Abstract
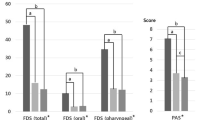
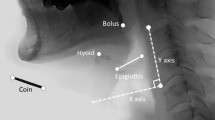
The purpose of this study was to compare the swallowing function and kinematics in stroke patients with and without tracheostomies. In this retrospective matched case–control study, we compared stroke patients with (TRACH group, n = 24) and without (NO-TRACH group, n = 24) tracheostomies. Patients were matched for age, sex, and stroke-type. Swallowing function was evaluated using the videofluoroscopic dysphagia scale (VDS) and functional oral intake scale (FOIS) obtained from videofluoroscopic swallow study (VFSS) images. Swallowing kinematics were evaluated using a two-dimensional kinematic analysis of the VFSS images. Mean duration of tracheostomy was 132.38 ± 150.46 days in the TRACH group. There was no significant difference in the total VDS score between the TRACH (35.17 ± 15.30) and NO-TRACH groups (29.25 ± 16.66, p = 0.247). FOIS was significantly lower in the TRACH group (2.33 ± 1.40) than in the NO-TRACH group (4.33 ± 1.79, p = 0.001). The TRACH group had a significantly lower maximum vertical displacement (15.23 ± 7.39 mm, p = 0.011) and velocity (54.99 ± 29.59 mm/s, p = 0.011), and two-dimensional velocity (61.07 ± 24.89 mm/s, p = 0.013) of the larynx than the NO-TRACH group (20.18 ± 5.70 mm, 82.23 ± 37.30 mm/s, and 84.40 ± 36.05 mm/s, respectively). Maximum horizontal velocity of the hyoid bone in the TRACH group (36.77 ± 16.97 mm/s) was also significantly lower than that in the NO-TRACH group (47.49 ± 15.73 mm/s, p = 0.032). This study demonstrated that stroke patients with tracheostomies had inferior swallowing function and kinematics than those without tracheostomies. A prospective longitudinal study is needed to elucidate the effect of a tracheostomy on swallowing recovery in stroke patients.

Similar content being viewed by others
References
Roth EJ, Lovell L, Harvey RL, Bode RK, Heinemann AW. Stroke rehabilitation: indwelling urinary catheters, enteral feeding tubes, and tracheostomies are associated with resource use and functional outcomes. Stroke. 2002;33:1845–50.
Walcott BP, Kamel H, Castro B, Kimberly WT, Sheth KN. Tracheostomy after severe ischemic stroke: a population-based study. J Stroke Cerebrovasc Dis. 2014;23:1024–9.
Hess DR, Altobelli NP. Tracheostomy tubes. Respir Care. 2014;59:956–71 discussion 971-953.
Bosel J. Tracheostomy in stroke patients. Curr Treat Options Neurol. 2014;16:274.
DeVita MA, Spierer-Rundback L. Swallowing disorders in patients with prolonged orotracheal intubation or tracheostomy tubes. Crit Care Med. 1990;18:1328–30.
Nash M. Swallowing problems in the tracheotomized patient. Otolaryngol Clin N Am. 1988;21:701–9.
Cameron JL, Reynolds J, Zuidema GD. Aspiration in patients with tracheostomies. Surg Gynecol Obstet. 1973;136:68–70.
Muz J, Mathog RH, Nelson R, Jones LA Jr. Aspiration in patients with head and neck cancer and tracheostomy. Am J Otolaryngol. 1989;10:282–6.
Elpern EH, Scott MG, Petro L, Ries MH. Pulmonary aspiration in mechanically ventilated patients with tracheostomies. Chest. 1994;105:563–6.
Feldman SA, Deal CW, Urquhart W. Disturbance of swallowing after tracheostomy. Lancet. 1966;1:954–5.
Bonanno PC. Swallowing dysfunction after tracheostomy. Ann Surg. 1971;174:29–33.
Eibling DE, Gross RD. Subglottic air pressure: a key component of swallowing efficiency. Ann Otol Rhinol Laryngol. 1996;105:253–8.
Clarett M, Andreu MF, Salvati IG, Donnianni MC, Montes GS, Rodriguez MG. Effect of subglottic air insufflation on subglottic pressure during swallowing. Med Intensiva. 2014;38:133–9.
Donzelli J, Brady S, Wesling M, Theisen M. Effects of the removal of the tracheotomy tube on swallowing during the fiberoptic endoscopic exam of the swallow (FEES). Dysphagia. 2005;20:283–9.
Leder SB, Ross DA. Confirmation of no causal relationship between tracheotomy and aspiration status: a direct replication study. Dysphagia. 2010;25:35–9.
Terk AR, Leder SB, Burrell MI. Hyoid bone and laryngeal movement dependent upon presence of a tracheotomy tube. Dysphagia. 2007;22:89–93.
Kang JY, Choi KH, Yun GJ, Kim MY, Ryu JS. Does removal of tracheostomy affect dysphagia? A kinematic analysis. Dysphagia. 2012;27:498–503.
Prigent H, Lejaille M, Terzi N, Annane D, Figere M, Orlikowski D, Lofaso F. Effect of a tracheostomy speaking valve on breathing-swallowing interaction. Intensive Care Med. 2012;38:85–90.
Amathieu R, Sauvat S, Reynaud P, Slavov V, Luis D, Dinca A, Tual L, Bloc S, Dhonneur G. Influence of the cuff pressure on the swallowing reflex in tracheostomized intensive care unit patients. Br J Anaesth. 2012;109:578–83.
Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke. 2005;36:2756–63.
Smithard DG, O’Neill PA, England RE, Park CL, Wyatt R, Martin DF, Morris J. The natural history of dysphagia following a stroke. Dysphagia. 1997;12:188–93.
Mann G, Hankey GJ, Cameron D. Swallowing function after stroke: prognosis and prognostic factors at 6 months. Stroke. 1999;30:744–8.
Han TR, Paik NJ, Park JW, Kwon BS. The prediction of persistent dysphagia beyond six months after stroke. Dysphagia. 2008;23:59–64.
Crary MA, Mann GD, Groher ME. Initial psychometric assessment of a functional oral intake scale for dysphagia in stroke patients. Arch Phys Med Rehabil. 2005;86:1516–20.
Seo HG, Oh BM, Han TR. Longitudinal changes of the swallowing process in subacute stroke patients with aspiration. Dysphagia. 2011;26:41–8.
Paik NJ, Kim SJ, Lee HJ, Jeon JY, Lim JY, Han TR. Movement of the hyoid bone and the epiglottis during swallowing in patients with dysphagia from different etiologies. J Electromyogr Kinesiol. 2008;18:329–35.
Lee SH, Oh BM, Chun SM, Lee JC, Min Y, Bang SH, Kim HC, Han TR. The accuracy of the swallowing kinematic analysis at various movement velocities of the hyoid and epiglottis. Ann Rehabil Med. 2013;37:320–7.
Pearce N. Analysis of matched case–control studies. BMJ. 2016;352:i969.
Conway A, Rolley JX, Fulbrook P, Page K, Thompson DR. Improving statistical analysis of matched case–control studies. Res Nurs Health. 2013;36:320–4.
Goldsmith T. Evaluation and treatment of swallowing disorders following endotracheal intubation and tracheostomy. Int Anesthesiol Clin. 2000;38:219–42.
Shaker R, Milbrath M, Ren J, Campbell B, Toohill R, Hogan W. Deglutitive aspiration in patients with tracheostomy: effect of tracheostomy on the duration of vocal cord closure. Gastroenterology. 1995;108:1357–60.
Ding R, Logemann JA. Swallow physiology in patients with trach cuff inflated or deflated: a retrospective study. Head Neck. 2005;27:809–13.
Matsuo K, Palmer JB. Anatomy and physiology of feeding and swallowing: normal and abnormal. Phys Med Rehabil Clin N Am. 2008;19:691–707.
Seo HG, Oh BM, Han TR. Swallowing kinematics and factors associated with laryngeal penetration and aspiration in stroke survivors with dysphagia. Dysphagia. 2016;31:160–8.
Nagy A, Molfenter SM, Peladeau-Pigeon M, Stokely S, Steele CM. The effect of bolus consistency on hyoid velocity in healthy swallowing. Dysphagia. 2015;30:445–51.
Martin-Harris B. Coordination of respiration and swallowing. GI Motility online, 2006. doi: 10.1038/gimo10.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Rights and permissions
About this article
Cite this article
Seo, H.G., Kim, JG., Nam, H.S. et al. Swallowing Function and Kinematics in Stroke Patients with Tracheostomies. Dysphagia 32, 393–400 (2017). https://doi.org/10.1007/s00455-016-9767-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-016-9767-x