Abstract
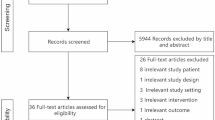
Critically ill patients who require a tracheostomy often have dysphagia. Widespread practice guidelines have yet to be developed regarding the acute assessment and management of dysphagia in patients with tracheostomy. In order for clinicians to base their practice on the best available evidence, they must first assess the applicable literature and determine its quality. To inform guideline development, our objective was to assess literature quality concerning swallowing following tracheostomy in acute stages of critical illness in adults. Our systematic literature search (published previously) included eight databases, nine gray literature repositories and citation chasing. Using inclusion criteria determined a priori, two reviewers, blinded to each other, conducted an eligibility review of identified citations. Patients with chronic tracheostomy and etiologies including head and/or neck cancer diagnoses were excluded. Four teams of two reviewers each, blinded to each other, assessed quality of included studies using a modified Cochrane Risk of Bias tool (RoB). Disagreements were resolved by consensus. Data were summarized descriptively according to study design and RoB domain. Of 6,396 identified citations, 74 studies met our inclusion criteria. Of those, 71 were observational and three were randomized controlled trials. Across all studies, the majority (> 75%) had low bias risk with: participant blinding, outcome reporting, and operationally defined outcomes. Areas requiring improvement included assessor and study personnel blinding. Prior to translating the literature into practice guidelines, we recommend attention to study quality limitations and its potential impact on study outcomes. For future work, we suggest an iterative approach to knowledge translation.



Similar content being viewed by others
References
Esteban A, Anzueto A, Frutos F, Alia I, Brochard L, Stewart TE, Benito S, Epstein SK, Apezteguia C, Nightingale P, Arroliga AC, Tobin MJ. Characteristics and outcomes in adult patients receiving mechanical ventilation: a 28-day international study. JAMA. 2002;287(3):345–55.
Durbin CG Jr. Indications for and timing of tracheostomy. Respir Care. 2005;50(4):483–7.
Freeman-Sanderson AL, Togher L, Elkins MR, Phipps PR. Quality of life improves with return of voice in tracheostomy patients in intensive care: an observational study. J Crit Care. 2016;33:186–91.
Skoretz SA, Riopelle SJ, Wellman L, Dawson C. Investigating swallowing and tracheostomy following critical illness: a scoping review. Crit Care Med. 2020;48(2):e141–e151.
RCSLT position paper: Speech and language therapy in adult critical care. 2014, The Royal College of Speech and Language Therapists: London, UK. pp. 1–25.
Moher D, Schulz KF, Simera I, Altman DG. Guidance for developers of health research reporting guidelines. PLoS Med. 2010;7(2):e1000217.
Sackett DL. Evidence-based medicine. Semin Perinatol. 1997;21(1):3–5.
van der Laan AL, Boenink M. Beyond bench and bedside: disentangling the concept of translational research. Health Care Anal. 2015;23(1):32–49.
Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (2019) Cochrane handbook for systematic reviews of interventions. Cochrane version 6.0 (updated July 2019): www.training.cochrane.org/handbook.
Pannucci CJ, Wilkins EG. Identifying and avoiding bias in research. Plast Reconstr Surg. 2010;126(2):619–25.
Amathieu R, Sauvat S, Reynaud P, Slavov V, Luis D, Dinca A, Tual L, Bloc S, Dhonneur G. Influence of the cuff pressure on the swallowing reflex in tracheostomized intensive care unit patients. Br J Anaesth. 2012;109(4):578–83.
Bonanno PC. Swallowing dysfunction after tracheostomy. Ann Surg. 1971;174(1):29–33.
Ceriana P, Carlucci A, Schreiber A, Fracchia C, Cazzani C, Dichiarante M, Cattani B, Fassio C, Segagni D, Nava S. Changes of swallowing function after tracheostomy: a videofluoroscopy study. Minerva Anestesiol. 2014;81(4):389–97.
Brady SL, Darragh M, Escobar NG, O'Neil K, Pape TL, Rao N. Persons with disorders of consciousness: are oral feedings safe/effective? Brain Inj. 2006;20(13–14):1329–34.
Coelho CA. Preliminary findings on the nature of dysphagia in patients with chronic obstructive pulmonary disease. Dysphagia. 1987;2(1):28–31.
Daly E, Miles A, Scott S, Gillham M. Finding the red flags: swallowing difficulties after cardiac surgery in patients with prolonged intubation. J Crit Care. 2016;31(1):119–24.
Davis DG, Bears S, Barone JE, Corvo PR, Tucker JB. Swallowing with a tracheostomy tube in place: does cuff inflation matter? J Intensive Care Med. 2002;17(3):132–5.
Davis LA, Stanton ST. Characteristics of dysphagia in elderly patients requiring mechanical ventilation. Dysphagia. 2004;19(1):7–14.
DeVita MA, Spierer-Rundback L. Swallowing disorders in patients with prolonged orotracheal intubation or tracheostomy tubes. Crit Care Med. 1990;18(12):1328–30.
Donzelli J, Brady S, Wesling M, Craney M. Predictive value of accumulated oropharyngeal secretions for aspiration during video nasal endoscopic evaluation of the swallow. Ann Otol Rhinol Laryngol. 2003;112(5):469–75.
Donzelli J, Brady S, Wesling M, Theisen M. Effects of the removal of the tracheotomy tube on swallowing during the fiberoptic endoscopic exam of the swallow (FEES). Dysphagia. 2005;20(4):283–9.
Donzelli J, Brady S, Wesling M, Theisen M. Secretions, occlusion status, and swallowing in patients with a tracheotomy tube: a descriptive study. Ear Nose Throat J. 2006;85(12):831–4.
DuBose CM, Groher MG, Mann GC, Mozingo DW. Pattern of dysphagia recovery after thermal burn injury. J Burn Care Rehabil. 2005;26(3):233–7.
Elpern EH, Borkgren Okonek M, Bacon M, Gerstung C, Skrzynski M. Effect of the Passy-Muir tracheostomy speaking valve on pulmonary aspiration in adults. Heart Lung. 2000;29(4):287–93.
Elpern EH, Jacobs ER, Bone RC. Incidence of aspiration in tracheally intubated adults. Heart Lung. 1987;16(5):527–31.
Elpern EH, Scott MG, Petro L, Ries MH. Pulmonary aspiration in mechanically ventilated patients with tracheostomies. Chest. 1994;105(2):563–6.
Fiorelli A, Ferraro F, Nagar F, Fusco P, Mazzone S, Costa G, Di Natale D, Serra N, Santini M. A new modified evans blue dye test as screening test for aspiration in tracheostomized patients. J Cardiothorac Vasc Anesth. 2016;31(2):441–5.
Frank U, Mader M, Sticher H. Dysphagic patients with tracheotomies: a multidisciplinary approach to treatment and decannulation management. Dysphagia. 2007;22(1):20–9.
Hafner G, Neuhuber A, Hirtenfelder S, Schmedler B, Eckel HE. Fiberoptic endoscopic evaluation of swallowing in intensive care unit patients. Eur Arch Otorhinolaryngol. 2008;265(4):441–6.
Hales PA, Drinnan MJ, Wilson JA. The added value of fibreoptic endoscopic evaluation of swallowing in tracheostomy weaning. Clin Otolaryngol. 2008;33(4):319–24.
Hayashi T, Fujiwara Y, Sakai H, Maeda T, Ueta T, Shiba K. Risk factors for severe dysphagia in acute cervical spinal cord injury. Spinal Cord. 2017;55(10):940–3.
Hogue CW Jr, Lappas GD, Creswell LL, Ferguson TB Jr, Sample M, Pugh D, Balfe D, Cox JL, Lappas DG. Swallowing dysfunction after cardiac operations. Associated adverse outcomes and risk factors including intraoperative transesophageal echocardiography. J Thorac Cardiovasc Surg. 1995;110(2):517–22.
Kang JY, Choi KH, Yun GJ, Kim MY, Ryu JS. Does removal of tracheostomy affect dysphagia? A kinematic analysis. Dysphagia. 2012;27(4):498–503.
Kim YK, Choi JH, Yoon JG, Lee JW, Cho SS. Improved dysphagia after decannulation of tracheostomy in patients with brain injuries. Ann Rehabil Med. 2015;39(5):778–85.
Kothari M, Bjerrum K, Nielsen LH, Jensen J, Nielsen JF. Influence of external subglottic air flow on dysphagic tracheotomized patients with severe brain injury. Ann Otol Rhinol Laryngol. 2017;126(3):199–204.
Leder SB. Effect of a one-way tracheotomy speaking valve on the incidence of aspiration in previously aspirating patients with tracheotomy. Dysphagia. 1999;14(2):73–7.
Leder SB. Incidence and type of aspiration in acute care patients requiring mechanical ventilation via a new tracheotomy. Chest. 2002;122(5):1721–6.
Leder SB, Joe JK, Hill SE, Traube M. Effect of tracheotomy tube occlusion on upper esophageal sphincter and pharyngeal pressures in aspirating and nonaspirating patients. Dysphagia. 2001;16(2):79–82.
Leder SB, Ross DA. Investigation of the causal relationship between tracheotomy and aspiration in the acute care setting. Laryngoscope. 2000;110(4):641–4.
Leder SB, Ross DA. Confirmation of no causal relationship between tracheotomy and aspiration status: a direct replication study. Dysphagia. 2010;25(1):35–9.
Leder SB, Tarro JM, Burrell MI. Effect of occlusion of a tracheotomy tube on aspiration. Dysphagia. 1996;11(4):254–8.
Ledl C, Ullrich YY. Occlusion of tracheostomy tubes does not alter pharyngeal phase kinematics but reduces penetration by enhancing pharyngeal clearance: a prospective study in patients with neurogenic dysphagia. Am J Phys Med Rehabil. 2017;96(4):268–72.
Lee JC, Gross BW, Rittenhouse KJ, Vogel AR, Vellucci A, Alzate J, Gillio M, Rogers FB. A bitter pill to swallow: dysphagia in cervical spine injury. J Surg Res. 2016;201(2):388–93.
Macht M, King CJ, Wimbish T, Clark BJ, Benson AB, Burnham EL, Williams A, Moss M. Post-extubation dysphagia is associated with longer hospitalization in survivors of critical illness with neurologic impairment. Crit Care. 2013;17(3):R119.
Macht M, Wimbish T, Clark BJ, Benson AB, Burnham EL, Williams A, Moss M. Postextubation dysphagia is persistent and associated with poor outcomes in survivors of critical illness. Crit Care. 2011;15(5):R231.
Mah JW, Staff I, Fisher SR, Butler KL. Improving decannulation and swallowing function: a comprehensive, multidisciplinary approach to post-tracheostomy care. Respir Care. 2017;62(2):137–43.
Mandaville A, Ray A, Robertson H, Foster C, Jesser C. A retrospective review of swallow dysfunction in patients with severe traumatic brain injury. Dysphagia. 2014;29(3):310–8.
Mangilli LD, Sassi FC, de Medeiros GC, de Andrade CR. Rehabilitative management of swallowing and oral-motor movements in patients with tetanus of a public service in Brazil. Acta Trop. 2012;122(3):241–6.
O'Neil-Pirozzi TM, Lisiecki DJ, Jack Momose K, Connors JJ, Milliner MP. Simultaneous modified barium swallow and blue dye tests: a determination of the accuracy of blue dye test aspiration findings. Dysphagia. 2003;18(1):32–8.
O'Neil-Pirozzi TM, Momose KJ, Mello J, Lepak P, McCabe M, Connors JJ, Lisiecki DJ. Feasibility of swallowing interventions for tracheostomized individuals with severely disordered consciousness following traumatic brain injury. Brain Inj. 2003;17(5):389–99.
Peruzzi WT, Logemann JA, Currie D, Moen SG. Assessment of aspiration in patients with tracheostomies: comparison of the bedside colored dye assessment with videofluoroscopic examination. Respir Care. 2001;46(3):243–7.
Ponfick M, Linden R, Nowak DA. Dysphagia—a common, transient symptom in critical illness polyneuropathy: a fiberoptic endoscopic evaluation of swallowing study. Crit Care Med. 2015;43(2):365–72.
Romero CM, Marambio A, Larrondo J, Walker K, Lira MT, Tobar E, Cornejo R, Ruiz M. Swallowing dysfunction in nonneurologic critically ill patients who require percutaneous dilatational tracheostomy. Chest. 2010;137(6):1278–82.
Schonhofer B, Barchfeld T, Haidl P, Kohler D. Scintigraphy for evaluating early aspiration after oral feeding in patients receiving prolonged ventilation via tracheostomy. Intensive Care Med. 1999;25(3):311–4.
Seidl RO, Nusser-Muller-Busch R, Ernst A. The influence of tracheotomy tubes on the swallowing frequency in neurogenic dysphagia. Otolaryngol Head Neck Surg. 2005;132(3):484–6.
Seidl RO, Nusser-Muller-Busch R, Kurzweil M, Niedeggen A. Dysphagia in acute tetraplegics: a retrospective study. Spinal Cord. 2010;48(3):197–201.
Seo HG, Kim JG, Nam HS, Lee WH, Han TR, Oh BM. Swallowing function and kinematics in stroke patients with tracheostomies. Dysphagia. 2017;32(3):393–400.
Sharma OP, Oswanski MF, Singer D, Buckley B, Courtright B, Raj SS, Waite PJ, Tatchell T, Gandaio A. Swallowing disorders in trauma patients: impact of tracheostomy. Am Surg. 2007;73(11):1117–21.
Shem K, Castillo K, Wong SL, Chang J, Kolakowsky-Hayner S. Dysphagia and respiratory care in individuals with tetraplegia: incidence, associated factors, and preventable complications. Top Spinal Cord Inj Rehabil. 2012;18(1):15–22.
Shin JC, Yoo JH, Lee YS, Goo HR, Kim DH. Dysphagia in cervical spinal cord injury. Spinal Cord. 2011;49(9):1008–13.
Simao Mde A, Alacid CA, Rodrigues KA, Albuquerque C, Furkim AM. Incidence of tracheal aspiration in tracheotomized patients in use of mechanical ventilation. Arq Gastroenterol. 2009;46(4):311–4.
Suiter DM, McCullough GH, Powell PW. Effects of cuff deflation and one-way tracheostomy speaking valve placement on swallow physiology. Dysphagia. 2003;18(4):284–92.
Suntrup S, Marian T, Schroder JB, Suttrup I, Muhle P, Oelenberg S, Hamacher C, Minnerup J, Warnecke T, Dziewas R. Electrical pharyngeal stimulation for dysphagia treatment in tracheotomized stroke patients: a randomized controlled trial. Intensive Care Med. 2015;41(9):1629–37.
Tolep K, Getch CL, Criner GJ. Swallowing dysfunction in patients receiving prolonged mechanical ventilation. Chest. 1996;109(1):167–72.
Ueha R, Nito T, Sakamoto T, Yamauchi A, Tsunoda K, Yamasoba T. Post-operative swallowing in multiple system atrophy. Eur J Neurol. 2016;23(2):393–400.
Warnecke T, Suntrup S, Teismann IK, Hamacher C, Oelenberg S, Dziewas R. Standardized endoscopic swallowing evaluation for tracheostomy decannulation in critically ill neurologic patients. Crit Care Med. 2013;41(7):1728–32.
Zielske J, Bohne S, Brunkhorst FM, Axer H, Guntinas-Lichius O. Acute and long-term dysphagia in critically ill patients with severe sepsis: results of a prospective controlled observational study. Eur Arch Otorhinolaryngol. 2014;271(11):3085–93.
Starmer HM, Riley LHI, Hillel AT, Akst LM, Best SR, Gourin CG. Dysphagia, short-term outcomes, and cost of care after anterior cervical disc surgery. Dysphagia. 2014;29(1):68–77.
Clayton N, Kennedy P, Maitz P. The severe burns patient with tracheostomy: implications for management of dysphagia, dysphonia and laryngotracheal pathology. Burns. 2010;36(6):850–5.
Smailes ST, Ives M, Richardson P, Martin RV, Dziewulski P. Percutaneous dilational and surgical tracheostomy in burn patients: incidence of complications and dysphagia. Burns. 2014;40(3):436–42.
Sutt AL, Cornwell P, Mullany D, Kinneally T, Fraser JF. The use of tracheostomy speaking valves in mechanically ventilated patients results in improved communication and does not prolong ventilation time in cardiothoracic intensive care unit patients. J Crit Care. 2015;30(3):491–4.
Wakabayashi H, Takahashi R, Watanabe N, Oritsu H, Shimizu Y. Prevalence of skeletal muscle mass loss and its association with swallowing function after cardiovascular surgery. Nutrition. 2017;38:70–3.
Hernandez G, Ortiz R, Pedrosa A, Cuena R, Vaquero Collado C, Gonzalez Arenas P, Garcia Plaza S, Canabal Berlanga A, Fernandez R. The indication of tracheotomy conditions the predictors of time to decannulation in critical patients. Med Intensiva. 2012;36(8):531–9.
Pryor L, Ward E, Cornwell P, O'Connor S, Chapman M. Patterns of return to oral intake and decannulation post-tracheostomy across clinical populations in an acute inpatient setting. Int J Lang Commun Disord. 2016;51(5):556–67.
Ward BK, Francis HW, Best SR, Starmer HM, Akst LM, Gourin CG. National prevalence and impact of perioperative vagus nerve injury in vestibular schwannoma. Laryngoscope. 2012;122(12):2824–31.
Beltrame F, Zussino M, Martinez B, Dibartolomeo S, Saltarini M, Vetrugno L, Giordano F. Percutaneous versus surgical bedside tracheostomy in the intensive care unit: a cohort study. Minerva Anestesiol. 2008;74(10):529–35.
Diaz-Reganon G, Minambres E, Ruiz A, Gonzalez-Herrera S, Holanda-Pena M, Lopez-Espadas F. Safety and complications of percutaneous tracheostomy in a cohort of 800 mixed ICU patients. Anaesthesia. 2008;63(11):1198–203.
Freeman-Sanderson AL, Togher L, Elkins MR, Phipps PR. Return of voice for ventilated tracheostomy patients in ICU: a randomized controlled trial of early-targeted intervention. Crit Care Med. 2016;44(6):1075–81.
Hernandez G, Pedrosa A, Ortiz R, Cruz Accuaroni Mdel M, Cuena R, Vaquero Collado C, Garcia Plaza S, Gonzalez Arenas P, Fernandez R. The effects of increasing effective airway diameter on weaning from mechanical ventilation in tracheostomized patients: a randomized controlled trial. Intensive Care Med. 2013;39(6):1063–70.
Young PJ, Pakeerathan S, Blunt MC, Subramanya S. A low-volume, low-pressure tracheal tube cuff reduces pulmonary aspiration. Crit Care Med. 2006;34(3):632–9.
Guell MR, Avendano M, Fraser J, Goldstein R. Pulmonary and nonpulmonary alterations in Duchenne muscular dystrophy. Arch Bronconeumol. 2007;43(10):557–61.
Woo P, Kelly G, Kirshner P. Airway complications in the head injured. Laryngoscope. 1989;99(7 Pt 1):725–31.
Yoshida M, Ikeda J, Urikane Y, Kashiwada T, Kaseda Y, Kohriyama T. Prevalence of tracheotomy and percutaneous endoscopic gastrostomy in patients with Guillain-Barre syndrome. Dysphagia. 2017;32(2):236–40.
Conway DH, Mackie C. The effects of tracheostomy cuff deflation during continuous positive airway pressure. Anaesthesia. 2004;59(7):652–7.
Concato J, Shah N, Horwitz RI. Randomized, controlled trials, observational studies, and the hierarchy of research designs. N Engl J Med. 2000;342(25):1887–922.
Rosenbek JC. Tyranny of the randomised clinical trial. Int J Speech Lang Pathol. 2016;18(3):241–9.
Brodsky MB, Richard T, Greco E, Jedlanek E, McCoy Y, Mckeon G, Sherman V, Martino R, The first 30 years of research in dysphagia: a scoping review. Dysphagia. 2019;34(6):963.
Acknowledgements
We are grateful to the many dedicated individuals with the Alberta Health Services (AHS) Tracheostomy Working Group who supported this project’s quality assessment including: Paulina Cunningham, Chelsea Sheldon, Carolyn Schmid, Denise Sorensen, Cassello Watson, and Leslie Wellman. The authors would like to thank research assistants Nekesia Abrams (UBC) and Nicole Anger (UBC) for their contributions to data extraction and Tamara Hempstock (AHS) for administrative support. We would also like to thank Alberta Health Services (AHS) Library Services.
Funding
This study was supported in part by internal funds: Dr. Skoretz’ School of Audiology and Speech Sciences startup funds from the University of British Columbia’s (UBC) Faculty of Medicine and Dr. Dawson’s Health Education England, West Midlands Clinical Academic Writing grant.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dawson, C., Riopelle, S.J. & Skoretz, S.A. Translating Dysphagia Evidence into Practice While Avoiding Pitfalls: Assessing Bias Risk in Tracheostomy Literature. Dysphagia 36, 409–418 (2021). https://doi.org/10.1007/s00455-020-10151-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-020-10151-w