Abstract
Introduction
Colorectal liver metastases develop in 50% of patients diagnosed with colorectal cancer. Surgical resection for colorectal liver metastasis typically involves either anatomical resection (AR) or parenchymal-sparing hepatectomy (PSH). The objective of the current study was to analyze data on parenchymal versus non-parenchymal-sparing hepatic resections for CLM.
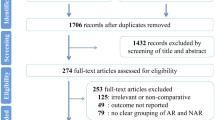
Methods
A systematic review of the literature regarding parenchymal-sparing hepatectomy was performed. MEDLINE/PubMed, Cochrane, and EMBASE databases were searched for publications containing the following medical subject headings (MeSH): “Colorectal Neoplasms,” “Neoplasm Metastasis,” “Liver Neoplasms” and “Hepatectomy”. Besides, the following keywords were used to complete the literature search: “Hepatectomy,” “liver resection,” “hepatic resection,” “anatomic/anatomical,” “nonanatomic/ nonanatomical,” “major,” “minor,” “limited,” “wedge,” “CRLM/CLM,” and “colorectal liver metastasis.” Data was reviewed, aggregated, and analyzed.
Results
Two thousand five hundred five patients included in 12 studies who underwent either PSH (n = 1087 patients) or AR (n = 1418 patients) were identified. Most patients had a primary tumor that originated in the colon (PSH 52.2–74.4% vs. AR 53.9–74.3%) (P = 0.289). The majority of studies included a large subset of patients with only a solitary tumor with a reported median tumor number of 1–2 regardless of whether the patient underwent PSH or AR. Median EBL was no different among patients undergoing PSH (100–896 mL) versus AR (200–1489 mL) for CLM (P = 0.248). There was no difference in median length-of-stay following PSH (6–17 days) versus AR (7–15 days) (P = 0.747). While there was considerable inter-study variability regarding margin status, there was no difference in the incidence of R0 resection among patients undergoing PSH (66.7–100%) versus AR (71.6–98.6%) (P = 0.58). When assessing overall survival, there was no difference whether resection of CLM was performed with PSH (5 years OS: mean 44.7%, range 29–62%) or AR (5 years OS: mean 44.6%, range 27–64%) (P = 0.97).
Conclusion
PSH had a comparable safety and efficacy profile compared with AR and did not compromise oncologic outcomes. PSH should be considered an appropriate surgical approach to treatment for patients with CLM that facilitates preservation of hepatic parenchyma.

Similar content being viewed by others
References
Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. International journal of cancer. 2010;127(12):2893–2917.
Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA: a cancer journal for clinicians. 2012;62(1):10–29.
Alvarez FA, Sanchez Claria R, Oggero S, de Santibanes E. Parenchymal-sparing liver surgery in patients with colorectal carcinoma liver metastases. World journal of gastrointestinal surgery. 2016;8(6):407–423.
Abdalla EK, Adam R, Bilchik AJ, Jaeck D, Vauthey JN, Mahvi D. Improving resectability of hepatic colorectal metastases: expert consensus statement. Annals of surgical oncology. 2006;13(10):1271–1280.
de Haas RJ, Wicherts DA, Andreani P, et al. Impact of expanding criteria for resectability of colorectal metastases on short- and long-term outcomes after hepatic resection. Annals of surgery. 2011;253(6):1069–1079.
Saiura A, Yamamoto J, Koga R, et al. Favorable outcome after repeat resection for colorectal liver metastases. Annals of surgical oncology. 2014;21(13):4293–4299.
Moris D, Dimitrokallis N, Oikonomou D, Mpaili E, Felekouras E. Less is more: salvageability as the new creed in surgery of colorectal liver metastatic disease. Journal of B.U.ON. : official journal of the Balkan Union of Oncology. 2016a;21(6):1562–1563.
Moris D, Dimitroulis D, Vernadakis S, et al. Parenchymal-sparing Hepatectomy as the New Doctrine in the Treatment of Liver-metastatic Colorectal Disease: Beyond Oncological Outcomes. Anticancer research. 2017;37(1):9–14.
Zorzi D, Mullen JT, Abdalla EK, et al. Comparison between hepatic wedge resection and anatomic resection for colorectal liver metastases. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract. 2006;10(1):86–94.
Lalmahomed ZS, Ayez N, van der Pool AE, Verheij J, JN IJ, Verhoef C. Anatomical versus nonanatomical resection of colorectal liver metastases: is there a difference in surgical and oncological outcome? World journal of surgery. 2011;35(3):656–661.
Wicherts DA, Miller R, de Haas RJ, et al. Long-term results of two-stage hepatectomy for irresectable colorectal cancer liver metastases. Annals of surgery. 2008;248(6):994–1005.
Masi G, Cupini S, Marcucci L, et al. Treatment with 5-fluorouracil/folinic acid, oxaliplatin, and irinotecan enables surgical resection of metastases in patients with initially unresectable metastatic colorectal cancer. Annals of surgical oncology. 2006;13(1):58–65.
Adam R, Delvart V, Pascal G, et al. Rescue surgery for unresectable colorectal liver metastases downstaged by chemotherapy: a model to predict long-term survival. Annals of surgery. 2004;240(4):644–657; discussion 657-648.
Charnsangavej C, Clary B, Fong Y, Grothey A, Pawlik TM, Choti MA. Selection of patients for resection of hepatic colorectal metastases: expert consensus statement. Annals of surgical oncology. 2006;13(10):1261–1268.
Hamady ZZ, Lodge JP, Welsh FK, et al. One-millimeter cancer-free margin is curative for colorectal liver metastases: a propensity score case-match approach. Annals of surgery. 2014;259(3):543–548.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Bmj. 2009;339:b2535.
Kokudo N, Tada K, Seki M, et al. Anatomical major resection versus nonanatomical limited resection for liver metastases from colorectal carcinoma. American journal of surgery. 2001;181(2):153–159.
DeMatteo RP, Palese C, Jarnagin WR, Sun RL, Blumgart LH, Fong Y. Anatomic segmental hepatic resection is superior to wedge resection as an oncologic operation for colorectal liver metastases. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract. 2000;4(2):178–184.
Stewart GD, O’Suilleabhain CB, Madhavan KK, Wigmore SJ, Parks RW, Garden OJ. The extent of resection influences outcome following hepatectomy for colorectal liver metastases. European journal of surgical oncology : the journal of the European Society of Surgical Oncology and the British Association of Surgical Oncology. 2004;30(4):370–376.
Finch RJ, Malik HZ, Hamady ZZ, et al. Effect of type of resection on outcome of hepatic resection for colorectal metastases. The British journal of surgery. 2007;94(10):1242–1248.
Sarpel U, Bonavia AS, Grucela A, Roayaie S, Schwartz ME, Labow DM. Does anatomic versus nonanatomic resection affect recurrence and survival in patients undergoing surgery for colorectal liver metastasis? Annals of surgical oncology. 2009;16(2):379–384.
Guzzetti E, Pulitano C, Catena M, et al. Impact of type of liver resection on the outcome of colorectal liver metastases: a case-matched analysis. Journal of surgical oncology. 2008;97(6):503–507.
von Heesen M, Schuld J, Sperling J, et al. Parenchyma-preserving hepatic resection for colorectal liver metastases. Langenbeck's archives of surgery / Deutsche Gesellschaft fur Chirurgie. 2012;397(3):383–395.
Matsuki R, Mise Y, Saiura A, Inoue Y, Ishizawa T, Takahashi Y. Parenchymal-sparing hepatectomy for deep-placed colorectal liver metastases. Surgery. 2016.
Matsumura M, Mise Y, Saiura A, et al. Parenchymal-Sparing Hepatectomy Does Not Increase Intrahepatic Recurrence in Patients with Advanced Colorectal Liver Metastases. Annals of surgical oncology. 2016.
Chouillard E, Cherqui D, Tayar C, Brunetti F, Fagniez PL. Anatomical bi- and trisegmentectomies as alternatives to extensive liver resections. Annals of surgery. 2003;238(1):29–34.
de Santibanes E, Sanchez Claria R, Palavecino M, Beskow A, Pekolj J. Liver metastasis resection: a simple technique that makes it easier. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract. 2007;11(9):1183–1187.
Machado MA, Herman P, Makdissi FF, Figueira ER, Bacchella T, Machado MC. Feasibility of bisegmentectomy 7-8 is independent of the presence of a large inferior right hepatic vein. Journal of surgical oncology. 2006;93(4):338–342.
Torzilli G, Procopio F, Donadon M, et al. Upper transversal hepatectomy. Annals of surgical oncology. 2012;19(11):3566.
Torzilli G, Procopio F, Cimino M, et al. Hepatic vein-sparing hepatectomy for multiple colorectal liver metastases at the caval confluence. Annals of surgical oncology. 2015;22(5):1576.
Torzilli G, Donadon M, Marconi M, et al. Systematic extended right posterior sectionectomy: a safe and effective alternative to right hepatectomy. Annals of surgery. 2008;247(4):603–611.
Mise Y, Aloia TA, Brudvik KW, Schwarz L, Vauthey JN, Conrad C. Parenchymal-sparing Hepatectomy in Colorectal Liver Metastasis Improves Salvageability and Survival. Annals of surgery. 2016;263(1):146–152.
Imai K, Allard MA, Benitez CC, et al. Early Recurrence After Hepatectomy for Colorectal Liver Metastases: What Optimal Definition and What Predictive Factors? The oncologist. 2016;21(7):887–894.
Butte JM, Gonen M, Allen PJ, et al. Recurrence After Partial Hepatectomy for Metastatic Colorectal Cancer: Potentially Curative Role of Salvage Repeat Resection. Annals of surgical oncology. 2015;22(8):2761–2771.
Gold JS, Are C, Kornprat P, et al. Increased use of parenchymal-sparing surgery for bilateral liver metastases from colorectal cancer is associated with improved mortality without change in oncologic outcome: trends in treatment over time in 440 patients. Annals of surgery. 2008;247(1):109–117.
Pang YY. The Brisbane 2000 terminology of liver anatomy and resections. HPB 2000; 2:333-39. HPB : the official journal of the International Hepato Pancreato Biliary Association. 2002;4(2):99; author reply 99-100.
Sui CJ, Cao L, Li B, et al. Anatomical versus nonanatomical resection of colorectal liver metastases: a meta-analysis. International journal of colorectal disease. 2012;27(7):939–946.
Nagakura S, Shirai Y, Yokoyama N, Wakai T, Suda T, Hatakeyama K. Major hepatic resection reduces the probability of intrahepatic recurrences following resection of colorectal carcinoma liver metastases. Hepato-gastroenterology. 2003;50(51):779–783.
Margonis GA, Sasaki K, Andreatos N, et al. KRAS Mutation Status Dictates Optimal Surgical Margin Width in Patients Undergoing Resection of Colorectal Liver Metastases. Annals of surgical oncology. 2016.
Cady B, Jenkins RL, Steele GD, Jr., et al. Surgical margin in hepatic resection for colorectal metastasis: a critical and improvable determinant of outcome. Annals of surgery. 1998;227(4):566–571.
Ekberg H, Tranberg KG, Andersson R, et al. Determinants of survival in liver resection for colorectal secondaries. The British journal of surgery. 1986;73(9):727–731.
Yan TD, Sim J, Black D, Niu R, Morris DL. Systematic review on safety and efficacy of repeat hepatectomy for recurrent liver metastases from colorectal carcinoma. Annals of surgical oncology. 2007;14(7):2069–2077.
Oba M, Hasegawa K, Shindoh J, et al. Survival benefit of repeat resection of successive recurrences after the initial hepatic resection for colorectal liver metastases. Surgery. 2016;159(2):632–640.
Pandanaboyana S, Bell R, White A, et al. Impact of parenchymal preserving surgery on survival and recurrence after liver resection for colorectal liver metastasis. ANZ journal of surgery. 2016.
Jarnagin WR, Gonen M, Fong Y, et al. Improvement in perioperative outcome after hepatic resection: analysis of 1,803 consecutive cases over the past decade. Annals of surgery. 2002;236(4):397–406; discussion 406-397.
Moris D, Felekouras E, Chrousos GP. No Cytokine Is an Island: IL-6 Alone Is not Sufficient to Predict Morbidity after a Major Abdominal Surgery. Annals of surgery. 2016b.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Funding
None.
Rights and permissions
About this article
Cite this article
Moris, D., Ronnekleiv-Kelly, S., Rahnemai-Azar, A.A. et al. Parenchymal-Sparing Versus Anatomic Liver Resection for Colorectal Liver Metastases: a Systematic Review. J Gastrointest Surg 21, 1076–1085 (2017). https://doi.org/10.1007/s11605-017-3397-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-017-3397-y