Abstract
Purpose
Residual symptoms indicating incomplete remission of lower leg numbness or low back pain may occur after spine surgery. The purpose was to elucidate the pattern of residual symptoms 5 years after minimally invasive lumbar decompression surgery using a cluster analysis.
Methods
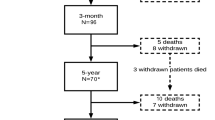
The study comprised 193 patients with lumbar spinal stenosis (LSS) (108 men, 85 women) ranging in age from 40 to 86 years (mean, 67.9 years). Each patient underwent 5-year follow-up. The Japanese Orthopedic Association score and visual analog scale scores for low back pain, leg pain, and leg numbness at 5 years were entered into the cluster analysis to characterize postoperative residual symptoms. Other clinical data were analyzed to detect the factors significantly related to each cluster.
Results
The analysis yielded four clusters representing different patterns of residual symptoms. Patients in cluster 1 (57.0%) were substantially improved and had few residual symptoms of LSS. Patients in cluster 2 (11.4%) were poorly improved and had major residual symptoms. Patients in cluster 3 (17.6%) were greatly improved but had mild residual low back pain. Patients in cluster 4 (14.0%) were improved but had severe residual leg numbness. Prognostic factors of cluster 2 were a short maximum walking distance, motor weakness, resting lower leg numbness, cofounding scoliosis, and high sagittal vertical axis.
Conclusions
This is the first study to identify specific patterns of residual symptoms of LSS after decompression surgery. Our results will contribute to acquisition of preoperative informed consent and identification of patients with the best chance of postoperative improvement.

Similar content being viewed by others
Data availability
All data analyzed during this study are included in this article.
References
Deyo RA, Mirza SK, Martin BI, Kreuter W, Goodman DC, Jarvik JG (2010) Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA 303:1259–1265
Weinstein JN, Tosteson TD, Lurie JD, Tosteson A, Blood E, Herkowitz H, Cammisa F, Albert T, Boden SD, Hilibrand A, Goldberg H, Berven S, An H (2010) Surgical versus nonoperative treatment for lumbar spinal stenosis four-year results of the spine patient outcomes research trial. Spine 35:1329–1338
Weinstein JN, Tosteson TD, Lurie JD, Tosteson AN, Blood E, Hanscom B, Herkowitz H, Cammisa F, Albert T, Boden SD, Hilibrand A, Goldberg H, Berven S, An H (2008) Surgical versus nonsurgical therapy for lumbar spinal stenosis. N Engl J Med 358:794–810
Stromqvist B, Fritzell P, Hagg O, Jonsson B, Sanden B (2013) Swespine: the Swedish spine register : the 2012 report. Eur Spine J 22:953–974
Katz JN, Lipson SJ, Brick GW, Grobler LJ, Weinstein JN, Fossel AH, Lew RA, Liang MH (1995) Clinical correlates of patient satisfaction after laminectomy for degenerative lumbar spinal stenosis. Spine (Phila Pa 1976) 20:1155–1160. https://doi.org/10.1097/00007632-199505150-00008
Airaksinen O, Herno A, Turunen V, Saari T, Suomlainen O (1997) Surgical outcome of 438 patients treated surgically for lumbar spinal stenosis. Spine (Phila Pa 1976) 22:2278–2282. https://doi.org/10.1097/00007632-199710010-00016
Bouras T, Stranjalis G, Loufardaki M, Sourtzis I, Stavrinou LC, Sakas DE (2010) Predictors of long-term outcome in an elderly group after laminectomy for lumbar stenosis. J Neurosurg Spine 13:329–334. https://doi.org/10.3171/2010.3.SPINE09487
Paulsen RT, Bouknaitir JB, Fruensgaard S, Carreon L, Andersen M (2018) Prognostic factors for satisfaction after decompression surgery for lumbar spinal stenosis. Neurosurgery 82:645–651
Slatis P, Malmivaara A, Heliovaara M, Sainio P, Herno A, Kankare J, Seitsalo S, Tallroth K, Turunen V, Knekt P, Hurri H (2011) Long-term results of surgery for lumbar spinal stenosis: a randomised controlled trial. Eur Spine J 20:1174–1181
Lurie JD, Tosteson TD, Tosteson A, Abdu WA, Zhao W, Morgan TS, Weinstein JN (2015) Long-term outcomes of lumbar spinal stenosis: eight-year results of the Spine Patient Outcomes Research Trial (SPORT). Spine 40:63–76
Dunn KM, Jordan K, Croft PR (2006) Characterizing the course of low back pain: a latent class analysis. Am J Epidemiol 163:754–761
Weatherall M, Shirtcliffe P, Travers J, Beasley R (2010) Use of cluster analysis to define COPD phenotypes. Eur Respir J 36:472–474
Toyoda H, Takahashi S, Hoshino M, Takayama K, Iseki K, Sasaoka R, Tsujio T, Yasuda H, Sasaki T, Kanematsu F, Kono H, Nakamura H (2017) Characterizing the course of back pain after osteoporotic vertebral fracture: a hierarchical cluster analysis of a prospective cohort study. Arch Osteoporos 12:82
Toyoda H, Nakamura H, Konishi S, Dohzono S, Kato M, Matsuda H (2011) Clinical outcome of microsurgical bilateral decompression via unilateral approach for lumbar canal stenosis: minimum five-year follow-up. Spine 36:410–415
Dohzono S, Toyoda H, Matsumoto T, Suzuki A, Terai H, Nakamura H (2015) The influence of preoperative spinal sagittal balance on clinical outcomes after microendoscopic laminotomy in patients with lumbar spinal canal stenosis. J Neurosurg 23:49–54
Hirabayashi K, Miyakawa J, Satomi K, Maruyama T, Wakano K (1981) Operative results and postoperative progression of ossification among patients with ossification of cervical posterior longitudinal ligament. Spine 6:354–364
Parker SL, Adogwa O, Paul AR, Anderson WN, Aaronson O, Cheng JS, McGirt MJ (2011) Utility of minimum clinically important difference in assessing pain, disability, and health state after transforaminal lumbar interbody fusion for degenerative lumbar spondylolisthesis. J Neurosurg 14:598–604
Alashwal H, El Halaby M, Crouse JJ, Abdalla A, Moustafa AA (2019) The application of unsupervised clustering methods to alzheimer’s disease. Front Comput Neurosci 13:31. https://doi.org/10.3389/fncom.2019.00031
Ward JH Jr (1963) Hierarchical grouping to optimize an objective function. J Am Stat Assoc 58:236–244
Murtagh F, Legendre P (2014) Ward’s hierarchical agglomerative clustering method: which algorithms implement ward’s criterion? J Classif 31:274–295
Carragee EJ (2010) The increasing morbidity of elective spinal stenosis surgery: is it necessary? JAMA 303:1309–1310. https://doi.org/10.1001/jama.2010.402
Minamide A, Yoshida M, Yamada H, Nakagawa Y, Hashizume H, Iwasaki H, Tsutsui S (2015) Clinical outcomes after microendoscopic laminotomy for lumbar spinal stenosis: a 5-year follow-up study. Eur Spine J 24:396–403. https://doi.org/10.1007/s00586-014-3599-x
Dohzono S, Toyoda H, Takahashi S, Matsumoto T, Suzuki A, Terai H, Nakamura H (2016) Factors associated with improvement in sagittal spinal alignment after microendoscopic laminotomy in patients with lumbar spinal canal stenosis. J Neurosurg Spine 25:39–45. https://doi.org/10.3171/2015.12.SPINE15805
Machado GC, Ferreira PH, Harris IA, Pinheiro MB, Koes BW, van Tulder M, Rzewuska M, Maher CG, Ferreira ML (2015) Effectiveness of surgery for lumbar spinal stenosis: a systematic review and meta-analysis. PLoS ONE 10:e0122800. https://doi.org/10.1371/journal.pone.0122800
Fritsch CG, Ferreira ML, Maher CG, Herbert RD, Pinto RZ, Koes B, Ferreira PH (2017) The clinical course of pain and disability following surgery for spinal stenosis: a systematic review and meta-analysis of cohort studies. Eur Spine J 26:324–335. https://doi.org/10.1007/s00586-016-4668-0
Sigmundsson FG, Kang XP, Jönsson B, Strömqvist B (2012) Prognostic factors in lumbar spinal stenosis surgery. Acta Orthop 83:536–542. https://doi.org/10.3109/17453674.2012.733915
Aono H, Iwasaki M, Ohwada T, Okuda S, Hosono N, Fuji T, Yoshikawa H (2007) Surgical outcome of drop foot caused by degenerative lumbar diseases. Spine (Phila Pa 1976) 32:E262-266. https://doi.org/10.1097/01.brs.0000259922.82413.72
Hara N, Oka H, Yamazaki T, Takeshita K, Murakami M, Hoshi K, Terayama S, Seichi A, Nakamura K, Kawaguchi H, Matsudaira K (2010) Predictors of residual symptoms in lower extremities after decompression surgery on lumbar spinal stenosis. Eur Spine J 19:1849–1854. https://doi.org/10.1007/s00586-010-1374-1
Pearson A, Lurie J, Tosteson T, Zhao W, Abdu W, Weinstein JN (2012) Who should have surgery for spinal stenosis? treatment effect predictors in SPORT. Spine (Phila Pa 1976) 37:1791–1802. https://doi.org/10.1097/BRS.0b013e3182634b04
Liu K, Zhu W, Shi J, Jia L, Shi G, Wang Y, Liu N (2013) Foot drop caused by lumbar degenerative disease: clinical features, prognostic factors of surgical outcome and clinical stage. PLoS ONE 8:e80375. https://doi.org/10.1371/journal.pone.0080375
Goh KJ, Khalifa W, Anslow P, Cadoux-Hudson T, Donaghy M (2004) The clinical syndrome associated with lumbar spinal stenosis. Eur Neurol 52:242–249. https://doi.org/10.1159/000082369
Babb A, Carlson WO (2006) Spinal stenosis. S D Med 59:103–105
Hikata T, Watanabe K, Fujita N, Iwanami A, Hosogane N, Ishii K, Nakamura M, Toyama Y, Matsumoto M (2015) Impact of sagittal spinopelvic alignment on clinical outcomes after decompression surgery for lumbar spinal canal stenosis without coronal imbalance. J Neurosurg Spine 23:451–458. https://doi.org/10.3171/2015.1.SPINE14642
Minamide A, Yoshida M, Iwahashi H, Simpson AK, Yamada H, Hashizume H, Nakagawa Y, Iwasaki H, Tsutsui S, Kagotani R, Sonekatsu M, Sasaki T, Shinto K, Deguchi T (2017) Minimally invasive decompression surgery for lumbar spinal stenosis with degenerative scoliosis: predictive factors of radiographic and clinical outcomes. J Orthop Sci 22:377–383. https://doi.org/10.1016/j.jos.2016.12.022
Kato M, Namikawa T, Matsumura A, Konishi S, Nakamura H (2017) Radiographic risk factors of reoperation following minimally invasive decompression for lumbar canal stenosis associated with degenerative scoliosis and spondylolisthesis. Global Spine J 7:498–505. https://doi.org/10.1177/2192568217699192
Ogura Y, Shinozaki Y, Kobayashi Y, Kitagawa T, Yonezawa Y, Takahashi Y, Yoshida K, Yasuda A, Ogawa J (2019) Impact of sagittal spinopelvic alignment on clinical outcomes and health-related quality of life after decompression surgery without fusion for lumbar spinal stenosis. J Neurosurg Spine. https://doi.org/10.3171/2018.10.SPINE181094
Aalto TJ, Malmivaara A, Kovacs F, Herno A, Alen M, Salmi L, Kröger H, Andrade J, Jiménez R, Tapaninaho A, Turunen V, Savolainen S, Airaksinen O (2006) Preoperative predictors for postoperative clinical outcome in lumbar spinal stenosis: systematic review. Spine (Phila Pa 1976) 31:E648-663. https://doi.org/10.1097/01.brs.0000231727.88477.da
Ghahreman A, Ferch RD, Rao P, Chandran N, Shadbolt B (2009) Recovery of ankle dorsiflexion weakness following lumbar decompressive surgery. J Clin Neurosci 16:1024–1027. https://doi.org/10.1016/j.jocn.2008.10.017
Iizuka Y, Iizuka H, Tsutsumi S, Nakagawa Y, Nakajima T, Sorimachi Y, Ara T, Nishinome M, Seki T, Shida K, Takagishi K (2009) Foot drop due to lumbar degenerative conditions: mechanism and prognostic factors in herniated nucleus pulposus and lumbar spinal stenosis. J Neurosurg Spine 10:260–264. https://doi.org/10.3171/2008.12.SPINE08500
Lin Z, Zhao C, Luo Q, Xia X, Yu X, Huang F (2016) Prevalence of restless legs syndrome in chronic kidney disease: a systematic review and meta-analysis of observational studies. Ren Fail 38:1335–1346. https://doi.org/10.1080/0886022X.2016.1227564
Försth P, Ólafsson G, Carlsson T, Frost A, Borgström F, Fritzell P, Öhagen P, Michaëlsson K, Sandén B (2016) A randomized, controlled trial of fusion surgery for lumbar spinal stenosis. N Engl J Med 374:1413–1423. https://doi.org/10.1056/NEJMoa1513721
Dijkerman ML, Overdevest GM, Moojen WA, Vleggeert-Lankamp CLA (2018) Decompression with or without concomitant fusion in lumbar stenosis due to degenerative spondylolisthesis: a systematic review. Eur Spine J 27:1629–1643. https://doi.org/10.1007/s00586-017-5436-5
Kim CH, Chung CK, Choi Y, Kim MJ, Shin S, Yang SH, Hwang SH, Kim DH, Park SB, Lee JH (2019) Increased proportion of fusion surgery for degenerative lumbar spondylolisthesis and changes in reoperation rate: a nationwide cohort study with a minimum 5-year follow-up. Spine (Phila Pa 1976) 44:346–354. https://doi.org/10.1097/BRS.0000000000002805
Acknowledgements
We would like to thank the patients, who participated in this study. We thank Angela Morben, DVM, ELS, from Edanz Group (https://en-author-services.edanzgroup.com/), for editing a draft of this manuscript.
Author information
Authors and Affiliations
Contributions
HT, KY and HN contributed to the study concept and design. HT, MH, HT, AS, KY and ST contributed to data acquisition and analyses. HT, KT, SO, YH, AY and HS contributed to data interpretation. All authors have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Consent to participate
Each participant provided an informed consent for participation.
Consent to publish
Each participant provided an informed consent for publication.
Ethical approval
Ethics approval was provided by the local ethics committee of Osaka City University (approval no. 3170).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Toyoda, H., Yamada, K., Terai, H. et al. Classification and prognostic factors of residual symptoms after minimally invasive lumbar decompression surgery using a cluster analysis: a 5-year follow-up cohort study. Eur Spine J 30, 918–927 (2021). https://doi.org/10.1007/s00586-021-06754-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-021-06754-y