Abstract
Purpose
This study compared the quality of healthcare before and after implementation of a policy restructuring the healthcare delivery system and estimated the impact of centralization.
Methods
We used the National Clinical Database to study patients undergoing esophagectomies from 2011 to 2016. We compared the effect of centralization based on the patient background, surgical mortality, and year of surgery. Difference-in-difference methods based on the generalized estimating equation logistic regression model were used for before-and-after comparisons after adjusting for patient-level expected surgical mortality.
Results
In total, 34,640 cases were identified. More cases with risk factors were noted in ultra-low-volume hospitals, where 38.4% of cases in underpopulated areas were treated, than in higher volume facilities, and the operative mortality, readmission within 30 days and length of stay were worse among patients treated in these hospitals. In centralized prefectures, the number of cases per hospital increased over time (7.2 in 2011 to 9.5 in 2016) while the crude operative mortality tended to decrease (3.4% in 2011 to 1.8% in 2016). The difference-in-difference estimator was 0.856 (95% confidence interval: 0.639–1.147, p = 0.298).
Conclusion
The centralization of ultra-low-volume hospitals did not lead to a deterioration in the quality of care but rather an improving trend.



Similar content being viewed by others
Change history
11 April 2021
A Correction to this paper has been published: https://doi.org/10.1007/s00595-021-02261-1
Abbreviations
- Alb:
-
Albumin
- ADL:
-
Activity of daily life
- CD:
-
Clavien–Dindo
- COPD:
-
Chronic obstructive pulmonary disease
- NCD:
-
National Clinical Database
- PT-INR:
-
Prothrombin time-international normalized ratio
- BUN:
-
Blood urea nitrogen
- WBC:
-
White blood cell
References
Shibuya K, Hashimoto H, Ikegami N, Nishi A, Tanimoto T, Miyata H, et al. Future of Japan’s system of good health at low cost with equity: beyond universal coverage. Lancet. 2011;378:1265–73.
White Paper on Aging Society 2019 (Entire Version) Aging Population in Japan. Cabinet Office. https://www8.cao.go.jp/kourei/whitepaper/w-2019/html/zenbun/s1_1_1.html (Access: 2020/7/1) In Japanese.
Hashimoto H, Ikegami N, Shibuya K, Izumida N, Noguchi H, Yasunaga H, et al. Cost containment and quality of care in Japan: is there a trade-off? Lancet. 2011;378:1174–82.
Outline of the act on the improvement of related laws to promote comprehensive medical and nursing care services in local communities. Ministry of health, labour and welfare notice. https://www.mhlw.go.jp/topics/bukyoku/soumu/houritu/dl/186-07.pdf. Accessed 1 July 2020. (In Japanese).
About the corporation for promotion of regional medical cooperation. https://www.mhlw.go.jp/content/000328791.pdf. Accessed 1 July 2020. (In Japanese).
Takahashi A, Miyata H. Establishment of a regional medical coordination system that makes effective use of limited resources and an understanding of the current situation. Nomura Healthcare Note. 2018; No.18–6 (In Japanese).
List of restructured integrated medical institutions. The 24th working group on regional medical care plan. https://www.mhlw.go.jp/content/10800000/000551037.pdf. Accessed 1 July 2020. (In Japanese).
Abe H, Tsukada K, Takada T, Ngakawa T. The selection of pancreatic reconstruction techniques gives rise to higher incidences of morbidity: results of the 30th Japan pancreatic surgery questionnaire survey on pancreatoduodenectomy in Japan. J Hepatobiliary Pancreat Surg. 2005;12:109–15.
Nomura E, Tsukuma H, Ajiki T, Oshima A. Population-based study of relationship between hospital surgical volume and 5-year survival of stomach cancer patients in Osaka Japan. Cancer Sci. 2003;94:998–1002.
Birkmeyer JD, Siewers AE, Finlayson EVA, Stukel TA, Lucas FL, Batista I, et al. Hospital volume and surgical mortality in the united states. N Engl J Med. 2002;346(15):1128–37.
Birkmeyer JD, Siewers AE, Marth NJ, Goodman DC. Regionalization of high-risk surgery and implications for patient travel times. JAMA. 2003;290(20):2703–8.
Miyata H, Motomura N, Ueda Y, Matsuda H, Takamoto S. Effect of procedural volume on outcome of coronary artery bypass graft surgery in Japan: implication toward public reporting and minimal volume standards. J Thorac Cardiovasc Surg. 2008;135:1306–12.
Nishigori T, Miyata H, Okabe H, Toh Y, Matsubara H, Konno H, et al. Impact of hospital volume on risk-adjusted mortality following oesophagectomy in Japan. Br J Surg. 2016;103(13):1880–6.
Markar SR, Karthikesalingam A, Thrumurthy S, Low DE. Volume-outcome relationship in surgery for esophageal malignancy: systematic review and meta-analysis 2000–2011. J Gastrointest Surg. 2012;16(5):1055–63.
Finks JF, Osborne NH, Birkmeyer JD. Trends in hospital volume and operative mortality for high-risk surgery. N Engl J Med. 2011;364(22):2128–37.
Sheetz KH, Dimick JB, Nathan H. Centralization of high-risk cancer surgery within existing hospital systems. J Clin Oncol. 2019;37(34):3234–42.
OECD_Hospital beds. https://data.oecd.org/healtheqt/hospital-beds.htm (Access: 2020/7/1)
National Clinical Database. http://www.ncd.or.jp/. Accessed 1 July 2020. (In Japanese)
Tomotaki A, Kumamaru H, Hashimoto H, Takahashi A, Ono M, Iwanaka T, et al. Evaluating the quality of data from the Japanese National Clinical Database 2011 via a comparison with regional government report data and medical charts. Surg Today. 2019;49(1):65–71.
Takahashi A, Kumamaru H, Tomotaki A, Matsumura G, Fukuchi E, Hirata Y, et al. Verification of data accuracy in Japan congenital cardiovascular surgery database including its postprocedural complication reports. World J Pediatr Congenit Heart Surg. 2018;9(2):150–6.
Kanaji S, Takahashi A, Miyata H, Marubashi S, Kakeji Y, Konno H, et al. (2019) Initial verification of data from a clinical database of gastroenterological surgery in Japan. Surg Today 49:328–333.
Anazawa T, Paruch JL, Miyata H, Gotoh M, Ko CY, Cohen ME, et al. Comparison of national operative mortality in gastroenterological surgery using web-based prospective data entry systems. Med (Baltim). 2015;94(e2194):37.
Marubashi S, Liu JY, Miyata H, Cohen ME, Ko CY, Seto Y, et al. Surgical quality improvement programs in Japan and USA: report from the collaborative projects between Japanese society of gastroenterological surgery and American college of surgeons national surgical quality improvement program. Ann Gastroenterol Surg. 2019;3:343–51.
Takeuchi H, Miyata H, Gotoh M, Kitagawa Y, Baba H, Kimura W, et al. A risk model for esophagectomy using data of 5354 patients included in a Japanese nationwide web-based database. Ann Surg. 2014;260(2):259–66.
Takahashi T. (2020) Reconstruction of the medical and welfare provision system that takes into account regional differences in the peak demand for medical care and the level of medical and welfare resources. Document on the 9th national assembly on the reform of social insurance system. https://www.mhlw.go.jp/stf/shingi/2r98520000030swa-att/2r98520000030t1k.pdf. Accessed 1 July 2020. (In Japanese)
Nishigori T, Takahashi A, Ichihara N, Tsunoda S, Toh Y, Watanabe M, et al. (2019) Simulation study on regionalization of esophagectomy using data of 27,576 patients with esophageal malignant tumor. J Clin Oncol. 37(4):151–151. 2019 Gastrointestinal Cancers Symposium https://ascopubs.org/doi/abs/https://doi.org/10.1200/JCO.2019.37.4_suppl.151. Accessed 28 Aug 2020.
Ingraham AM, Richards KE, Hall BL, Ko CY. Quality improvement in surgery: the American college of surgeons national surgical quality improvement program approach. Adv Surg. 2010;44:251–67.
Feudtner C, Berry JG, Parry G, Hain P, Morse RB, Slonim AD, et al. Statistical uncertainty of mortality rates and rankings for children’s hospitals. Pediatrics. 2011;128:e966–72.
Orley A, David C. Using the longitudinal structure of earnings to estimate the effect of training programs. Rev Econom Statis. 1985;67(4):648–60.
Justin BD, Andrew MR. Methods for evaluating changes in healthcare policy: the difference-in-differences approach. JAMA. 2014;312(22):2401–2.
Ravi R, Jeanette WC, Andrew TJ, Mark EC, Allison RD, Clifford YK, et al. Association of the 2011 ACGME resident duty hour reform with general surgery patient outcomes and with resident examination performance. JAMA. 2014;312(22):2374–84.
Reames BN, Ghaferi AA, Birkmeyer JD, Dimick JB. Hospital volume and operative mortality in the modern era. Ann Surg. 2014;260(2):244–51.
Yasuyuki S. National clinical database (NCD) shows the trend for centralization of major surgery: should it depend on hospital or surgeon volume ? Ann Gastroenterol Surg. 2019;3(4):340–2.
Kakeji Y, Takahashi A, Udagawa H, Unno M, Endo I, Kunisaki C, et al. Surgical outcomes in gastroenterological surgery in Japan: report of national clinical database 2011–2016. Ann Gastroenterol Surg. 2018;2(1):37–54.
Miyata H, Motomura N, Takamoto S. Regionalization of cardiac surgery in Japan I. Effect of procedural volume on outcome of CABG surgery. Kyobu Geka. 2007a;60:334–43. (In Japanese).
Miyata H, Kondo JM, Motomura N, Fushimi K, Takamoto S. Regionalization of cardiac surgery in Japan II. Estimating the multiple effect of regionalization in cardiac surgery. Kyobu Geka. 2007;60:747–53. (In Japanese).
Konno H, Kamiya K, Kikuchi H, Miyata H, Hirahara N, Gotoh M, et al. Association between the participation of board-certified surgeons in gastroenterological surgery and operative mortality after eight gastroenterological procedures. Surg Today. 2017;47:611–8.
Toh Y, Yamamoto H, Miyata H, Gotoh M, Watanabe M, Matsubara H, et al. Significance of the board-certified surgeon systems and clinical practice guideline adherence to surgical treatment of esophageal cancer in Japan: a questionnaire survey of departments registered in the National Clinical Database. Esophagus. 2019;16(4):362–70.
Shahian DM. Improving cardiac surgery quality–volume, outcome, process? JAMA. 2004;291:246–8.
Postma J, Jerak TZ. Beyond volume indicators and centralization: toward a broad perspective on policy for improving quality of emergency care. Ann Emerg Med. 2017;69(6):689–97.
Greenberg CC, Stanley WA, Schrag D. Centralization of cancer surgery: what does it mean for surgical training? J Clin Oncol. 2009;27(28):4637–9.
Projected future population by prefecture. https://www.kantei.go.jp/jp/singi/shakaihoshoukaikaku/wg_dai2/siryou4.pdf. Accessed 1 July 2020. (In Japanese)
Vonlanthen R, Lodge P, Barkun JS, Farges O, Rogiers X, Soreide K, Kehlet H, et al. Toward a consensus on centralization in surgery. Ann Surg. 2018;268(5):712–24.
Stitzenberg KB, Sigurdson ER, Egleston BL, Starkey RB. Centralization of cancer surgery: implications for patient access to optimal care. J Clin Oncol. 2009;27(28):4671–8.
Izumisawa Y, Endo H, Ichihara N, Takahashi A, Nawata K, Shiraishi H, Miyata H, Motomura N. Association between prehospital transfer distance and surgical mortality in emergency thoracic aortic surgery. J Thorac Cardiovasc Surg. 2020;20:30709–11 (S0022-5223).
Acknowledgements
The author would like to thank all of the data administrators and hospitals who participated in the NCD project and put effort into data entry. The authors also thank Drs. T. Iwanaka, Y. Ueda, S. Takamoto, N. Motomura, Y. Tokuda, S, Endo, T, Okamoto, H. Kumamaru and N. Ichihara for their cooperation. This work was supported by a grant from the Ministry of Health, Labour and Welfare of Japan. A portion of the results of this study was presented at The 78th Annual Meeting of Japanese Society of Public Health (October 25, 2019; Kochi, Japan).
Funding
This work was supported by a grant from the Ministry of Health, Labour and Welfare of Japan.
Author information
Authors and Affiliations
Contributions
AT, HY, and HM planned the present study and wrote the manuscript. AT, HY, and HM analyzed the data. YK, SM, MG, and YS reviewed the manuscript and revised it critically for important intellectual content.
Corresponding author
Ethics declarations
Conflict of interest
Arata Takahashi, Hiroyuki Yamamoto, and Hiroaki Miyata are affiliated with the Department of Healthcare Quality Assessment at the University of Tokyo. The department is a social collaboration department supported by grants from the National Clinical Database, Johnson and Johnson K.K. and Nipro Co.; no other authors have any conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
595_2021_2245_MOESM1_ESM.docx
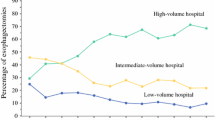
Supplementary file1 (DOCX 80 KB) Supplemental material: The percentage of hospitals performing fewer than two esophagectomy procedures per year in Japan (2011-2016). The percentage of hospitals performing fewer than two esophagectomy procedures per year and the percentage of esophagectomy procedures performed in those hospitals have been decreasing.
Rights and permissions
About this article
Cite this article
Takahashi, A., Yamamoto, H., Kakeji, Y. et al. Estimates of the effects of centralization policy for surgery in Japan: does centralization affect the quality of healthcare for esophagectomies?. Surg Today 51, 1010–1019 (2021). https://doi.org/10.1007/s00595-021-02245-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-021-02245-1