Abstract
Background
To identify patients with concordant seizure semiology, interictal epileptiform discharges on standard EEG and brain MRI changes to define the patients with pharmacoresistant epilepsy (PRE) who would be suitable for epilepsy surgery according to non-invasive protocol.
Methods
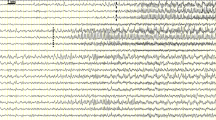
The medical records of the patients with epilepsy seen in Epilepsy Center of Institute of Neurology and Neuropsychology (ECINN) (Tbilisi, Georgia) were reviewed retrospectively. The diagnostic work-up included neurological examination, standard EEG, and MRI. The degree of concordance of the seizure semiology, EEG, and neuroimaging was used to determine the potential candidates for surgery. The probability of seizure freedom rate was estimated based on known predictive values of anatomical, electrophysiological, and semiological characteristics.
Results
A total of 83 (25 %) patients met the criteria of PRE. Fourteen (17 %) patients had complete concordance of seizure semiology, MRI, and EEG. Out of these patients, 11 had mesial temporal sclerosis on MRI and three had focal cortical dysplasia (FCD). Estimated seizure-free surgical success rate in this group was 75–95 % without the need for further investigations. Out of 25 (30 %) non-lesional MRI cases, the concordance of seizure semiology and EEG was in nine patients with probable success rate up to 60 %. Thirteen patients (16 %) had discordant EEG and MRI data and were not suitable for surgery without further testing.
Conclusions
A significant portion of PRE patients with concordant anatomical, electrophysiological, and semiological characteristics can be treated surgically in resource-limited countries. Nevertheless, most patients will still require further investigation for proper localization of epileptogenic focus.
Similar content being viewed by others
References
Berg AT, Walczak T, Hirsch LJ, Spencer SS (1998) Multivariable prediction of seizure outcome one year after resective epilepsy surgery: development of a model with independent validation. Epilepsy Res 29:185–194
Berg AT, Zelko FA, Levy SR, Testa FM (2012) Age at onset of epilepsy, pharmacoresistance, and cognitive outcomes: a prospective cohort study. Neurology 79:1384–1391
Boesebeck F, Schulz R, May T, Ebner A (2002) Lateralizing semiology predicts the seizure outcome after epilepsy surgery in the posterior cortex. Brain 125:2320–2331
Bonini F, Mc Gonigal A, Trebuchon A, Gavaret M, Bartolomei F, Giusiano B, Chauvel P (2014) Frontal lobe seizures: from clinical semiology to localization. Epilepsia 55:264–277
Burkholder DB, Sulc V, Hoffman EM, Cascino GD, Britton JW, So EL, Marsh WR, Meyer FB, Van Gompel JJ, Giannini C, Wass CT, Watson RE Jr, Worrell GA (2014) Interictal scalp electroencephalography and intraoperative electrocorticography in magnetic resonance imaging–negative temporal lobe epilepsy surgery. JAMA Neurol 71:702–709
Campos MG (2012) Epilepsy surgery in developing countries. Handb Clin Neurol 108:943–953
Campos MG, Godoy J, Mesa MT, Torrealba G, Gejman R, Huete I (2000) Temporal lobe epilepsy surgery with limited resources: results and economic considerations. Epilepsia 41(4):S18–S21
Cascino GD, Trenerry MR, So EL, Sharbrough FW, Shin C, Lagerlund TD, Zupanc ML, Jack CR Jr (1996) Routin EEG and temporal lobe epilepsy: relation to long-term EEG monitoring, quantitative MRI, and operative outcome. Epilepsia 37(7):651–656
Census (2015) Number of Population as of January 1, 2015 http://census.ge/en/saqartvelos-mosakhleobis-ritskhovnoba-2015-tslis-1-ianvris-mdgomareobit/184#.VVZNHvC79TR. Accessed 12 May 2015
Commission of Classification and Terminology of the ILAE (1981) Proposal for revised clinical and electroencephalographic classification of epileptic seizures. Epilepsia 22:489–501
Dolezalová I, Brázdil M, Hermanová M, Janousová E, Kuba R (2014) Effect of partial drug withdrawal on the lateralization of interictal epileptiform discharges and its relationship to surgical outcome in patients with hippocampal sclerosis. Epilepsy Res 108:1406–1416
Dworetzky BA, Reinsberger C (2011) The role of the interictal EEG in selecting candidates for resective epilepsy surgery. Epilepsy Behav 20:167–171
Engel J Jr (2014) Approaches to refractory epilepsy. Ann Indian Acad Neurol 17(1):S12–S17
Engel J Jr, International League Against Epilepsy (ILAE) (2001) A proposed diagnostic scheme for people with epileptic seizures and with epilepsy: report of the ILAE task force on classification and terminology. Epilepsia 42:796–803
Foldvary-Schaefer N, Unnwongse K (2011) Localizing and lateralizing features of auras and seizures. Epilepsy Behav 20:160–166
Gilliam F, Faught E, Martin R, Bowling S, Bilir E, Thomas J, Kuzniecky R (2000) Predictive value of MRI-identified mesial temporal sclerosis for surgical outcome in temporal lobe epilepsy: an intent-to-treat analysis. Epilepsia 41(8):963–966
Jeha LE, Najm I, Bingaman W, Dinner D, Widdess-Walsh P, Luders H (2007) Surgical outcome and prognostic factors of frontal lobe epilepsy surgery. Brain 130:574–584
Kwan P, Arzimanoglou A, Berg AT, Brodie MJ, Allen Hauser W, Mathern G, Moshé SL, Perucca E, Wiebe S, French J (2010) Definition of drug-resistant epilepsy: consensus proposal by the ad hoc Task Force of the ILAE Commission on Therapeutic Strategies. Epilepsia 51:1069–1077
Kwan P, Schachter SC, Brodie MJ (2011) Drug-resistant epilepsy. N Engl J Med 369:919–926
Laxer KD, Trinka E, Hirsch LJ, Cendes F, Langfitt J, Delanty N, Resnick T, Benbadis SR (2014) The consequences of refractory epilepsy and its treatment. Epilepsy Behav 37:59–70
Lomidze G, Kasradze S, Kvernadze D, Okujava N, Toidze O, de Boer HM, Dua T, Sander JW (2012) The prevalence and treatment gap of epilepsy in Tbilisi, Georgia. Epilepsy Res 98(2–3):123–129
Mc Gonigal A, Chauvel P (2004) Frontal lobe epilepsy: seizure semiology and presurgical evaluation. Pract Neurol 4:260–273
Mosewich RK, So EL, O’Brien TJ, Cascino GD, Sharbrough FW, Marsh WR, Meyer FB, Jack CR, O’Brien PC (2000) Factors predictive of the outcome of frontal lobe epilepsy surgery. Epilepsia 41:843–849
Noe K, Sulc V, Wong-Kisiel L, Wirrell E, Van Gompel JJ, Wetjen N, Britton J, So E, Cascino GD, Marsh WR, Meyer F, Horinek D, Giannini C, Watson R, Brinkmann BH, Stead M, Worrel GA (2013) Long-term outcomes after nonlesional extratemporal lobe epilepsy surgery. JAMA Neurol 70:1003–1008
Ngugi AK, Bottomley C, Kleinschmidt I, Sander JW, Newton CR (2010) Estimation of the burden of active and life-time epilepsy: a meta-analytic approach. Epilepsia 51:883–890
Ngugi AK, Kariuki SM, Bottomley C, Kleinschmidt I, Sander JW, Newton CR (2011) Incidence of epilepsy—a systematic review and meta-analysis. Neurology 77:1005–1012
Radhakrishnan K, So EL, Silbert PL, Jack CR Jr, Cascino GD, Sharbrough FW, O’Brien PC (1998) Predictors of outcome of anterior temporal lobectomy for intractable epilepsy: a multivariate study. Neurology 51:465–471
Schmidt D, Stavem K (2009) Long-term seizure outcome of surgery versus no surgery for drug-resistant partial epilepsy: a review of controlled studies. Epilepsia 50:1301–1309
Semah F, Picot MC, Adam C, Broglin D, Arzimanoglou A, Bazin B, Cavalcanti D, Baulac M (1998) Is the underlying cause of epilepsy a major prognostic factor for recurrence? Neurology 51:1256–1262
Spooner CG, Berkovic SF, Mitchell LA, Wrennall JA, Harvey AS (2006) New-onset temporal lobe epilepsy in children: lesion on MRI predicts poor seizure outcome. Neurology 67(12):2147–2153
Tatum WO, Benbadis SR, Hussain A, Al-Saadis S, Kaminski B, Heriaud LS, Fl V (2008) Ictal EEG remains the prominent predictor of seizure-free outcome after temporal lobectomy in epileptic patients with normal brain MRI. Seizure 17:631–636
Téllez-Zenteno JF, Hernández Ronquillo L, Moien-Afshari F, Wiebe S (2010) Surgical outcomes in lesional and non-lesional epilepsy: a systematic review and meta-analysis. Epilepsy Res 89:310–318
Tonini C, Beghi E, Berg AT, Bogliun G, Giordano, Newton RW, Tetto A, Vitelli E, Vitezic D, Wiebe S (2004) Predictors of epilepsy surgery outcome: a meta-analysis. Epilepsy Res 62:75–87
Wassenaar M, Leijten FSS, Egberts TCG, Moons KGM, Uijl SG (2013) Prognostic factors for medically intractable epilepsy: a systematic review. Epilepsy Res 106:301–310
Acknowledgments
The study was performed within the frame of the Shota Rustaveli National Science Foundation’s Grant “Epidemiology and risk factors of pharmacoresistant epilepsy in Georgia” (Project number DI/40/8-313/11). We are grateful to G. Kutchuchidze, T. Tchintcharauli, T. Kobulashvili, D. Kvernadze, K. Geladze, and M. Khvadagiani for providing support for the implementation of the project. We are grateful to M. Okujava for reviewing the MRIs.
Ethical standards
The study was scrutinized and approved by the National Committee of Bioethics and was carried with full adherence to the principles of the Declaration of Helsinki, 1964. Before inclusion in the study, all participants gave informed consent.
Conflict of interest
The funding source has not been involved in the collection, analysis and interpretation of data, in the writing of the report, or in the decision to submit the article for publication. GL, GJ and SK were paid for their job within the grant DI/40/8-313/11. None of other authors have conflict of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
This study is trying to establish arguments to overcome the problem of establishing an epilepsy surgery center in a country where resources to create new cost-intensive treatments is difficult. It is well known that presurgical evaluation can frequently be expensive due to the necessity to have video EEG places with round-the-clock monitoring personnel. In addition, a whole group of experts is needed, such as EEG technicians, epileptologists, experienced EEG readers, neuropsychologists, a modern era MRI, and, as another source of high expense, the technology of implanted electrode evaluations. This problem is certainly not restricted to Georgia; there are other countries in Europe and around the world that are in the same situation.
The authors have done a good job of carefully reviewing the literature and using the data obtained from the literature to identify potential candidates for epilepsy surgery from their annual patient load. They were able to identify 83 potential candidates with drug-resistant epilepsy who in theory would deserve to be evaluated if they are suitable candidates for epilepsy surgery. The paper is obviously written with the intention to convince the local authorities to invest the money for the creation of an epilepsy surgery service. The calculations are based on good data. The study was carefully done, and I think the conclusions are correct. The numbers they found are in accordance with the percentages known from other countries. The study was performed by a neurology group specialized in epileptology and is indirectly related to neurosurgery by pointing out that even with limited resources, for example no intracranial electrode placement, it is still possible to identify surgical candidates. This was done in a convincing fashion.
These arguments may be useful for other joint neurology/neurosurgery groups who want to convince their administrations to establish an epilepsy surgery center.
Johannes Schramm
Bonn, Germany
The authors present a study looking to justify the setting up of an epilepsy surgery program for Georgia (population of 4 million) based on seizure semiology, inter-ictal EEG, and MRI. Temporal lobe epilepsy remains the “mainstay” of adult epilepsy surgery and the authors estimate a “pool” of over 400 cases of MTS in the country, many of which will be potential surgical candidates. Considering that surgery for MTS is one of the few neurosurgical procedures for which there is class I evidence, and with a high chance of rendering the patients seizure free (and hence being highly cost effective), this is the obvious cohort on which to initially develop the service. It is surprising that this study did not identify more glioneuronal tumors—another cohort of lesional epilepsy cases, which are potentially good surgical candidates. For left mesial temporal lesions, some form of memory assessment would add to the pre-evaluation work-up. To undertake non-lesional work on the basis of such a limited assessment may prove more challenging and less rewarding—especially when one considers the Mayo Clinic experience where only 11 % of extra-temporal non-lesional cases had an excellent outcome.
Interestingly, the rate of MTS appears to be decreasing in most developed counties and, despite guidelines, the numbers of patients receiving surgery has always fallen well short of the predicted numbers of patients who might benefit from such surgery. While the authors have supplied good evidence for the need of a service in Georgia, we suspect that once the “backlog” of cases (resulting in a high prevalence) is dealt with, the incidence of new cases coming to surgery will be more modest than that predicted by the authors.
Paul Chumas
Leeds, UK
1. Wiebe S, Blume WT, Girvin JP, Eliasziw M (2001) Effectiveness and Efficiency of Surgery for Temporal Lobe Epilepsy Study Group: a randomized, controlled trial of surgery for temporal-lobe epilepsy. N Eng J Med 345: 311–318
2. Noe K, Sulc V, Wong-Kisiel L, Wirrell E, Van Gompel JJ, Wetjen N, Britton J, So E, Cascino GD, Marsh WR, Meyer F, Horinek D, Giannini C, Watson R, Brinkmann BH, Stead M, Worrell GA (2013) Long-term outcomes after nonlesional extratemporal lobe epilepsy surgery. JAMA Neurol 70:1003–1008
3. Englot DJ, Ouyang D, Garcia PA, Barbaro NM, Chang EF(2012) Epilepsy surgery trends in the United States, 1990–2008. Neurology 78:1200–1206, 2012
4. Van Gompel JJ, Ottman R, Worrell GA, Marsh R, Wetjen NM, Cascino GD, Meyer FB(2012) Use of anterior temporal lobectomy for epilepsy in a community-based population. Arch Neurol 69: 1476–1481
Rights and permissions
About this article
Cite this article
Kasradze, S., Alkhidze, M., Lomidze, G. et al. Perspectives of epilepsy surgery in resource-poor countries: a study in Georgia. Acta Neurochir 157, 1533–1540 (2015). https://doi.org/10.1007/s00701-015-2496-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-015-2496-3