Abstract
Purpose
Saliva is often used as a tool for identifying systemic diseases because of the noninvasive nature of its collection. Moreover, salivary metabolites can be potential predictive factors for postoperative survival. We conducted the present study to establish whether salivary metabolites can function as predictive biomarkers for lung surgery complications.
Methods
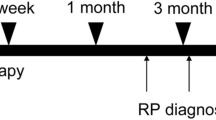
Unstimulated salivary samples were collected from 412 patients before lung surgery. Salivary metabolites were analyzed comprehensively by capillary electrophoresis mass spectrometry. Clinical data with the discriminatory ability of biomarkers were assessed to predict lung surgery complications using multivariate logistic regression analysis. The primary endpoint was the risk factors for postoperative complications of Clavien–Dindo grade ≥ III.
Results
Postoperative complications of Clavien–Dindo grade ≥ III developed in 36 patients (8.7%). There was no postoperative 30-day mortality. Male sex (odds ratio [OR], 3.852; 95% confidence interval CI 1.455–10.199; p = 0.007) and salivary gamma-butyrobetaine (OR, 0.809; 95% CI 0.694–0.943; p = 0.007) were identified as significant risk factors for postoperative complications of Clavien–Dindo grade ≥ III.
Conclusion
Salivary metabolites are potential noninvasive biomarkers for predicting postoperative complications of lung surgery.

Similar content being viewed by others
Data availability statement
Data cannot be shared for privacy or ethical reasons but are available from the corresponding author on reasonable request, subject to permission from the ethics committee of Yamagata University.
References
Cattaneo SM, Park BJ, Wilton AS, Seshan VE, Bains MS, Downey RJ, et al. Use of video-assisted thoracic surgery for lobectomy in the elderly results in fewer complications. Ann Thorac Surg. 2008;85:231–5.
O’Sullivan KE, Kreaden US, Hebert AE, Eaton D, Redmond KC. A systematic review and meta-analysis of robotic versus open and video-assisted thoracoscopic surgery approaches for lobectomy. Interact Cardiovasc Thorac Surg. 2019;28:526–34.
Aiolfi A, Nosotti M, Micheletto G, Khor D, Bonitta G, Perali C, et al. Pulmonary lobectomy for cancer: systematic review and network meta-analysis comparing open, video-assisted thoracic surgery, and robotic approach. Surgery. 2021;169:436–46.
Galata C, Karampinis I, Roessner ED, Stamenovic D. Risk factors for surgical complications after anatomic lung resections in the era of VATS and ERAS. Thorac Cancer. 2021;12:3255–62.
Suzuki K, Saji H, Aokage K, Watanabe SI, Okada M, Mizusawa J, et al. Comparison of pulmonary segmentectomy and lobectomy: safety results of a randomized trial. J Thorac Cardiovasc Surg. 2019;158:895–907.
Motono N, Ishikawa M, Iwai S, Iijima Y, Usuda K, Uramoto H. Individualization of risk factors for postoperative complication after lung cancer surgery: a retrospective study. BMC Surg. 2021;21:311.
Shiono S, Katahira M, Abiko M, Sato T. Smoking is a perioperative risk factor and prognostic factor for lung cancer surgery. Gen Thorac Cardiovasc Surg. 2015;63:93–8.
Al Sawalhi S, Ding J, Vannucci J, Li Y, Odeh A, Zhao D. Perioperative risk factors for atrial fibrillation (AF) in patients underwent uniportal video-assisted thoracoscopic (VATS) pneumonectomy versus open thoracotomy: single center experience. Gen Thorac Cardiovasc Surg. 2021;69:487–96.
Ueda T, Suzuki K, Matsunaga T, Takamochi K, Oh S. Postoperative atrial fibrillation is less frequent in pulmonary segmentectomy compared with lobectomy. Gen Thorac Cardiovasc Surg. 2018;66:95–100.
Takamori S, Oizumi H, Suzuki J, Watanabe H, Sato K, Saito S, et al. Thoracoscopic anatomical individual basilar segmentectomy. Eur J Cardiothorac Surg. 2022;62:eazab509.
Takamori S, Oizumi H, Suzuki J, Suzuki K, Kabasawa T. Video-assisted thoracoscopic segmentectomy for deep and peripheral small lung cancer. Thorac Cardiovasc Surg. 2022;70:233–8.
Sano Y, Okazaki M, Shigematsu H, Yamashita N, Sugimoto R, Sakao N, et al. Quality of life after partial lung resection with uniportal versus 3-port video-assisted thoracoscopic surgery: a prospective randomized controlled study. Surg Today. 2021;51:1755–63.
Rodríguez-Fuster A, Belda-Sanchis J, Aguiló R, Embun R, Mojal S, Call S, et al. Morbidity and mortality in a large series of surgical patients with pulmonary metastases of colorectal carcinoma: a prospective multicentre Spanish study (GECMP-CCR-SEPAR). Eur J Cardiothorac Surg. 2014;45:671–6.
Lo Faso F, Solaini L, Lembo R, Bagioni P, Zago S, Soliani P, et al. Thoracoscopic lung metastasectomies: a 10-year, single-center experience. Surg Endosc. 2013;27:1938–44.
Okada S, Shimada J, Teramukai S, Kato D, Tsunezuka H, Miyata N, et al. Risk stratification according to the prognostic nutritional index for predicting postoperative complications after lung cancer surgery. Ann Surg Oncol. 2018;25:1254–61.
Tvarijonaviciute A, Martinez-Lozano N, Rios R, Marcilla de Teruel MC, Garaulet M, Cerón JJ. Saliva as a non-invasive tool for assessment of metabolic and inflammatory biomarkers in children. Clin Nutr. 2020;39:2471–8.
Takamori S, Ishikawa S, Suzuki J, Oizumi H, Uchida T, Ueda S, et al. Differential diagnosis of lung cancer and benign lung lesion using salivary metabolites: a preliminary study. Thorac Cancer. 2022;13:460–5.
Bel’skaya LV, Sarf EA, Kosenok VK, Gundyrev IA. Biochemical markers of saliva in lung cancer: diagnostic and prognostic perspectives. Diagnostics. 2020. https://doi.org/10.3390/diagnostics10040186.
Ishikawa S, Ishizawa K, Tanaka A, Kimura H, Kitabatake K, Sugano A, et al. Identification of salivary proteomic biomarkers for oral cancer screening. In Vivo. 2021;35:541–7.
Ishikawa S, Sugimoto M, Konta T, Kitabatake K, Ueda S, Edamatsu K, et al. Salivary metabolomics for prognosis of oral squamous cell carcinoma. Front Oncol. 2021;11: 789248.
Katayama H, Kurokawa Y, Nakamura K, Ito H, Kanemitsu Y, Masuda N, et al. Extended Clavien-Dindo classification of surgical complications: Japan clinical oncology group postoperative complications criteria. Surg Today. 2016;46:668–85.
Clavien PA, Sanabria JR, Strasberg SM. Proposed classification of complications of surgery with examples of utility in cholecystectomy. Surgery. 1992;111:518–26.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Henson BS, Wong DT. Collection, storage, and processing of saliva samples for downstream molecular applications. Methods Mol Biol. 2010;666:21–30.
Ishikawa S, Sugimoto M, Kitabatake K, Sugano A, Nakamura M, Kaneko M, et al. Identification of salivary metabolomic biomarkers for oral cancer screening. Sci Rep. 2016;6:31520.
Ishikawa S, Sugimoto M, Kitabatake K, Tu M, Sugano A, Yamamori I, et al. Effect of timing of collection of salivary metabolomic biomarkers on oral cancer detection. Amino Acids. 2017;49:761–70.
Sugimoto M, Wong DT, Hirayama A, Soga T, Tomita M. Capillary electrophoresis mass spectrometry-based saliva metabolomics identified oral, breast and pancreatic cancer-specific profiles. Metabolomics. 2010;6:78–95.
Bremer J. Carnitine—metabolism and functions. Physiol Rev. 1983;63:1420–80.
Rebouche CJ. Effect of dietary carnitine isomers and gamma-butyrobetaine on L-carnitine biosynthesis and metabolism in the rat. J Nutr. 1983;113:1906–13.
Rebouche CJ, Chenard CA. Metabolic fate of dietary carnitine in human adults: identification and quantification of urinary and fecal metabolites. J Nutr. 1991;121:539–46.
Sandstedt S, Larsson J, Cederblad G. Carnitine levels in skeletal muscle of malnourished patients before and after total parenteral nutrition. Clin Nutr. 1986;5:227–30.
Adeva-Andany MM, Calvo-Castro I, Fernández-Fernández C, Donapetry-García C, Pedre-Piñeiro AM. Significance of l-carnitine for human health. IUBMB Life. 2017;69:578–94.
Arduini A, Gorbunov N, Arrigoni-Martelli E, Dottori S, Molajoni F, Russo F, et al. Effects of l-carnitine and its acetate and propionate esters on the molecular dynamics of human erythrocyte membrane. Biochim Biophys Acta. 1993;1146:229–35.
Shingu Y, Katoh N, Ooka T, Katoh H, Wakasa S. L-carnitine supplementation for the prevention of postoperative atrial fibrillation in aortic valve surgery. Gen Thorac Cardiovasc Surg. 2021;69:1460–6.
Dastan F, Talasaz AH, Mojtahedzadeh M, Karimi A, Salehiomran A, Bina P, et al. Randomized trial of carnitine for the prevention of perioperative atrial fibrillation. Semin Thorac Cardiovasc Surg. 2018;30:7–13.
Hino H, Karasaki T, Yoshida Y, Fukami T, Sano A, Tanaka M, et al. Risk factors for postoperative complications and long-term survival in lung cancer patients older than 80 years. Eur J Cardiothorac Surg. 2018;53:980–6.
Rueth NM, Parsons HM, Habermann EB, Groth SS, Virnig BA, Tuttle TM, et al. Surgical treatment of lung cancer: predicting postoperative morbidity in the elderly population. J Thorac Cardiovasc Surg. 2012;143:1314–23.
Endo S, Ikeda N, Kondo T, Nakajima J, Kondo H, Yokoi K, et al. Model of lung cancer surgery risk derived from a Japanese nationwide web-based database of 78 594 patients during 2014–2015. Eur J Cardiothorac Surg. 2017;52:1182–9.
Ishikawa S, Yamamori I, Takamori S, Kitabatake K, Edamatsu K, Sugano A, et al. Evaluation of effects of perioperative oral care intervention on hospitalization stay and postoperative infection in patients undergoing lung cancer intervention. Support Care Cancer. 2021;29:135–43.
Kaga A, Ikeda T, Tachibana K, Tanaka R, Kondo H, Kawabata T, et al. An innovative oral management procedure to reduce postoperative complications. JTCVS Open. 2022;10:442–53.
Acknowledgements
This work was supported by grants from YU-COE(C) from Yamagata University. The authors thank all patients who provided the samples.
Funding
This work was supported by grants from YU-COE(C) from Yamagata University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We have no conflicts of interest to declare.
Informed consent
Informed consent was obtained from all participants included in the study. Written informed consent was obtained from all participants in the original study. In the present study, the participants were given the option to opt out online. None of the patients declined to participate.
Statement of human and/or animal rights
The Institutional Review Board Ethics Committee approved the study (IRB #2022–131, August 29, 2022).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
595_2024_2794_MOESM1_ESM.docx
Supplementary file1 (DOCX 23 KB) Table S1. Median salivary metabolite values in each group (patients without complications, patients with complications of Clavien–Dindo grade I and II, and patients with complications of Clavien–Dindo grade IIIa and IIIb). Table S2. Postoperative complications of Clavien–Dindo grade ≥ I.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Takamori, S., Ishikawa, S., Sato, K. et al. Salivary metabolites as potential predictive biomarkers for lung surgery complications: a retrospective cross-sectional study. Surg Today (2024). https://doi.org/10.1007/s00595-024-02794-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00595-024-02794-1