Abstract
Background
Laparoscopic fundoplication is the current gold standard for medically refractory gastroesophageal reflux disease. Over a 10-year period following surgery, 5–10% of primary laparoscopic fundoplication patients undergo reoperative surgery. Our objective was to compare the symptomatic outcomes and morbidity of primary and reoperative fundoplication procedures.
Methods
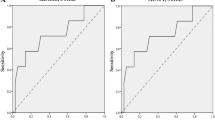
This was a retrospective review of patients who underwent laparoscopic primary or reoperative fundoplication between 2011 and 2017. A single surgeon with a more than 10-year experience in reoperative foregut surgery performed all procedures. Patients in both groups completed the GERD health-related quality of life (GERD-HRQL) survey prior to surgery and postoperatively. Outcomes were reflected by the composite GERD-HRQL scores (0 to 50, with lower scores representing a better GERD-related quality of life), which were compared between groups postoperatively. Demographics, perioperative data, and complications were compared. Patient data were analyzed using Chi-Square tests and outcomes were analyzed using independent samples t tests and Mann–Whitney U tests.
Results
There were 136 primary and 82 reoperative fundoplications. Prior to surgery, GERD-HRQL scores were similar for primary and reoperative patients. Both groups experienced significant improvement in GERD-related quality of life at 2 years, although this improvement was greater in primary patients (8.7 ± 7.8 primary vs. 14.3 ± 13.6 reoperative, p = 0.02). Operative time and length of stay were longer following reoperative cases. The rate of moderate to severe 30-day complications requiring radiologic, endoscopic, or surgical intervention was similar (2.9% primary vs. 1.2% reoperative, p = 0.65).
Conclusions
Patients who undergo reoperative fundoplication experience a significant improvement in their GERD-related symptoms, although not to the degree seen in primary antireflux surgery patients. Perioperative morbidity rates following reoperative and primary procedures can be similar in the hands of an experienced surgeon.
Similar content being viewed by others
References
El-Serag HB, Sweet S, Winchester CC, Dent J (2014) Update on the epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut 63:871–880
Grant A, Boachie C, Cotton S, Faria R, Bojke L, Epstein DM, Ramsay CR, Corbacho B, Sculpher M, Krukowski ZH, Heading RC, Campbell MK (2013) Clinical and economic evaluation of laparoscopic surgery compared with medical management for gastro-oesophageal reflux disease: 5-year follow-up of multicentre randomised trial (the REFLUX trial). Health Technol Assess 17:1–167
Stefanidis D, Hope WW, Kohn GP, Reardon PR, Richardson WS, Fanelli RD, SAGES Guidelines Committee (2010) Guidelines for surgical treatment of gastroesophageal reflux disease. Surg Endosc 24:2647–2669. https://doi.org/10.1007/s00464-010-1267-8
Teixeira JR, Moreira LM, Flores A, Ribeiro C (2012) Durability of long-term results of laparoscopic nissen—comparison of the results at 5 years and 10 years after surgery. Hepatogastroenterology 59:2428–2431
Fein M, Bueter M, Thalheimer A, Pachmayr V, Heimbucher J, Freys SM, Fuchs KH (2008) Ten-year outcome of laparoscopic antireflux surgery. J Gastrointest Surg 12:1893–1899
Zhou T, Harnsberger C, Broderick R, Fuchs H, Talamini M, Jacobsen G, Horgan S, Chang D, Sandler B (2015) Reoperation rates after laparoscopic fundoplication. Surg Endosc 29:510–514
Wilshire CL, Louie BE, Schultz D, Jutric Z, Farivar AS, Aye RS (2016) Clinical outcomes of reoperation for failed antireflux operations. Ann Thorac Surg 101:1290–1296
Musunuru S, Gould J (2012) Perioperative outcomes of surgical procedures for symptomatic fundoplication failure: a retrospective case-control study. Surg Endosc 26:838–842
Dindo D, Demartines N, Clavien P (2004) Classification of surgical complications. Ann Surg 240:205–213
Velanovich V (2007) The development of the GERD-HRQL symptom severity instrument. Dis Esoph 20:130–134
Chey WD, Mody RR, Wu EQ, Chen L, Kothari S, Persson B, Beaulieu N, Lu M (2009) Treatment patterns and symptom control in patients with GERD: US community-based survey. Curr Med Res Opin 25:1869–1878. https://doi.org/10.1185/03007990903035745
Funk LM, Kanji A, Scott Melvin W, Perry KA (2014) Elective antireflux surgery in the US: an analysis of national trends in utilization and inpatient outcomes from 2005 to 2010. Surg Endosc 28:1712–1719. https://doi.org/10.1007/s00464-013-3380-y
Obeid N, Altieri M, Yang J, Park J, Price K, Bates A, Pryor AD (2018) Patterns of reoperation after failed fundoplication: an analysis of 9462 patients. Surg Endosc 32:345–350. https://doi.org/10.1007/s00464-017-5682-y
Van Beek DB, Auyang ED, Soper NJ (2011) A comprehensive review of laparoscopic redo fundoplication. Surg Endosc 25:706–712
Furnée EJ, Draaisma WA, Broeders IA, Gooszen HG (2009) Surgical reintervention after failed antireflux surgery: a systematic review of the literature. J Gastrointest Surg 13:1539–1549. https://doi.org/10.1007/s11605-009-0873-z
Singhal S, Kirkpatrick DR, Masuda T, Gerhardt J, Mittal SK (2018) Primary and redo antireflux surgery: outcomes and lessons learned. J Gastrointest Surg 22:177–186. https://doi.org/10.1007/s11605-017-3480-4
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Gould is a consultant for Torax Medical/Ethicon and Gore. Mr. Kanani have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kanani, Z., Gould, J.C. Laparoscopic fundoplication for refractory GERD: a procedure worth repeating if needed. Surg Endosc 35, 298–302 (2021). https://doi.org/10.1007/s00464-020-07396-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07396-9