health Organization (WHO), Geneva
Sacks DB, Arnold M, Bakris GL, Bruns DE, Horvath AR, Kirkman MS, Lernmark A, Metzger BE, Nathan DM (2011) Guidelines and recommendations for laboratory analysis in the diagnosis and management of diabetes mellitus. Clin Chem 57:e1–e47. https://doi.org/10.1373/clinchem.2010.161596
Friedewald WT, Levy RI, Fredrickson DS (1972) Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 18:499–502
American Diabetes A (2014) Diagnosis and classification of diabetes mellitus. Diabetes Care 37(Suppl 1):S81–S90. https://doi.org/10.2337/dc14-S081
Tonetti MS, Claffey N, European Workshop in Periodontology group C (2005) Advances in the progression of periodontitis and proposal of definitions of a periodontitis case and disease progression for use in risk factor research. Group C consensus report of the 5th European Workshop in Periodontology. J Clin Periodontol 32:210–213. https://doi.org/10.1111/j.1600-051X.2005.00822.x
Eke PI, Dye BA, Wei L, Thornton-Evans GO, Genco RJ (2012) Prevalence of periodontitis in adults in the United States: 2009 and 2010. J Dent Res 91:914–920. https://doi.org/10.1177/0022034512457373
Kocher T, Holtfreter B, Petersmann A, Eickholz P, Hoffmann T, Kaner D, Kim TS, Meyle J, Schlagenhauf U, Doering S, Gravemeier M, Prior K, Rathmann W, Harks I, Ehmke B, Koch R (2018) Effect of periodontal treatment on HbA1c among patients with prediabetes. J Dent Res 22034518804185:171–179. https://doi.org/10.1177/0022034518804185
Javed F, Ahmed HB, Mehmood A, Bain C, Romanos GE (2014) Effect of nonsurgical periodontal therapy (with or without oral doxycycline delivery) on glycemic status and clinical periodontal parameters in patients with prediabetes: a short-term longitudinal randomized case-control study. Clin Oral Investig 18:1963–1968. https://doi.org/10.1007/s00784-014-1185-6
Alshehri FA, Javed F (2015) Impact of scaling and root planing on clinical periodontal status and glycemic levels in prediabetic patients. Interv Med Appl Sci 7:17–21. https://doi.org/10.1556/IMAS.6.2014.004
Nelson RG, Shlossman M, Budding LM, Pettitt DJ, Saad MF, Genco RJ, Knowler WC (1990) Periodontal disease and NIDDM in Pima Indians. Diabetes Care 13:836–840
Emrich LJ, Shlossman M, Genco RJ (1991) Periodontal disease in non-insulin-dependent diabetes mellitus. J Periodontol 62:123–131
Demmer RT, Squillaro A, Papapanou PN, Rosenbaum M, Friedewald WT, Jacobs DR Jr, Desvarieux M (2012) Periodontal infection, systemic inflammation, and insulin resistance: results from the continuous National Health and Nutrition Examination Survey (NHANES) 1999-2004. Diabetes Care 35:2235–2242. https://doi.org/10.2337/dc12-0072
Nesse W, Abbas F, van der Ploeg I, Spijkervet FK, Dijkstra PU, Vissink A (2008) Periodontal inflamed surface area: quantifying inflammatory burden. J Clin Periodontol 35:668–673. https://doi.org/10.1111/j.1600-051X.2008.01249.x
Kebschull M, Demmer RT, Grun B, Guarnieri P, Pavlidis P, Papapanou PN (2014) Gingival tissue transcriptomes identify distinct periodontitis phenotypes. J Dent Res 93:459–468. https://doi.org/10.1177/0022034514527288
Kingman A, Albandar JM (2002) Methodological aspects of epidemiological studies of periodontal diseases. Periodontol 29:11–30
Sanz M, Ceriello A, Buysschaert M, Chapple I, Demmer RT, Graziani F, Herrera D, Jepsen S, Lione L, Madianos P, Mathur M, Montanya E, Shapira L, Tonetti M, Vegh D (2018) Scientific evidence on the links between periodontal diseases and diabetes: consensus report and guidelines of the joint workshop on periodontal diseases and diabetes by the international Diabetes Federation and the European Federation of Periodontology. J Clin Periodontol 45:138–149. https://doi.org/10.1111/jcpe.12808
Funding
This study was supported by Cualtis, previously named Sociedad de Prevención de Ibermutuamur, a company that focuses specifically on preventing diseases and accidents, by monitoring and promoting workers’ health. The authors were fully independent in preparing the protocol, conducting the research, interpreting the results and preparing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Montero, E., Carasol, M., Fernández-Meseguer, A. et al. Prediabetes and diabetes prevalence in the Workers’ Oral Health Study. Clin Oral Invest 23, 4233–4241 (2019). https://doi.org/10.1007/s00784-019-02875-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-019-02875-3