Abstract
Purpose
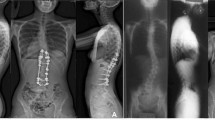
To validate the predictability of S-line in Lenke 5C patients.
Methods
Lenke 5C patients with a minimum 2-year follow-up and with the lowest instrumented vertebra (LIV) at lower end vertebra were included. The S-line was defined as a line connecting the centers of concave-side pedicles of upper instrumented vertebra (UIV) and LIV on baseline films. The S-line tilt to right was defined as positive S-line status (S-line +) and tilt to left as S-line − status. Statistical analysis was performed between different subgroups.
Results
Among the 92 patients, 69 patients had a left lumbar curve and 23 patients had a right lumbar curve. For left curves, the S-line + status had a significantly higher incidence of both proximal and distal decompensation. However, for right curves, the S-line − status was the risk factor. Thus, we modified the definition of S-line: The value of S-line tilt for right curves was opposite to that for left curves. Patients with modified S-line + showed a significantly higher incidence of both proximal and distal decompensation in Lenke 5C patients with both left and right curves (p < 0.001 and p = 0.010). In UEV group, patients with modified S-line + showed significantly higher incidence of proximal decompensation (P = 0.001). However, in UEV-1 group, the incidence of proximal decompensation was not statistically affected by modified S-line + (P = 0.281).
Conclusion
Modified S-line + is a validated risk factor that predisposed to post-operative coronal decompensation in Lenke 5C AIS patients. Selecting UIV at one level caudal to UEV could be a possible solution if the modified S-line was positive.



Similar content being viewed by others
References
Kadoury S, Cheriet F, Beauséjour M, Stokes IA, Parent S, Labelle H (2009) A three-dimensional retrospective analysis of the evolution of spinal instrumentation for the correction of adolescent idiopathic scoliosis. Eur Spine J 18(1):23–37. https://doi.org/10.1007/s00586-008-0817-4
Hattori T, Sakaura H, Iwasaki M, Nagamoto Y, Yoshikawa H, Sugamoto K (2011) In vivo three-dimensional segmental analysis of adolescent idiopathic scoliosis. Eur Spine J 20(10):1745–1750. https://doi.org/10.1007/s00586-011-1869-4
Li J, Hwang SW, Shi Z, Yan N, Yang C, Wang C, Zhu X, Hou T, Li M (2011) Analysis of radiographic parameters relevant to the lowest instrumented vertebrae and postoperative coronal balance in Lenke 5C patients. Spine 36(20):1673–1678. https://doi.org/10.1097/BRS.0b013e3182091fba
Satake K, Lenke LG, Kim YJ, Bridwell KH, Blanke KM, Sides B, Steger-May K (2005) Analysis of the lowest instrumented vertebra following anterior spinal fusion of thoracolumbar/lumbar adolescent idiopathic scoliosis: can we predict post-operative disk wedging? Spine 30(4):418–426. https://doi.org/10.1097/01.brs.0000153342.89478.d
Betz RR, Harms J, Clements DH 3rd, Lenke LG, Lowe TG, Shufflebarger HL, Jeszenszky D, Beele B (1999) Comparison of anterior and posterior instrumentation for correction of adolescent thoracic idiopathic scoliosis. Spine 24(3):225–239. https://doi.org/10.1097/00007632-199902010-00007
Li M, Ni J, Fang X, Liu H, Zhu X, He S, Gu S, Wang X (2009) Comparison of selective anterior versus posterior screw instrumentation in Lenke5C adolescent idiopathic scoliosis. Spine 34(11):1162–1166. https://doi.org/10.1097/BRS.0b013e31819e2b16
Geck MJ, Rinella A, Hawthorne D, Macagno A, Koester L, Sides B, Bridwell K, Lenke L, Shufflebarger H (2009) Comparison of surgical treatment in Lenke 5C adolescent idiopathic scoliosis: anterior dual rod versus posterior pedicle fixation surgery: a comparison of two practices. Spine 34(18):1942–1951. https://doi.org/10.1097/BRS.0b013e3181a3c777
Wang Y, Bünger CE, Zhang Y, Wu C, Li H, Dahl B, Hansen ES (2013) Lowest instrumented vertebra selection for Lenke 5C scoliosis: a minimum 2-year radiographical follow-up. Spine 38(14):E894-900. https://doi.org/10.1097/BRS.0b013e31829537be
Gomez JA, Matsumoto H, Colacchio ND, Roye DP Jr, Sucato DJ, Richards BS, Emans JB, Erickson MA, Sanders JO, Lenke LG, Vitale MG (2014) Risk factors for coronal decompensation after posterior spinal instrumentation and fusion in adolescent idiopathic scoliosis. Spine Deform 2(5):380–385. https://doi.org/10.1016/j.jspd.2014.05.001
Okada E, Watanabe K, Pang L, Ogura Y, Takahashi Y, Hosogane N, Toyama Y, Matsumoto M (2015) Posterior correction and fusion surgery using pedicle-screw constructs for Lenke type 5C adolescent idiopathic scoliosis: a preliminary report. Spine 40(1):25–30. https://doi.org/10.1097/brs.0000000000000652
Upasani VV, Hedequist DJ, Hresko MT, Karlin LI, Emans JB, Glotzbecker MP (2015) Spinal deformity progression after posterior segmental instrumentation and fusion for idiopathic scoliosis. J Child Orthop 9(1):29–37. https://doi.org/10.1007/s11832-015-0632-5
Kwan MK, Chan CY (2016) Is there an optimal upper instrumented vertebra (UIV) tilt angle to prevent post-operative shoulder imbalance and neck tilt in Lenke 1 and 2 adolescent idiopathic scoliosis (AIS) patients? Eur Spine J 25(10):3065–3074. https://doi.org/10.1007/s00586-016-4529-x
Oba H, Takahashi J, Kobayashi S, Ohba T, Ikegami S, Kuraishi S, Uehara M, Takizawa T, Munakata R, Hatakenaka T, Koseki M, Ebata S, Haro H, Matsuyama Y, Kato H (2019) Upper instrumented vertebra to the right of the lowest instrumented vertebra as a predictor of an increase in the main thoracic curve after selective posterior fusion for the thoracolumbar/lumbar curve in Lenke type 5C adolescent idiopathic scoliosis: multicenter study on the relationship between fusion area and surgical outcome. J Neurosurg Spine. https://doi.org/10.3171/2019.5.Spine181469
Lonner BS, Ren Y, Upasani VV, Marks MM, Newton PO, Samdani AF, Chen K, Shufflebarger HL, Shah SA, Lefton DR, Nasser H, Dabrowski CT, Betz RR (2018) Disc degeneration in unfused caudal motion segments ten years following surgery for adolescent idiopathic scoliosis. Spine Deform 6(6):684–690. https://doi.org/10.1016/j.jspd.2018.03.013
Wang Y, Hansen ES, Høy K, Wu C, Bünger CE (2011) Distal adding-on phenomenon in Lenke 1A scoliosis: risk factor identification and treatment strategy comparison. Spine 36(14):1113–1122. https://doi.org/10.1097/BRS.0b013e3181f51e95
Cloyd JM, Acosta FL Jr, Cloyd C, Ames CP (2010) Effects of age on perioperative complications of extensive multilevel thoracolumbar spinal fusion surgery. J Neurosurg Spine 12(4):402–408. https://doi.org/10.3171/2009.10.Spine08741
Djurasovic M, Glassman SD, Howard JM, Copay AG, Carreon LY (2011) Health-related quality of life improvements in patients undergoing lumbar spinal fusion as a revision surgery. Spine 36(4):269–276. https://doi.org/10.1097/BRS.0b013e3181cf1091
Ilharreborde B, Ferrero E, Angelliaume A, Lefèvre Y, Accadbled F, Simon AL, de Gauzy JS, Mazda K (2017) Selective versus hyperselective posterior fusions in Lenke 5 adolescent idiopathic scoliosis: comparison of radiological and clinical outcomes. Eur Spine J 26(6):1739–1747. https://doi.org/10.1007/s00586-017-5070-2
Qin X, Sun W, Xu L, Liu Z, Qiu Y, Zhu Z (2016) Selecting the last “substantially” touching vertebra as lowest instrumented vertebra in Lenke type 1A curve: radiographic outcomes with a minimum of 2-year Follow-Up. Spine 41(12):E742-750. https://doi.org/10.1097/brs.0000000000001374
Matsumoto M, Watanabe K, Hosogane N, Kawakami N, Tsuji T, Uno K, Suzuki T, Ito M, Yanagida H, Yamaguchi T, Minami S, Akazawa T (2013) Postoperative distal adding-on and related factors in Lenke type 1A curve. Spine 38(9):737–744. https://doi.org/10.1097/BRS.0b013e318279b666
Sudo H, Kaneda K, Shono Y, Iwasaki N (2016) Selection of the upper vertebra to be instrumented in the treatment of thoracolumbar and lumbar adolescent idiopathic scoliosis by anterior correction and fusion surgery using dual-rod instrumentation: a minimum 12-year follow-up study. Spine J 16(3):281–287. https://doi.org/10.1016/j.spinee.2015.08.021
Kaneda K, Satoh S, Fujiya N (1985) Analysis of results with Zielke instrumentation for thoracolumbar and lumbar curvature. Nihon Seikeigeka Gakkai Zasshi 59(8):841–851
Qin X, He Z, Yin R, Qiu Y, Zhu Z (2019) Where to stop distally in Lenke modifier C AIS with lumbar curve more than 60°: L3 or L4? Clin Neurol Neurosurg 178:77–81. https://doi.org/10.1016/j.clineuro.2019.02.005
Fabry G, Van Melkebeek J, Bockx E (1989) Back pain after Harrington rod instrumentation for idiopathic scoliosis. Spine 14(6):620–624. https://doi.org/10.1097/00007632-198906000-00015
Funding
This work was financially supported by the Natural Science Foundation of Jiangsu Province (No. BK20180122); and supported by the Special Funds for Health Science and Technology Development of Nanjing City (No. YKK18092).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has any potential conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhang, T., Shu, S., Jing, W. et al. Optimizing the fusion level for lenke 5C adolescent idiopathic scoliosis: is the S-line a validated and reproducible tool to predict coronal decompensation?. Eur Spine J 30, 1935–1942 (2021). https://doi.org/10.1007/s00586-021-06781-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-021-06781-9