Abstract
Introduction
Lactoferrin has recently been reported for its potent bone growth effects. However, the effects of lactoferrin on the healing process of fragility fracture have not yet been studied, so the purpose of this study is to investigate whether oral administration of lactoferrin can promote the fracture healing in an OVX animal model.
Materials and methods
Three months after bilateral ovariectomy, all rats underwent unilateral tibial osteotomy and were then randomly divided into control group and bovine lactoferrin (bLF) group. At 4 and 8 weeks post-fracture, animals were sacrificed, and the fractured tibiae and serum samples were collected for evaluation.
Results
Our results showed that bLF treatment not only accelerated the bone growth at an early stage of OPF healing but also shortened the remolding process of OPF healing. When compared to control group, bLF treatment induced a significant rise in callus BMD (by 35.0% at 4 weeks and by 39.7% at 8 weeks; both p < 0.05) consistent with enhanced biomechanical strength of the callus, with ultimate force increased by 3.39-fold at 4 weeks (p < 0.05) and 1.95-fold at 8 weeks (p < 0.05). Besides, bLF administration resulted in a substantial increase in serum levels of BALP and a significant decrease in serum levels of TRAP 5b and TNF-α. Moreover, both the RANKL/OPG mRNA ratio and the expression of TNF-α in the callus of bLF-treated group were markedly lower than those in the control group.
Conclusions
At a dose of 85mg/kg/day orally administrated bLF potently promoted the bone healing following tibial fracture in OVX rats.






Similar content being viewed by others
References
NIH Consensus Development Panel on Osteoporosis Prevention Diagnosis and Therapy (2001) Osteoporosis prevention, diagnosis, and therapy. JAMA 285:785–795
Lane NE (2006) Epidemiology, etiology, and diagnosis of osteoporosis. Am J Obstet Gynecol 194:S3–11
Meyer RA, Tsahakis PJ, Martin DF, Banks DM, Harrow ME, Kiebzak GM (2001) Age and ovariectomy impair both the normalization of mechanical properties and the accretion of mineral by the fracture callus in rats. J Orthop Res 19:428–435
Wang JW, Li W, Xu SW, Yang DS, Wang Y, Lin M, Zhao GF (2005) Osteoporosis influences the middle and late periods of fracture healing in a rat osteoporotic model. Chin J Traumatol 8:111–116
Rossini M, Lello S, Sblendorio I, Viapiana O, Fracassi E, Adami S, Gatti D (2013) Profile of bazedoxifene/conjugated estrogens for the treatment of estrogen deficiency symptoms and osteoporosis in women at risk of fracture. Drug Des Dev Ther 7:601–610
Ravn P (2002) Bisphosphonates for prevention of postmenopausal osteoporosis. Dan Med Bull 49:1–18
Binkley N, Bone H, Gilligan JP, Krause DS (2014) Efficacy and safety of oral recombinant calcitonin tablets in postmenopausal women with low bone mass and increased fracture risk: a randomized, placebo-controlled trial. Osteoporos Int 25:2649–2656
Henriksen K, Andersen JR, Riis BJ, Mehta N, Tavakkol R, Alexandersen P, Byrjalsen I, Valter I, Nedergaard BS, Teglbjaerg CS, Stern W (2013) Evaluation of the efficacy, safety and pharmacokinetic profile of oral recombinant human parathyroid hormone [rhPTH(1–31)NH(2)] in postmenopausal women with osteoporosis. Bone 53:160–166
Avenell A, Mak JC, O'Connell D (2014) Vitamin D and vitamin D analogues for preventing fractures in post-menopausal women and older men. Cochrane Database Syst Rev 4:CD000227
Saito M, Shiraishi A, Ito M, Sakai S, Hayakawa N, Mihara M, Marumo K (2010) Comparison of effects of alfacalcidol and alendronate on mechanical properties and bone collagen cross-links of callus in the fracture repair rat model. Bone 46:1170–1179
Fu LJ, Tang TT, Hao YQ, Dai KR (2013) Long-term effects of alendronate on fracture healing and bone remodeling of femoral shaft in ovariectomized rats. Acta Pharmacol Sin 34:387–392
Girotra M, Rubin MR, Bilezikian JP (2006) The use of parathyroid hormone in the treatment of osteoporosis. Rev Endocr Metab Disord 7:113–121
Lorget F, Clough J, Oliveira M, Daury MC, Sabokbar A, Offord E (2002) Lactoferrin reduces in vitro osteoclast differentiation and resorbing activity. Biochem Biophys Res Commun 296:261–266
Cornish J, Naot D (2010) Lactoferrin as an effector molecule in the skeleton. Biometals 23:425–430
Cornish J, Callon KE, Naot D, Palmano KP, Banovic T, Bava U, Watson M, Lin JM, Tong PC, Chen Q, Chan VA (2004) Lactoferrin is a potent regulator of bone cell activity and increases bone formation in vivo. Endocrinology 145:4366–4374
Hou JM, Xue Y, Lin QM (2012) Bovine lactoferrin improves bone mass and microstructure in ovariectomized rats via OPG/RANKL/RANK pathway. Acta Pharmacol Sin 33:1277–1284
Blais A, Malet A, Mikogami T, Martin-Rouas C, Tome D (2009) Oral bovine lactoferrin improves bone status of ovariectomized mice. Am J Physiol Endocrinol Metab 296:E1281–1288
Li YF, Luo E, Feng G, Zhu SS, Li JH, Hu J (2010) Systemic treatment with strontium ranelate promotes tibial fracture healing in ovariectomized rats. Osteoporos Int 21:1889–1897
Guo HY, Jiang L, Ibrahim SA, Zhang L, Zhang H, Zhang M, Ren FZ (2009) Orally administered lactoferrin preserves bone mass and microarchitecture in ovariectomized rats. J Nutr 139:958–964
Schmidmaier G, Wildemann B, Bail H, Lucke M, Fuchs T, Stemberger A, Flyvbjerg A, Haas NP, Raschke M (2001) Local application of growth factors (insulin-like growth factor-1 and transforming growth factor-beta1) from a biodegradable poly(d, l-lactide) coating of osteosynthetic implants accelerates fracture healing in rats. Bone 28:341–350
Boyd SK, Davison P, Muller R, Gasser JA (2006) Monitoring individual morphological changes over time in ovariectomized rats by in vivo micro-computed tomography. Bone 39:854–862
Indrekvam K, Gjerdet NR, Engesaeter LB, Langeland N (1991) Effects of intramedullary reaming and nailing of rat femur. A mechanical and chemical study. Acta Orthop Scand 62:582–586
Namkung-Matthai H, Appleyard R, Jansen J, Hao Lin J, Maastricht S, Swain M, Mason RS, Murrell GA, Diwan AD, Diamond T (2001) Osteoporosis influences the early period of fracture healing in a rat osteoporotic model. Bone 28:80–86
Giannoudis P, Tzioupis C, Almalki T, Buckley R (2007) Fracture healing in osteoporotic fractures: is it really different? A basic science perspective. Injury 38:S90–99
Naot D, Chhana A, Matthews BG, Callon KE, Tong PC, Lin JM, Costa JL, Watson M, Grey AB, Cornish J (2011) Molecular mechanisms involved in the mitogenic effect of lactoferrin in osteoblasts. Bone 49:217–224
Inubushi T, Kawazoe A, Miyauchi M, Kudo Y, Ao M, Ishikado A, Makino T, Takata T (2012) Molecular mechanisms of the inhibitory effects of bovine lactoferrin on lipopolysaccharide-mediated osteoclastogenesis. J Biol Chem 287:23527–23536
McCann RM, Colleary G, Geddis C, Clarke SA, Jordan GR, Dickson GR, Marsh D (2008) Effect of osteoporosis on bone mineral density and fracture repair in a rat femoral fracture model. J Orthop Res 26:384–393
Pang J, Ye M, Gu X, Cao Y, Zheng Y, Guo H, Zhao Y, Zhan H, Shi Y (2015) Ovariectomy-induced osteopenia influences the middle and late periods of bone healing in a mouse femoral osteotomy model. Rejuvenation res 18:356–365
Breuil V, Cosman F, Stein L, Horbert W, Nieves J, Shen V, Lindsay R, Dempster DW (1998) Human osteoclast formation and activity in vitro: effects of alendronate. J Bone Miner Res 13:1721–1729
Kwak HB, Kim JY, Kim KJ, Choi MK, Kim JJ, Kim KM, Shin YI, Lee MS, Kim HS, Kim JW, Chun CH (2009) Risedronate directly inhibits osteoclast differentiation and inflammatory bone loss. Biol Pharm Bull 32:1193–1198
Zhao R (2012) Immune regulation of osteoclast function in postmenopausal osteoporosis: a critical interdisciplinary perspective. Int J Med Sci 9:825–832
Pacifici R (2008) Estrogen deficiency, T cells and bone loss. Cell Immunol 252:68–80
Malet A, Bournaud E, Lan A, Mikogami T, Tome D, Blais A (2011) Bovine lactoferrin improves bone status of ovariectomized mice via immune function modulation. Bone 48:1028–1035
Acknowledgements
This study was supported by grants from The National Natural Science Foundation of China (No. 81600832), Chongqing Research Program of Basic Research and Frontier Technology (cstc2019jcyj-msxmX0455), Project Supported by Scientific and Technological Research Program of Chongqing Municipal Education Commission (No. KJQN201900406, KJQN201902804), Project Supported by Program for Innovation Team Building at Institutions of Higher Education in Chongqing in 2016 (No. CXTDG201602006) and Project Supported by Chongqing Municipal Key Laboratory of Oral Biomedical Engineering of Higher Education.
Author information
Authors and Affiliations
Contributions
WL contributed to conception, design, data acquisition, analysis, and interpretation, drafted the manuscript; JH contributed to data acquisition, analysis, and interpretation, drafted and critically revised the manuscript; PJ and SZ contributed to conception and design, and critically revised the manuscript; YZ contributed to conception, design, data acquisition, analysis, and interpretation, drafted and critically revised the manuscript.
Corresponding author
Ethics declarations
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
774_2020_1105_MOESM1_ESM.jpg
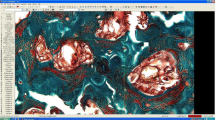
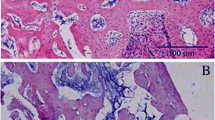
Supplementary file1. Fig.1S. Histological examination of the tibial metaphyseal at 12 weeks after bilateral ovariectomy (H&E staining; × 100): a OVX group, b Sham group. The scale bar represents 100 μm. c DXA examination of the tibial metaphyseal at 12 weeks after bilateral ovariectomy, n = 5 specimens/group. Data are expressed as mean ± SD, error bars in the figure indicate SD. ★p < 0.05 vs. Sham group. d Fracture was generated by a transverse osteotomy at the proximal one third of the tibiae (JPG 840 kb)
774_2020_1105_MOESM2_ESM.jpg
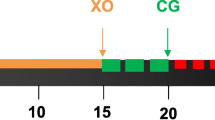
Supplementary file2. Fig.2S. The scheme of our study design. OVX ovariectomized, DXA dual dual-energy x-ray absorptiometry, RT-PCR reverse transcription-polymerase chain reaction (JPG 818 kb)
774_2020_1105_MOESM3_ESM.jpg
Supplementary file3. Fig.3S. Values of BMD (a) and ultimate force (b) of the contralateral tibial metaphysic, n = 6 specimens/group. Data are expressed as mean ± SD, error bars in the figure indicate SD. ★p < 0.05 vs. control group (JPG 653 kb)
About this article
Cite this article
Li, W., Hu, J., Ji, P. et al. Oral administration of bovine lactoferrin accelerates the healing of fracture in ovariectomized rats. J Bone Miner Metab 38, 648–657 (2020). https://doi.org/10.1007/s00774-020-01105-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-020-01105-1