Abstract
Objectives
To estimate the prevalence of prediabetes in individuals with moderate or severe periodontitis and to verify the association between periodontitis and glycated hemoglobin levels.
Material and methods
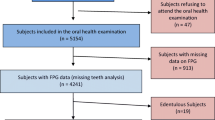
A cross-sectional study was conducted including individuals age 18–93 years from a representative sample residing in rural Southern Brazil. Data collection included full mouth periodontal clinical examinations, laboratory screens, and structured questionnaires. Glycemic levels were based on glycated hemoglobin. Periodontitis case definition was based on criteria established by the Centers for Disease Control and Prevention and the American Academy of Periodontology. A logistic regression model adjusted for body mass index was used to estimate odds ratios (OR) and 95% confidence intervals (CI). The association between periodontal parameters and changes in glycated hemoglobin levels was evaluated using linear regression models.
Results
A higher prevalence of prediabetes was observed among individuals with moderate (39.6%) and severe periodontitis (49.7%) than in individuals with mild (23.8%) or no periodontitis (27.8%). Adjusting for body mass index, individuals with severe periodontitis exhibited a 2.5 greater chance of being prediabetic (OR=2.5; 95% CI: 1.3–4.9) that was significantly associated with an increase of 0.10% in HbA1c.
Conclusion
Severe periodontitis was associated with elevated blood glucose levels. Individuals with this condition having a higher percentage HbA1c are more likely to be prediabetic.
Clinical relevance
This study highlights the importance of the clinicians’ awareness of the association between severe periodontitis and prediabetes allowing its early detection in the dental office.

Similar content being viewed by others
References
International Diabetes Federation (2019) Diabetes Atlas Ninth edition. Brussels, Belgium: International Diabetes Federation
Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, Colagiuri S, Guariguata L, Motala AA, Ogurtsova K, Shaw JE, Bright D, Williams R, IDF Diabetes Atlas Committee (2019) Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas , 9 th edition. Diabetes Res Clin Pract 157:107843. https://doi.org/10.1016/j.diabres.2019.107843
American Diabetes Association (2020) 2 Classification and diagnosis of diabetes: standards of Medical Care in Diabetes-2020. Diabetes Care 43(Suppl. 1):S14–S31. https://doi.org/10.2337/dc20-S002
Mataftsi M, Koukos G, Sakellari D (2019) Prevalence of undiagnosed diabetes and pre-diabetes in chronic periodontitis patients assessed by an HbA1c chairside screening protocol. Clin Oral Investig 23(12):4365–4370. https://doi.org/10.1007/s00784-019-02888-y
Huang Y, Cai X, Mai W, Li M, Hu Y (2016) Association between prediabetes and risk of cardiovascular disease and all cause mortality: systematic review and meta-analysis. BMJ 23(355):i5953. https://doi.org/10.1136/bmj.i5953
American Medical Association Centers for Disease Control and Prevention (2015) Preventing type 2 diabetes. Atlanta: Centers for Disease Control and Prevention
Chapple ILC, Genco R (2013) Diabetes and periodontal diseases: consensus report of the Joint EFP/AAP Workshop on Periodontitis and Systemic Diseases. J Periodontol 84(4 Suppl):S106–S112. https://doi.org/10.1902/jop.2013.1340011
Papapanou PN, Sanz M, Buduneli N, Dietrich T, Feres M, Fine DH, Flemmig TF, Garcia R, Giannobile WV, Graziani F, Greenwell H, Herrera D, Kao RT, Kebschull M, Kinane DF, Kirkwood KL, Kocher T, Kornman KS, Kumar PS, Loos BG, Machtei E, Meng H, Mombelli A, Needleman I, Offenbacher S, Seymour GJ, Teles R, Tonetti MS (2018) Periodontitis: consensus report of workgroup 2 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Clin Periodontol 45:162–170. https://doi.org/10.1111/jcpe.12946
Eke PI, Wei L, Borgnakke WS, Thornton-Evans G, Zhang X, Lu H, McGuire LC, Genco RJ (2016) Periodontitis prevalence in adults ≥ 65 years of age, in the USA. Periodontol 2000(72):76–95. https://doi.org/10.1111/prd.12145
Petersen PE, Ogawa H (2012) The global burden of periodontal disease: Towards integration with chronic disease prevention and control. Periodontol 60(1):15–39. https://doi.org/10.1111/j.1600-0757.2011.00425.x
Bernabe E, Marcenes W, Hernandez CR et al (2020) Global, regional, and national levels and trends in burden of oral conditions from 1990 to 2017: a systematic analysis for the Global Burden of Disease 2017 Study. J Dent Res 99(4):362–373. https://doi.org/10.1177/0022034520908533
Polak D, Shapira L (2018) An update on the evidence for pathogenic mechanisms that may link periodontitis and diabetes. J Clin Periodontol 45(2):150–166. https://doi.org/10.1111/jcpe.12803
Grossi SG, Zambón JJ, Ho AW et al (1994) Assessment of risk for periodontal disease. I Risk indicators for attachment loss J Periodontol 65(3):260–267. https://doi.org/10.1902/jop.1994.65.3.260
Borgnakke WS, Ylöstalo PV, Taylor GW et al (2013) Effect of periodontal disease on diabetes: systematic review of epidemiologic observational evidence. J Periodontol 84(4 Suppl):S135–S152. https://doi.org/10.1902/jop.2013.1340013
Taylor GW, Burt B, Becker MP et al (1996) Severe periodontitis and risk for poor glycemic control in patients with non-insulin-dependent diabetes mellitus. J Periodontol 67(10 Suppl):1085–1093. https://doi.org/10.1902/jop.1996.67.10s.1085
Lalla E, Papapanou PN (2011) Diabetes mellitus and periodontitis: a tale of two common interrelated diseases. Nat Rev Endocrinol 7(12):738–748. https://doi.org/10.1038/nrendo.2011.106
Holm N-CR, Belstrøm D, Østergaard JA, Schou S, Holmstrup P, Grauballe MB (2016) Identification of individuals with undiagnosed diabetes and pre-diabetes in a Danish cohort attending dental treatment. J Periodontol 87(4):395–402. https://doi.org/10.1902/jop.2016.150266
Preshaw PM, Alba AL, Herrera D, Jepsen S, Konstantinidis A, Makrilakis K, Taylor R (2012) Periodontitis and diabetes: a two-way relationship. Diabetologia 55(1):21–31. https://doi.org/10.1007/s00125-011-2342-y
Taylor JJ, Preshaw PM, Lalla E (2013) A review of the evidence for pathogenic mechanisms that may link periodontitis and diabetes. J Periodontol 84(4 Suppl):S113–S134. https://doi.org/10.1902/jop.2013.134005
Taylor GW, Borgnakke WS (2008) Periodontal disease: associations with diabetes,glycemic control and complications. Oral Dis 14(3):191–203. https://doi.org/10.1111/j.1601-0825.2008.01442.x
Albert DA, Ward A, Allweiss P, Graves DT, Knowler WC, Kunzel C, Leibel RL, Novak KF, Oates TW, Papapanou PN, Schmidt AM, Taylor GW, Lamster IB, Lalla E (2012) Diabetes and oral disease: implications for health professionals. Ann N Y Acad Sci 1255:1–15. https://doi.org/10.1111/j.1749-6632.2011.06460.x
Lalla E, Kunzel C, Burkett S, Cheng B, Lamster IB (2011) Identification of unrecognized diabetes and pre-diabetes in a dental setting. J Dent Res 90(7):855–860. https://doi.org/10.1177/0022034511407069
Ferreira TGM, Rocha JM, de David SC et al (2019) Sampling strategy of an epidemiological survey using a satellite image program. Rev Saúde Pública 53:47. https://doi.org/10.11606/s1518-8787.2019053000834
Ainamo J, Bay I (1975) Problems and proposals for recording gingivitis and plaque. Int Dent J 25(4):229–235
World Health Organization (2010) WHO guidelines on drawing blood: best practices in phlebotomy. Geneva: World Health Organization 2010:1–105
Instituto Brasileiro de Geografia e Estatística (2013) Manual de antropometria. Pesquisa Nacional de Saúde [accessed 20 Set]. Rio de Janeiro: IBGE Available at: http://www.pns.icict.fiocruz.br/arquivos/Novos/Manual%20de%20Antropometria%20PDF.pdf.Portuguese
Centers for Disease Control and Prevention (2007) National Health and Nutrition Examinatory Survey (NHANES): Anthropometry Procedures Manual [accessed 20 Set]. Atlanta: CDC Available at: https://www.cdc.gov/nchs/data/nhanes/nhanes_07_08/manual_an.pdf
Eke PI, Page RC, Wei L, Thornton-Evans G, Genco RJ (2012) Update of the case definitions for population-based surveillance of periodontitis. J Periodontol 83(12):1449–1454. https://doi.org/10.1902/jop.2012.110664
Holtfreter B, Albandar JM, Dietrich T, Dye BA, Eaton KA, Eke PI, Papapanou PN, Kocher T, Joint EU/USA Periodontal Epidemiology Working Group (2015) Standards for reporting chronic periodontitis prevalence and severity in epidemiologic studies: proposed standards from the Joint EU/USA Periodontal Epidemiology Working Group. J Clin Periodontol 42(5):407–412. https://doi.org/10.1111/jcpe.12392
Tonetti MS, Greenwell H, Kornman KS (2018) Staging and grading of periodontitis: Framework and proposal of a new classification and case definition. J Clin Periodontol 45:149–161. https://doi.org/10.1111/jcpe.12945
Taboza ZA, Costa KL, Silveira VR, Furlaneto FA, Montenegro Jr R, Russell S, Dasanayake A, Rego RO (2018) Periodontitis, edentulism and glycemic control in patients with type 2 diabetes: a cross-sectional study. BMJ Open Diabetes Res Care 6(1):e000453. https://doi.org/10.1136/bmjdrc-2017-000453
Costa KL, Taboza ZA, Angelino GB, Silveira VR, Montenegro R Jr, Haas AN, Rego RO (2016) The influence of periodontal disease on changes of glycated hemoglobin levels in type 2 diabetics: a retrospective cohort study. J Periodontol 88(1):1–13. https://doi.org/10.1902/jop.2016.160140
Silbernagel G, Grammer TB, Winkelmann BR, Boehm BO, Marz W (2011) Glycated hemoglobin predicts all-cause, cardiovascular, and cancer mortality in people without a history of diabetes undergoing coronary angiography. Diabetes Care 34(6):1355–1361. https://doi.org/10.2337/dc10-2010
Simpson TC, Weldon JC, Worthington HV et al (2015) Treatment of periodontal disease for glycaemic control in people with diabetes mellitus. Cochrane Database Syst Rev 6(11):CD004714. https://doi.org/10.1002/14651858
Khaw KT, Wareham N, Luben R, Bingham S, Oakes S, Welch A, Day N (2001) Glycated haemoglobin, diabetes, and mortality in men in Norfolk cohort of European prospective investigation of cancer and nutrition (EPIC-Norfolk). BMJ 322(7277):15–18. https://doi.org/10.1136/bmj.322.7277.15
Estrich CG, Araujo MWB, Lipman RD (2019) Prediabetes and diabetes screening in dental care settings: NHANES 2013 to 2016. JDR Clin Trans Res 4(1):76–85. https://doi.org/10.1177/2380084418798818
Centers for Disease Control and Prevention (2020) National Diabetes Statistics Report, 2020. Atlanta, GA: Centers for Disease Control and Prevention U.S. Dept of Health and Human Services
Sanz M, Ceriello A, Buysschaert M, Chapple I, Demmer RT, Graziani F, Herrera D, Jepsen S, Lione L, Madianos P, Mathur M, Montanya E, Shapira L, Tonetti M, Vegh D (2018) Scientific evidence on the links between periodontal diseases and diabetes: consensus report and guidelines of the joint workshop on periodontal diseases and diabetes by the International Diabetes Federation and the European Federation of Periodontology. J Clin Periodontol 45(2):138–149. https://doi.org/10.1111/jcpe.12808
Acknowledgements
The authors are grateful to Alessandra Pascotini Grellmann, Maísa Casarin, Silvia Cardoso de David, and Ticiane de Góes Mário Ferreira for their contributions with data collection, and Sérgio Dantas and the staff of the Rosário do Sul City Hall for collaboration with this study. Our special thanks to Dr. Ulf Wikesjö for reviewing this manuscript.
Funding
This study was funded by Rosário do Sul City Hall and, in part, by the Brazilian fostering agency Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES [Coordination for the Advancement of Higher Education Personnel] – Finance code 001).
Author information
Authors and Affiliations
Contributions
Rodrigo da Cunha Rossignollo Tavares—statistical analysis, writing and review of manuscript
Gabriela Barbieri Ortigara—writing and review of manuscript
Karen Finger Tatsch—writing and review of manuscript
Ciandra Miraglia Ferreira—writing and review of manuscript
Jociana Boligon—data collect, writing and review of manuscript
Carlos Heitor Cunha Moreira—study design, coordination, data analysis and in drafting and review this manuscript.
Corresponding author
Ethics declarations
Ethical approval
This study received approval from the Human Research Ethics Committee of the Federal University of Santa Maria (certificate number: 37862414.5.0000.5346) and was performed in accordance with Declaration of Helsinki (1964, revised in 1975, 1983, 1989, 1996, and 2000).
Consent to participate
All individuals who agreed to participate signed a written informed-consent-form.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tavares, R.d.R., Ortigara, G.B., Tatsch, K.F. et al. Association between periodontitis and glycated hemoglobin levels in individuals living in rural Southern Brazil. Clin Oral Invest 25, 6901–6907 (2021). https://doi.org/10.1007/s00784-021-03980-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-021-03980-y