Abstract
Purpose
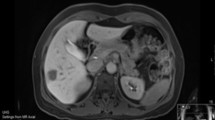
Laparoscopic right posterior sectionectomy (LRPS) is a technically demanding procedure. The aim of this article is to share our experience with LRPS and to highlight technical aspects of this procedure.
Methods
This is a single-center retrospective analysis of all patients who underwent LRPS between September 2011 and October 2017. Data were retrieved from a prospectively maintained database. Video-in-picture (VIP) technology is used to facilitate and to highlight the technical aspects of this procedure.
Results
In total, 18 patients underwent LRPS. Indication for surgery was mainly liver metastases (n = 11) and hepatocellular carcinoma (n = 6). The Glissonean approach for inflow control was used in 13 patients. Median operative time was 162 (140–190) minutes. Median blood loss was 325 mL (IQR: 150–450). One conversion (5.5%) was required. There were two minor complications and one major complication. Median hospital stay was 6 days (range 5–8 days). All patients had an R0 resection. There was no 90-day mortality.
Conclusion
The results of our experience in LRPS add weight to the feasibility and safety of this approach.





Similar content being viewed by others
Abbreviations
- LRPS:
-
Laparoscopic right posterior sectionectomy
- VIP:
-
Video-in-picture
- CVP:
-
Central venous pressure
- IOUS:
-
Intraoperative ultrasonography
- RHV:
-
Right hepatic vein
- IQR:
-
Interquartile range
- ERCP:
-
Endoscopic retrograde cholangiopancreatography
- LLR:
-
Laparoscopic liver resection
- HPB:
-
Hepato-pancreato-biliary
- HCC:
-
Hepatocellular carcinoma
- CRLM:
-
Colorectal liver metastasis
- LHV:
-
Left hepatic vein
References
Zhang X-L, Liu R-F, Zhang D, Zhang Y-S, Wang T (2017) Laparoscopic versus open liver resection for colorectal liver metastases: a systematic review and meta-analysis of studies with propensity score-based analysis. Int J Surg 44:191–203. https://doi.org/10.1016/j.ijsu.2017.05.073
Fretland ÅA, Dagenborg VJ, Bjørnelv GMW, Kazaryan AM, Kristiansen R, Fagerland MW, Hausken J, Tønnessen TI, Abildgaard A, Barkhatov L, Yaqub S, Røsok BI, Bjørnbeth BA, Andersen MH, Flatmark K, Aas E, Edwin B (2017) Laparoscopic versus open resection for colorectal liver metastases. Ann Surg 267:199–207. https://doi.org/10.1097/SLA.0000000000002353
Guro H, Cho JY, Han H-S, Yoon Y-S, Choi Y, Kim S, Kim K, Hyun IG (2018) Outcomes of major laparoscopic liver resection for hepatocellular carcinoma. Surg Oncol 27:31–35. https://doi.org/10.1016/J.SURONC.2017.11.006
Cho JY, Han HS, Yoon YS, Shin SH (2008) Feasibility of laparoscopic liver resection for tumors located in the posterosuperior segments of the liver, with a special reference to overcoming current limitations on tumor location. Surgery 144:32–38. https://doi.org/10.1016/j.surg.2008.03.020
Cheng K-C, Yeung Y-P, Ho K-M, Chan FK-M (2015) Laparoscopic right posterior sectionectomy for malignant lesions: an anatomic approach. J Laparoendosc Adv Surg Tech A 25:646–650. https://doi.org/10.1089/lap.2015.0166
Siddiqi NN, Abuawwad M, Halls M, Rawashdeh A, Giovinazzo F, Aljaiuossi A, Wicherts D, D’Hondt M, Hilal MA, D’Hondt M, Hilal MA (2017) Laparoscopic right posterior sectionectomy (LRPS): surgical techniques and clinical outcomes. Surg Endosc 32:1–8. https://doi.org/10.1007/s00464-017-5958-2
Ciria R, Cherqui D, Geller DA, Briceno J, Wakabayashi G (2016) Comparative short-term benefits of laparoscopic liver resection: 9000 cases and climbing. Ann Surg 263:761–777. https://doi.org/10.1097/SLA.0000000000001413
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibañes E, Pekolj J, Slankamenac K, Bassi C, Graf R, Vonlanthen R, Padbury R, Cameron JLMM (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250:187–196
Halls MC, Alseidi A, Berardi G, Cipriani F, Van der Poel M, Davila D, Ciria R, Besselink M, D’Hondt M, Dagher I, Alrdrighetti L, Troisi RI, Abu Hilal M (2018) A comparison of the learning curves of laparoscopic liver surgeons in differing stages of the IDEAL paradigm of surgical innovation. Ann Surg 1. https://doi.org/10.1097/SLA.0000000000002996
D’Hondt M, Yoshihara E, Vansteenkiste F, Steelant PJ, Van Ooteghem B, Pottel H, Devriendt D, Van Rooy F (2016) Laparoscopic parenchymal preserving hepatic resections in semiprone position for tumors located in the posterosuperior segments. Langenbeck's Arch Surg 401:255–262. https://doi.org/10.1007/s00423-016-1375-6
Ryckx A, Christiaens C, Clarysse M, Vansteenkiste F, Steelant PJ, Sergeant G, Parmentier I, Pottel H, D’Hondt M (2017) Central venous pressure drop after hypovolemic phlebotomy is a strong independent predictor of intraoperative blood loss during liver resection. Ann Surg Oncol 24:1367–1375. https://doi.org/10.1245/s10434-016-5737-7
Ikeda T, Toshima T, Harimoto N, Yamashita Y, Ikegami T, Yoshizumi T, Soejima Y, Shirabe K, Maehara Y (2014) Laparoscopic liver resection in the semiprone position for tumors in the anterosuperior and posterior segments, using a novel dual-handling technique and bipolar irrigation system. Surg Endosc 28:2484–2492. https://doi.org/10.1007/s00464-014-3469-y
Ikeda T, Yonemura Y, Ueda N, Kabashima A, Shirabe K, Taketomi A, Yoshizumi T, Uchiyama H, Harada N, Ijichi H, Kakeji Y, Morita M, Tsujitani S, Maehara Y (2011) Pure laparoscopic right hepatectomy in the semi-prone position using the intrahepatic glissonian approach and a modified hanging maneuver to minimize intraoperative bleeding. Surg Today 41:1592–1598. https://doi.org/10.1007/s00595-010-4479-6
Machado MAC, Makdissi FF, Galvão FH, Machado MCC (2008) Intrahepatic Glissonian approach for laparoscopic right segmental liver resections. Am J Surg 196:38–43. https://doi.org/10.1016/j.amjsurg.2007.10.027
Galperin EI, Karagiulian SR (1989) A new simplified method of selective exposure of hepatic pedicles for controlled hepatectomies. HPB Surg 1:119–130. https://doi.org/10.1155/1989/28161
Machado MAC, Surjan RC, Basseres T, Schadde E, Costa FP, Makdissi FF (2016) The laparoscopic Glissonian approach is safe and efficient when compared with standard laparoscopic liver resection: results of an observational study over 7 years. Surgery 160:643–651. https://doi.org/10.1016/j.surg.2016.01.017
Knol J, Chadi SA (2016) Transanal total mesorectal excision: technical aspects of approaching the mesorectal plane from below. Minim Invasive Ther Allied Technol 25:257–270. https://doi.org/10.1080/13645706.2016.1206572
Ciria R, Cherqui D, Geller DA, Briceno J, Wakabayashi G (2016) Comparative short-term benefits of laparoscopic liver resection. Ann Surg 263:761–777. https://doi.org/10.1097/SLA.0000000000001413
Nguyen KT, Gamblin TC, Geller DA (2009) World review of laparoscopic liver resection—2,804 patients. Ann Surg 250:831–841. https://doi.org/10.1097/SLA.0b013e3181b0c4df
Abu Hilal M, Aldrighetti L, Dagher I, Edwin B, Troisi RI, Alikhanov R, Aroori S, Belli G, Besselink M, Briceno J, Gayet B, D’Hondt M, Lesurtel M, Menon K, Lodge P, Rotellar F, Santoyo J, Scatton O, Soubrane O, Sutcliffe R, Van Dam R, White S, Halls MC, Cipriani F, Van der Poel M, Ciria R, Barkhatov L, Gomez-Luque Y, Ocana-Garcia S, Cook A, Buell J, Clavien P-A, Dervenis C, Fusai G, Geller D, Lang H, Primrose J, Taylor M, Van Gulik T, Wakabayashi G, Asbun H, Cherqui D (2017) The southampton consensus guidelines for laparoscopic liver surgery. Ann Surg XX:1. https://doi.org/10.1097/SLA.0000000000002524
Wakabayashi G, Cherqui D, Geller DA, Buell JF, Kaneko H, Han HS, Asbun H, O’Rourke N, Tanabe M, Koffron AJ, Tsung A, Soubrane O, Machado MA, Gayet B, Troisi RI, Pessaux P, Van Dam RM, Scatton O, Hilal MA, Belli G, Kwon CHD, Edwin B, Choi GH, Aldrighetti LA, Cai X, Cleary S, Chen KH, Schön MR, Sugioka A, Tang CN, Herman P, Pekolj J, Chen XP, Dagher I, Jarnagin W, Yamamoto M, Strong R, Jagannath P, Lo CM, Clavien PA, Kokudo N, Barkun J, Strasberg SM (2015) Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in Morioka. Ann Surg 261:619–629. https://doi.org/10.1097/SLA.0000000000001184
Mise Y, Aloia TA, Brudvik KW, Schwarz L, Vauthey JN, Conrad C (2016) Parenchymal-sparing hepatectomy in colorectal liver metastasis improves salvageability and survival. Ann Surg 263:146–152. https://doi.org/10.1097/SLA.0000000000001194
Montalti R, Tomassini F, Laurent S, Smeets P, De Man M, Geboes K, Libbrecht LJ, Troisi RI (2015) Impact of surgical margins on overall and recurrence-free survival in parenchymal-sparing laparoscopic liver resections of colorectal metastases. Surg Endosc 29:2736–2747. https://doi.org/10.1007/s00464-014-3999-3
Gold JS, Are C, Kornprat P, Jarnagin WR, Gönen M, Fong Y, DeMatteo RP, Blumgart LH, D’Angelica M (2008) Increased use of parenchymal-sparing surgery for bilateral liver metastases from colorectal cancer is associated with improved mortality without change in oncologic outcome: trends in treatment over time in 440 patients. Ann Surg 247:109–117. https://doi.org/10.1097/SLA.0b013e3181557e47
Von Heesen M, Schuld J, Sperling J, Grünhage F, Lammert F, Richter S, Schilling MK, Kollmar O (2012) Parenchyma-preserving hepatic resection for colorectal liver metastases. Langenbeck's Arch Surg 397:383–395. https://doi.org/10.1007/s00423-011-0872-x
Abu Hilal M, Lodge JPA (2008) Pushing back the frontiers of resectability in liver cancer surgery. Eur J Surg Oncol 34:272–280
Tuttle TM, Curley SA, Roh MS (1997) Repeat hepatic resection as effective treatment of recurrent colorectal liver metastases. Ann Surg Oncol 4:125–130
Moris D, Ronnekleiv-Kelly S, Rahnemai-Azar AA, Felekouras E, Dillhoff M, Schmidt C, Pawlik TM (2017) Parenchymal-sparing versus anatomic liver resection for colorectal liver metastases: a systematic review. J Gastrointest Surg 21:1076–1085. https://doi.org/10.1007/s11605-017-3397-y
Buell JF, Cherqui D, Geller DA, O’Rourke N, Iannitti D, Dagher I, Koffron AJ, Thomas M, Gayet B, Han HS, Wakabayashi G, Belli G, Kaneko H, Ker C-G, Scatton O, Laurent A, Abdalla EK, Chaudhury P, Dutson E, Gamblin C, D’Angelica M, Nagorney D, Testa G, Labow D, Manas D, Poon RT, Nelson H, Martin R, Clary B, Pinson WC, Martinie J, Vauthey J-N, Goldstein R, Roayaie S, Barlet D, Espat J, Abecassis M, Rees M, Fong Y, McMasters KM, Broelsch C, Busuttil R, Belghiti J, Strasberg S, Chari RS (2009) The international position on laparoscopic liver surgery. Ann Surg 250:825–830. https://doi.org/10.1097/SLA.0b013e3181b3b2d8
Di Fabio F, Samim M, Di Gioia P, Godeseth R, Pearce NW, Abu Hilal M (2014) Laparoscopic major hepatectomies: clinical outcomes and classification. World J Surg 38:3169–3174. https://doi.org/10.1007/s00268-014-2724-7
van der Poel MJ, Huisman F, Busch OR, Abu Hilal M, van Gulik TM, Tanis PJ, Besselink MG (2017) Stepwise introduction of laparoscopic liver surgery: validation of guideline recommendations. HPB 19:894–900. https://doi.org/10.1016/j.hpb.2017.06.007
Tomlinson JS, Jarnagin WR, DeMatteo RP, Fong Y, Kornprat P, Gonen M, Kemeny N, Brennan MF, Blumgart LH, D’Angelica M (2007) Actual 10-year survival after resection of colorectal liver metastases defines cure. J Clin Oncol 25:4575–4580. https://doi.org/10.1200/JCO.2007.11.0833
Fisher SB, Kneuertz PJ, Dodson RM, Patel SH, Maithel SK, Sarmiento JM, Russell MC, Cardona K, Choti MA, Staley CA, Pawlik TM, Kooby DA (2013) A comparison of right posterior sectorectomy with formal right hepatectomy: a dual-institution study. HPB 15:753–762. https://doi.org/10.1111/hpb.12126
Acknowledgements
Video-in-picture technology (Non-profit iLappSurgery Foundation, Hasselt, Belgium) was used as an educational video tool.
Author information
Authors and Affiliations
Contributions
MD participated in the study conception and design. MD, SO, and MV participated in the analysis and interpretation of data. All authors participated in the acquisition of data, drafting of the manuscript, and critical revision of the manuscript.
Corresponding author
Ethics declarations
This article was written in accordance with the ethical standards of the institutional review board and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent was obtained from all human subjects as is the standard of care and as with compliance with institution guidelines.
Conflicts of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
D’Hondt, M., Ovaere, S., Knol, J. et al. Laparoscopic right posterior sectionectomy: single-center experience and technical aspects. Langenbecks Arch Surg 404, 21–29 (2019). https://doi.org/10.1007/s00423-018-1731-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-018-1731-9