Abstract
Purpose
To investigate the relationship between sagittal plane characteristics of the spinal column and conservative treatment failure in acute osteoporotic spinal fractures (OSFs).
Methods
As a retrospective study of single-institute data, thoracolumbar OSF patients with similar propensities in terms of location of fractures and results of bone mineral density were analyzed. Among them, 43 patients (group I) who needed reconstructive surgical interventions and 39 patients (group II) who obtained successful treatment through conservative care were included. General demographic data, radiographic features of fractures, and magnetic resonance imaging (MRI) features of fractures were analyzed. To investigate the relationship between global sagittal alignment of the spine and occurrence of delayed complication following OSFs, radiological sagittal parameters were analyzed.
Results
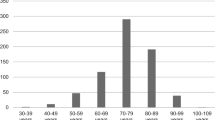
The number of cases requiring reconstructive surgery was significantly higher when the index vertebra showed diffuse or mid-portion bone marrow changes in MRI. In terms of sagittal parameters, pelvic incidence (group I 59.1° ± 11.9°, group II 54.6° ± 9.8°) and thoracolumbar angle (group I 26.5° ± 14.1°, group II 17.4° ± 11.2°) were significantly higher in group I. Logistic regression analysis showed that higher pelvic incidence (OR 1.09, 95% CI 1.01–1.18, p value < 0.05) and higher thoracolumbar angle (OR 1.09, 95% CI 1.02–1.17, p value < 0.05) were significant risk factors for delayed complications requiring reconstructive surgery following OSFs.
Conclusion
Delayed complications requiring reconstructive surgery following OSFs are related to sagittal plane parameters of the spine such as high pelvic incidences, in addition to previously known radiographic characteristics of fractures.





Similar content being viewed by others
References
Ha KY, Kim YH (2013) Risk factors affecting progressive collapse of acute osteoporotic spinal fractures. Osteoporos Int 24:1207–1213. https://doi.org/10.1007/s00198-012-2065-z
Goldstein S, Smorgick Y, Mirovsky Y, Anekstein Y, Blecher R, Tal S (2016) Clinical and radiological factors affecting progressive collapse of acute osteoporotic compression spinal fractures. J Clin Neurosci 31:122–126. https://doi.org/10.1016/j.jocn.2016.02.020
Longo UG, Loppini M, Denaro L, Maffulli N, Denaro V (2012) Osteoporotic vertebral fractures: current concepts of conservative care. Br Med Bull 102:171–189. https://doi.org/10.1093/bmb/ldr048
Kempinsky WH, Morgan PP, Boniface WR (1958) Osteoporotic kyphosis with paraplegia. Neurology 8:181–186. https://doi.org/10.1212/wnl.8.3.181
Tsujio T, Nakamura H, Terai H, Hoshino M, Namikawa T, Matsumura A, Kato M, Suzuki A, Takayama K, Fukushima W, Kondo K, Hirota Y, Takaoka K (2011) Characteristic radiographic or magnetic resonance images of fresh osteoporotic vertebral fractures predicting potential risk for nonunion: a prospective multicenter study. Spine (Phila Pa 1976) 36:1229–1235. https://doi.org/10.1097/BRS.0b013e3181f29e8d
Ohnishi T, Iwata A, Kanayama M, Oha F, Hashimoto T, Iwasaki N (2018) Impact of spino-pelvic and global spinal alignment on the risk of osteoporotic vertebral collapse. Spine Surg Relat Res 2:72–76. https://doi.org/10.22603/ssrr.2017-0046
Laouissat F, Sebaaly A, Gehrchen M, Roussouly P (2018) Classification of normal sagittal spine alignment: refounding the Roussouly classification. Eur Spine J 27:2002–2011. https://doi.org/10.1007/s00586-017-5111-x
Lee CS, Lee CK, Kim YT, Hong YM, Yoo JH (2001) Dynamic sagittal imbalance of the spine in degenerative flat back: significance of pelvic tilt in surgical treatment. Spine (Phila Pa 1976) 26:2029–2035. https://doi.org/10.1097/00007632-200109150-00017
Shimokawa T, Miyamoto K, Hioki A, Masuda T, Fushimi K, Ogawa H, Ohnishi K, Akiyama H (2022) Compensatory Pelvic Retro-Rotation Associated with a decreased quality of life in patients with normal sagittal balance. Asian Spine J 16:241–247. https://doi.org/10.31616/asj.2020.0449
Youn YH, Cho KJ, Na Y, Kim JS (2022) Global sagittal alignment and clinical outcomes after 1–3 short-segment lumbar fusion in degenerative spinal diseases. Asian Spine J 16:551–559. https://doi.org/10.31616/asj.2021.0182
Kim GU, Park WT, Chang MC, Lee GW (2022) Diagnostic technology for spine pathology. Asian Spine J 16:764–775. https://doi.org/10.31616/asj.2022.0374
Inose H, Kato T, Ichimura S, Nakamura H, Hoshino M, Togawa D, Hirano T, Tokuhashi Y, Ohba T, Haro H, Tsuji T, Sato K, Sasao Y, Takahata M, Otani K, Momoshima S, Yuasa M, Hirai T, Yoshii T, Okawa A (2020) Risk factors of nonunion after acute osteoporotic vertebral fractures: a prospective multicenter cohort study. Spine Phila Pa 45:895–902. https://doi.org/10.1097/brs.0000000000003413
Kanchiku T, Taguchi T, Kawai S (2003) Magnetic resonance imaging diagnosis and new classification of the osteoporotic vertebral fracture. J Orthop Sci 8:463–466. https://doi.org/10.1007/s00776-003-0665-3
Roussouly P, Gollogly S, Berthonnaud E, Dimnet J (2005) Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine Phila Pa 1976) 30:346–353
Sisodia GB (2013) Methods of predicting vertebral body fractures of the lumbar spine. World J Orthop 4:241–247. https://doi.org/10.5312/wjo.v4.i4.241
Baek SW, Kim C, Chang H (2015) The relationship between the spinopelvic balance and the incidence of adjacent vertebral fractures following percutaneous vertebroplasty. Osteoporos Int 26:1507–1513. https://doi.org/10.1007/s00198-014-3021-x
Borgström F, Sobocki P, Ström O, Jönsson B (2007) The societal burden of osteoporosis in Sweden. Bone 40:1602–1609. https://doi.org/10.1016/j.bone.2007.02.027
Ferrar L, Roux C, Felsenberg D, Glüer CC, Eastell R (2012) Association between incident and baseline vertebral fractures in European women: vertebral fracture assessment in the Osteoporosis and Ultrasound Study (OPUS). Osteoporos Int 23:59–65. https://doi.org/10.1007/s00198-011-1701-3
Garfin SR, Yuan HA, Reiley MA (2001) New technologies in spine: kyphoplasty and vertebroplasty for the treatment of painful osteoporotic compression fractures. Spine (Phila Pa 1976) 26:1511–1515. https://doi.org/10.1097/00007632-200107150-00002
Imai K (2011) Vertebral fracture risk and alendronate effects on osteoporosis assessed by a computed tomography-based nonlinear finite element method. J Bone Miner Metab 29:645–651. https://doi.org/10.1007/s00774-011-0281-9
Roux C, Baron G, Audran M, Breuil V, Chapurlat R, Cortet B, Fardellone P, Trémollières F, Ravaud P (2011) Influence of vertebral fracture assessment by dual-energy X-ray absorptiometry on decision-making in osteoporosis: a structured vignette survey. Rheumatology (Oxford) 50:2264–2269. https://doi.org/10.1093/rheumatology/ker225
Zethraeus N, Borgström F, Ström O, Kanis JA, Jönsson B (2007) Cost-effectiveness of the treatment and prevention of osteoporosis–a review of the literature and a reference model. Osteoporos Int 18:9–23. https://doi.org/10.1007/s00198-006-0257-0
Jang HD, Kim EH, Lee JC, Choi SW, Kim HS, Cha JS, Shin BJ (2022) Management of osteoporotic vertebral fracture: review update 2022. Asian Spine J 16:934–946. https://doi.org/10.31616/asj.2022.0441
Ito M, Harada A, Nakano T, Kuratsu S, Deguchi M, Sueyoshi Y, Machida M, Yonezawa Y, Matsuyama Y, Wakao N (2010) Retrospective multicenter study of surgical treatments for osteoporotic vertebral fractures. J Orthop Sci 15:289–293. https://doi.org/10.1007/s00776-010-1455-3
Libicher M, Appelt A, Berger I, Baier M, Meeder PJ, Grafe I, Dafonseca K, Nöldge G, Kasperk C (2007) The intravertebral vacuum phenomen as specific sign of osteonecrosis in vertebral compression fractures: results from a radiological and histological study. Eur Radiol 17:2248–2252. https://doi.org/10.1007/s00330-007-0684-0
Wang G, Yang H, Chen K (2010) Osteoporotic vertebral compression fractures with an intravertebral cleft treated by percutaneous balloon kyphoplasty. J Bone Joint Surg Br 92:1553–1557. https://doi.org/10.1302/0301-620x.92b11.24671
Yu CW, Hsu CY, Shih TT, Chen BB, Fu CJ (2007) Vertebral osteonecrosis: MR imaging findings and related changes on adjacent levels. AJNR Am J Neuroradiol 28:42–47
Lee HM, Park SY, Lee SH, Suh SW, Hong JY (2012) Comparative analysis of clinical outcomes in patients with osteoporotic vertebral compression fractures (OVCFs): conservative treatment versus balloon kyphoplasty. Spine J 12:998–1005. https://doi.org/10.1016/j.spinee.2012.08.024
Iwata A, Kanayama M, Oha F, Hashimoto T, Iwasaki N (2017) Does spinopelvic alignment affect the union status in thoracolumbar osteoporotic vertebral compression fracture? Eur J Orthop Surg Traumatol 27:87–92. https://doi.org/10.1007/s00590-016-1844-1
Hayashi T, Maeda T, Masuda M, Ueta T, Shiba K (2016) Morphology of the injured posterior wall causing spinal canal encroachment in osteoporotic vertebral fractures. Spine J 16:946–950. https://doi.org/10.1016/j.spinee.2016.03.021
Sugita M, Watanabe N, Mikami Y, Hase H, Kubo T (2005) Classification of vertebral compression fractures in the osteoporotic spine. J Spinal Disord Tech 18:376–381. https://doi.org/10.1097/01.bsd.0000168716.23440.61
Labelle H, Roussouly P, Berthonnaud E, Transfeldt E, O’Brien M, Chopin D, Hresko T, Dimnet J (2004) Spondylolisthesis, pelvic incidence, and spinopelvic balance: a correlation study. Spine (Phila Pa 1976) 29:2049–2054. https://doi.org/10.1097/01.brs.0000138279.53439.cc
Lee JK, Hyun SJ, Kim KJ (2022) Reciprocal changes in the whole-body following realignment surgery in adult spinal deformity. Asian Spine J 16:958–967. https://doi.org/10.31616/asj.2021.0451
Kim YC, Kim YH, Ha KY (2014) Pathomechanism of intravertebral clefts in osteoporotic compression fractures of the spine. Spine J 14:659–666. https://doi.org/10.1016/j.spinee.2013.06.106
Acknowledgements
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (No. 52019A015400438).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Hoon-Seok Sung, Sang-Il Kim, Hyung-Youl Park, Myung-Sup Ko, Jeong-Han Lee and Young-Hoon Kim (corresponding author) declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sung, HS., Kim, SI., Park, HY. et al. Predictive factors for conversion from conservatively to surgically treatment osteoporotic thoracolumbar compression fractures based on sagittal parameters and magnetic resonance imaging features. Eur Spine J 32, 3933–3940 (2023). https://doi.org/10.1007/s00586-023-07864-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07864-5