Abstract
Background
To specify peripheral nerve affection in autosomal recessive spastic ataxia of Charlevoix-Saguenay (ARSACS) by correlating high-resolution nerve ultrasound and nerve conduction studies.
Methods
We assessed a cohort of 11 ARSACS patients with standardized nerve conduction studies and high-resolution ultrasound of peripheral nerves and compared nerve ultrasound findings to a healthy control group matched for age, sex, size and weight.
Results
Mean age of patients was 39.0 (± 14.1) years and disease duration at assessment 30.6 (± 12.5) years. All patients presented with a spasticity, ataxia and peripheral neuropathy. Neuropathy appeared to be primarily demyelinating in 9/11 cases and was not classifiable in 2/11 cases due to not evocable potentials. Nerve ultrasound revealed a normal ultrasound pattern sum score (UPSS) in each ARSACS patient and no significant nerve enlargement compared to the control group.
Conclusions
Peripheral neuropathy in ARSACS showed primarily demyelinating rather than axonal characteristics and presented without nerve enlargement. As demyelinating neuropathies do commonly present enlarged nerves we recommend further genetic testing of the SACS gene in patients who present with this combination of demyelinating neuropathy without nerve enlargement. ARSACS cases that initially presented only with neuropathy without spasticity or ataxia and therefore were misdiagnosed as Charcot-Marie-Tooth disease are supporting this suggestion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
High-resolution ultrasound (HRUS) of nerves is a rapidly expanding field. As an addition to nerve conduction studies (NCS) it helps further stratify neuropathies.
Generally, ultrasound examinations show nerve enlargement in demyelinating neuropathies, whereas most axonal neuropathies do not [1]. Previous data show nerve enlargement in hereditary caused neuropathies like Charcot–Marie–Tooth disease (CMT) [2,3,4,5] or hereditary neuropathy with liability to pressure palsy (HNPP) [4, 5]. Nerve enlargement was also reported for autoimmune caused neuropathies like chronic inflammatory demyelinating polyneuropathy (CIDP) [2, 3, 6], Guillain–Barre Syndrome (GBS) [7], multifocal motor neuropathy (MMN) [2, 8], demyelinating neuropathy in monoclonal gammopathy of undetermined significance (MGUS) [9], and neuropathy with anti-MAG (myelin-associated glycoprotein) antibodies [10].
In contrast, axonal neuropathies commonly do not show nerve enlargement or only to a mild degree. Axonal neuropathy caused by vasculitis [11, 12], sarcoidosis [13], or sporadic mononeuropathies without trauma (e.g., borreliosis or hepatitis E) [14] are exceptions that often present with focal nerve swelling.
There is a lack of data regarding HRUS in genetic neurodegenerative diseases other than primary hereditary neuropathies. Recently nerve enlargement was shown in demyelinating X-linked adrenomyeloneuropathy (AMN) [15], metachromatic leukodystrophy [16], and cerebrotendinous xanthomatosis (CTX) [17].
This study investigates HRUS data compared to electrophysiological data in patients suffering from autosomal recessive spastic ataxia of Charlevoix-Saguenay (ARSACS).
ARSACS is caused by bi-allelic mutations in the SACS gene encoding sacsin and is characterized as an early onset spastic cerebellar ataxia with peripheral neuropathy [18]. Characteristic but not obligatory imaging findings include streaky pontine hypointensities in magnetic resonance imaging (MRI) and in some cases also hypertrophic retinal myelinated fibers. Further, epilepsy, hearing loss, urinary dysfunction, and mild intellectual disability have been reported [19,20,21,22,23,24]. Cases have been reported, which primarily presented with an isolated neuropathy, leading to the initial diagnosis of CMT [19, 25].
Findings in nerve conduction studies (NCS) in these patients are heterogenic and include not only primarily axonal polyneuropathic but also primary demyelinating or mixed demyelinating and axonal changes [19, 21,22,23, 26].
Patients and methods
Cohort
Included in this study were 11 genetically diagnosed ARSACS patients with homozygous or two compound heterozygous mutations in the SACS gene (Table 1).
Between 09/2019 and 06/2020 the participants have been examined in our specialized outpatient clinic for ataxia and received an additional electrophysiological work-up, including NCS and nerve ultrasound. This study was approved by the local ethic committee of the University of Tübingen (702/2015BO2) and conform with the World Medical Association Declaration of Helsinki. All examinations were undertaken with understanding and written informed consent from all participants. Further nerve ultrasound measurements were obtained for an age, sex, size, and weight-matched healthy control group with no medical history or symptoms of neuropathy.
Clinical assessment and electrophysiology
The clinical assessment involved a standardized neurological examination by a movement disorder specialist, including the Scale for the Assessment and Rating of Ataxia (SARA) [27].
Nerve conduction studies were performed with standard conditions as described before [28], using a Dantec® Keypoint® G4 workstation (Natus Medical Inc., San Carlos, California, USA). Motor nerve conduction studies included distal motor latencies (DML), compound muscle action potentials (CMAP), and motor nerve conduction velocities (MNCV) of the ulnar (U), fibular (F), and tibial nerve (T). Sensory NCS included sensory nerve action potentials (SNAP) and sensory nerve conduction velocities (SNCV) of the ulnar (U) and sural nerve (S).
In all patients, motor nerves were tested alternately on both sides, for example, left side for ulnar and tibial nerve, right side for the fibular nerve. Sensory nerves were tested on the right side; however, changes were made individually to each patient, without deviating from the overall protocol.
Neuropathy was defined as demyelinating if NCV was slower than 75% or distal latency longer than 130% of the norm and as axonal if amplitudes were decreased with only mild reduction of NCV or distal latency, accordingly to Preston and Shapiro 2013 [29] (comparable to the guidelines of the European Federation of Neurological Societies and the Peripheral Nerve Society for CIDP [30]).
High-resolution nerve ultrasound
High-resolution B-mode ultrasound was performed accordingly to a previously published protocol [17] with a high-resolution probe (24 MHz broad band linear probe, Aplio i800, Canon Medical Systems GmbH, Neuss, Germany). Nerve ultrasound covered easily accessible peripheral nerves on the right body site (median, ulnar, radial, tibial, fibular, sural and vagal nerve, as well as the C5 and C6 nerve roots) and was performed by well-experienced sonographers, assessing the cross-sectional area (CSA) of peripheral nerves and diameter for cervical roots. In a nerve enlargement of > 150% 2 points and in a nerve enlargement > 100% but less than 150% 1 point are given.
With adjusted boundary values we summed up the results to the Ultrasound Pattern Sum Score (UPSS) reaching from 0 to 22 points, whereas a sum of ≤ 3 points is supposed to be not pathological [31]. For A09 adolescent boundary values were used [32].
Echo intensity was evaluated semi-quantitatively by defining nerves as hypoechogenic if isointense with blood vessels lumen and hyperechogenic if isointense with lymph nodes [6].
Statistical analysis
All analyses were conducted using IBM SPSS Statistics, version 27.0.0.0 (Chicago, IL, USA). Results of descriptive analyses are given as mean ± standard deviation (SD) if normally distributed or median and inter quartile range (IQR) if not normally distributed, after testing normality with the Shapiro–Wilk test. ARSACS patients and the control group were compared using an independent-sample t-test for normally distributed variables (with testing the equality of variance by the Levene test) and for non-normally distributed variables with the Mann–Whitney U test. Sex, as the only categorical variable, was not tested because of exact matching in both groups. Significance level for the nerve ultrasound results was corrected for multiple comparisons and set at p ≤ 0.003. For all other tests significance level was set at p ≤ 0.05.
Results
Cohort
An overview of the included participants with their clinical and genetic characteristics is given in Table 1. The mean age at assessment was 39.0 (± 14.1) years with a mean disease duration of 30.6 (± 12.5) years since retrospectively the first ARSACS-related symptom occurred.
Clinical assessment and electrophysiology
In total, 11 patients, registered to our outpatient ataxia department of the university hospital Tuebingen and Essen diagnosed with ARSACS, were included in this study. All patients clinically presented with the typical triad of ARSACS including spasticity, ataxia, and peripheral neuropathy (see Table 1). Mean SARA score was 19.5 (± 7.2) points.
In all 11 cases SNAP of the sural and ulnar nerve was extinguished.
NCS showed a demyelinating neuropathy in 10/11 cases, defined by a reduced NCV of ≤ 75% of the norm or a distal latency longer than 130% of the norm. In one patient, neither MSAP nor SNAP could be evoked; therefore, no further classification was possible. Late response was determined for the ulnar and tibial nerve. Since the MUAP amplitude of the tibial nerve was not evocable in 8 of 11 patients, the late response of the ulnar nerve was primarily considered when conducting the analysis. In 5 of 8 patients’ late response was elongated by > 30% (see Table 2). All nerve conduction study data values were compared to normative values adapted from literature.
High-resolution nerve ultrasound
Nerve ultrasound was performed in 10 of 11 patients, in 5 investigated patients subtle nerve swelling was seen. The UPSS varied from a minimum of 0 to 2 points and is therefore non-pathological (Tables 2 and 3). Exemplary ultrasound images of the right ulnar nerve at the upper arm are shown in Fig. 1 for one ARSACS patient (A01) in comparison to a CIDP patient and a control group patient. The distribution pattern was inhomogenic and nerve swelling did not only affect the peripheral nerves but also affected the cervical nerve roots. Nerve ultrasound results were compared to a control group with no significant difference in sex, age, size, and weight. After correcting for multiple testing (p ≤ 0.003), no significant differences of CSA values were observed. The results of the group comparison are reported in Table 3.
Further, nerve ultrasound of an exemplary patient suffering from chronic inflammatory demyelinating polyneuropathy (CIDP) showed a statistically significant higher UPSS (p < 0.0.5).
Discussion
Due to the rarity ARSACS, the current literature lacks a clear description of NCS findings and ultrasound data. Especially in regard to NCS, data described in literature are contradictive.
In the previously described studies, demyelinating or axonal neuropathy was either not clearly defined or defined as demyelinating if nerve conduction velocity was reduced, axonal if action potentials were affected, or mixed if both signs were seen, while the current EAN or AAN criteria and guidelines were not taken into consideration.
A further limitation is the ambiguity of which nerves were examined. Therefore, specified data vary from a clear description of which nerves are included in the performed NCS [19, 20, 22, 26], while other studies do not provide any further details [21, 23]. Our data show that ARSACS patients present with demyelinating polyneuropathy, accompanying the underlying pathophysiology of the disease:
To date, the role of sacsin is not fully understood, although an axonal and Schwann cell dysfunction in patients with sacsin mutations is implicated [33].
Therefore, ARSACS differs from other common recessive ataxias with neuropathy like polymerase gamma (POLG)-related ataxia [34, 35], the cerebellar ataxia, neuropathy and vestibular areflexia syndrome (CANVAS) [36], Friedreich’s ataxia (FRDA) [37], Ataxia telangiectasia (AT) [38], and ataxia with oculomotor apraxia (AOA) Type 1 [39] and 2 [40], which are all presenting a mainly axonal type of neuropathy. Histopathologically, peripheral nerve findings in ARSACS are well reflecting demyelination by demonstrating onion bulbs, thinning of myelin sheaths, and loss of large myelinated fibers, but also show signs of axonal damage [20, 26, 41, 42].
Nerve ultrasound showed no nerve enlargement in all patients with an UPSS of < 3 points which in turn is contradictory to our previous understanding of demyelinating polyneuropathies:
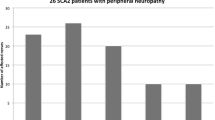
Generally speaking, nerve swelling can be seen on ultrasound, although with some individual differences. Inflammatory polyneuropathies, such as CIDP and atypical CIDPs, tend to show focal nerve swelling with some predominant fascicles [2, 3, 6]. Hereditary polyneuropathies, such as Charcot–Marie–Tooth Type 1 or storage diseases like leukodystrophies, adrenoleukodystrophies, xantochromatosis, or glucocerebrosidosis [15,16,17, 32, 43], mainly show ubiquitous nerve swelling, as would be expected in ARSACS patients per se. Our knowledge on nerve ultrasound as a biomarker in neurodegenerative diseases still lacks data. So far studies were able to identify that no nerve swelling is observed in other neurodegenerative diseases, spinocerebellar ataxia type 2 (SCA2), and CANVAS [44] or spinal muscular atrophy (SMA) [45]. However, as mentioned previously, these patients present with predominant axonal damage on NCS and ultrasound data in these cases coincide with ultrasound data from other, non-genetic, axonal neuropathies, making ARSACS in total, an exemption.
High-resolution ultrasound itself serves as an important biomarker to further stratify polyneuropathies as a non-invasive and fast diagnostic tool. We therefore suggest that in patients primaprily presenting with polyneuropathy, not ataxia, combined with primarily demyelinating peripheral neuropathy and no nerve swelling seen on ultrasound, further genetic testing for ARSACS should be strongly considered.
Early diagnosis prevents patients from vain diagnostic procedures and enables adequate counseling and symptomatic treatment. ARSACS patients who have been initially misdiagnosed as CMT support this assumption [19, 25].
A limitation of our study is its small sample size. If possible in this ultra-rare disorder, additional studies with larger patient numbers and extended electrophysiological examinations, nerve ultrasound, and correlation with histopathological data are needed to further evaluate the reported results. A correlation between neuropathy severity and ataxia severity has also been not assessed in this study design, but should be assessed in other prospective study designs.
Conclusion
In summary, this high-resolution ultrasound and electrophysiological study indicates a primarily demyelinating neuropathy pattern in ARSACS without enlargement of peripheral nerves. We therefore recommend genetic testing for mutations in the SACS gene in patients with demyelinating neuropathy who are not presenting enlargement of peripheral nerves.
Data availability statement
The data that support the findings of this study are available from the corresponding author upon request.
References
Telleman JA, Grimm A, Goedee S, Visser LH, Zaidman CM (2018) Nerve ultrasound in polyneuropathies. Muscle Nerve 57(5):716–728
Grimm A, Vittore D, Schubert V, Lipski C, Heiling B, Decard BF et al (2016) Ultrasound pattern sum score, homogeneity score and regional nerve enlargement index for differentiation of demyelinating inflammatory and hereditary neuropathies. Clin Neurophysiol 127(7):2618–2624
Zaidman CM, Harms MB, Pestronk A (2013) Ultrasound of inherited vs. acquired demyelinating polyneuropathies. J Neurol 260(12):3115–3121
Goedee SH, Brekelmans GJ, van den Berg LH, Visser LH (2015) Distinctive patterns of sonographic nerve enlargement in Charcot-Marie-Tooth type 1A and hereditary neuropathy with pressure palsies. Clin Neurophysiol 126(7):1413–1420
Schreiber S, Oldag A, Kornblum C, Kollewe K, Kropf S, Schoenfeld A et al (2013) Sonography of the median nerve in CMT1A, CMT2A, CMTX, and HNPP. Muscle Nerve 47(3):385–395
Padua L, Granata G, Sabatelli M, Inghilleri M, Lucchetta M, Luigetti M et al (2014) Heterogeneity of root and nerve ultrasound pattern in CIDP patients. Clin Neurophysiol 125(1):160–165
Grimm A, Decard BF, Axer H (2014) Ultrasonography of the peripheral nervous system in the early stage of Guillain-Barre syndrome. J Peripher Nerv Syst 19(3):234–241
Kerasnoudis A, Pitarokoili K, Behrendt V, Gold R, Yoon MS (2014) Multifocal motor neuropathy: correlation of nerve ultrasound, electrophysiological, and clinical findings. J Peripher Nerv Syst 19(2):165–174
Athanasopoulou IM, Rasenack M, Grimm C, Axer H, Sinnreich M, Decard BF et al (2016) Ultrasound of the nerves—an appropriate addition to nerve conduction studies to differentiate paraproteinemic neuropathies. J Neurol Sci 362:188–195
Lucchetta M, Padua L, Granata G, Luigetti M, Campagnolo M, Dalla Torre C et al (2015) Nerve ultrasound findings in neuropathy associated with anti-myelin-associated glycoprotein antibodies. Eur J Neurol 22(1):193–202
Grimm A, Decard BF, Bischof A, Axer H (2014) Ultrasound of the peripheral nerves in systemic vasculitic neuropathies. J Neurol Sci 347(1–2):44–49
Goedee HS, van der Pol WL, van Asseldonk JH, Vrancken A, Notermans NC, Visser LH et al (2016) Nerve sonography to detect peripheral nerve involvement in vasculitis syndromes. Neurol Clin Pract 6(4):293–303
Kerasnoudis A, Woitalla D, Gold R, Pitarokoili K, Yoon MS (2014) Sarcoid neuropathy: correlation of nerve ultrasound, electrophysiological and clinical findings. J Neurol Sci 347(1–2):129–136
Winter N, Dammeier N, Schaffer E, Bornemann A, Stahl JH, Herlan S et al (2019) Nerve ultrasonography as an additive tool to clinical examination and electrodiagnostics in sporadic mononeuritis—imaging is the key. Ultraschall Med 40(4):465–472
Rattay TW, Just J, Roben B, Hengel H, Schule R, Synofzik M et al (2018) Nerve ultrasound characterizes AMN polyneuropathy as inhomogeneous and focal hypertrophic. Orphanet J Rare Dis 13(1):194
Grimm A, Schaffer E, Just J, Schols L, Kehrer C, Bevot A et al (2016) Thickening of the peripheral nerves in metachromatic leukodystrophy. J Neurol Sci 368:399–401
Roeben B, Just J, Hengel H, Bender F, Poschl P, Synofzik M et al (2020) Multifocal, hypoechogenic nerve thickening in cerebrotendinous xanthomatosis. Clin Neurophysiol 131(8):1798–1803
Vermeer S, van de Warrenburg BP, Kamsteeg EJ, Brais B, Synofzik M. Arsacs (1993) In: Adam MP, Ardinger HH, Pagon RA, Wallace SE, Bean LJH, Stephens K et al (eds) GeneReviews((R)). University of Washington, Seattle Copyright © 1993–2020, Seattle. University of Washington, Seattle. GeneReviews is a registered trademark of the University of Washington, Seattle. All rights reserved
Synofzik M, Soehn AS, Gburek-Augustat J, Schicks J, Karle KN, Schule R et al (2013) Autosomal recessive spastic ataxia of charlevoix saguenay (ARSACS): expanding the genetic, clinical and imaging spectrum. Orphanet J Rare Dis 8:41
Baets J, Deconinck T, Smets K, Goossens D, Van den Bergh P, Dahan K et al (2010) Mutations in SACS cause atypical and late-onset forms of ARSACS. Neurology 75(13):1181–1188
Vermeer S, Meijer RP, Pijl BJ, Timmermans J, Cruysberg JR, Bos MM et al (2008) ARSACS in the Dutch population: a frequent cause of early-onset cerebellar ataxia. Neurogenetics 9(3):207–214
Prodi E, Grisoli M, Panzeri M, Minati L, Fattori F, Erbetta A et al (2013) Supratentorial and pontine MRI abnormalities characterize recessive spastic ataxia of Charlevoix-Saguenay. A comprehensive study of an Italian series. Eur J Neurol 20(1):138–146
Pilliod J, Moutton S, Lavie J, Maurat E, Hubert C, Bellance N et al (2015) New practical definitions for the diagnosis of autosomal recessive spastic ataxia of Charlevoix-Saguenay. Ann Neurol 78(6):871–886
Duquette A, Brais B, Bouchard JP, Mathieu J (2013) Clinical presentation and early evolution of spastic ataxia of Charlevoix-Saguenay. Mov Disord 28(14):2011–2014
Souza PVS, Bortholin T, Naylor FGM, Pinto W, Oliveira ASB (2018) Early-onset axonal Charcot–Marie–Tooth disease due to SACS mutation. Neuromuscul Disord 28(2):169–172
Vill K, Muller-Felber W, Glaser D, Kuhn M, Teusch V, Schreiber H et al (2018) SACS variants are a relevant cause of autosomal recessive hereditary motor and sensory neuropathy. Hum Genet 137(11–12):911–919
Schmitz-Hubsch T, du Montcel ST, Baliko L, Berciano J, Boesch S, Depondt C et al (2006) Scale for the assessment and rating of ataxia: development of a new clinical scale. Neurology 66(11):1717–1720
Linnemann C, du Montcel ST, Rakowicz M, Schmitz-Hubsch T, Szymanski S, Berciano J et al (2016) Peripheral neuropathy in spinocerebellar ataxia type 1, 2, 3, and 6. Cerebellum (London, England). 15(2):165–173
Preston DC, Shapiro BE (2013) Basic nerve conduction studies. In: Preston DC, Shapiro BE (eds) Electromyography and neuromuscular disorders. W.B. Saunders, London, pp 19–35
Joint Task Force of the E, the PNS (2010) European Federation of Neurological Societies/Peripheral Nerve Society Guideline on management of chronic inflammatory demyelinating polyradiculoneuropathy: report of a joint task force of the European Federation of Neurological Societies and the Peripheral Nerve Society–First Revision. J Peripher Nerv Syst 15(1):1–9
Grimm A, Axer H, Heiling B, Winter N (2018) Nerve ultrasound normal values—readjustment of the ultrasound pattern sum score UPSS. Clin Neurophysiol 129(7):1403–1409
Grimm AS, Schubert C, Grimm A, Stahl JH, Kupper H, Horber V et al (2020) Normative observational nerve ultrasound values in school-age children and adolescents and their application to hereditary neuropathies. Front Neurol 11:303
Berciano J, Garcia A, Infante J (2013) Peripheral nerve involvement in hereditary cerebellar and multisystem degenerative disorders. Handb Clin Neurol 115:907–932
Tzoulis C, Engelsen BA, Telstad W, Aasly J, Zeviani M, Winterthun S et al (2006) The spectrum of clinical disease caused by the A467T and W748S POLG mutations: a study of 26 cases. Brain 129(Pt 7):1685–1692
Bender F, Timmann D, van de Warrenburg BP, Adarmes-Gómez AD, Bender B, Thieme A et al (2021) Natural History of Polymerase Gamma-Related Ataxia. Mov Disord 36(11):2642–2652
Dupre M, Hermann R, Froment Tilikete C (2020) Update on cerebellar ataxia with neuropathy and bilateral vestibular areflexia syndrome (CANVAS). Cerebellum (London, England)
Morral JA, Davis AN, Qian J, Gelman BB, Koeppen AH (2010) Pathology and pathogenesis of sensory neuropathy in Friedreich’s ataxia. Acta Neuropathol 120(1):97–108
Crawford TO (1998) Ataxia telangiectasia. Semin Pediatr Neurol 5(4):287–294
Coutinho P, Barbot C (1993) Ataxia with Oculomotor Apraxia Type 1. In: Adam MP, Ardinger HH, Pagon RA, Wallace SE, Bean LJH, Stephens K et al (eds) GeneReviews((R)). University of Washington, Seattle Copyright © 1993–2020, Seattle. University of Washington, Seattle. GeneReviews is a registered trademark of the University of Washington, Seattle. All rights reserved
Moreira MC, Koenig M (1993) Ataxia with oculomotor apraxia type 2. In: Adam MP, Ardinger HH, Pagon RA, Wallace SE, Bean LJH, Stephens K et al (eds) GeneReviews((R)). University of Washington, Seattle Copyright © 1993–2020, Seattle. University of Washington, Seattle. GeneReviews is a registered trademark of the University of Washington, Seattle. All rights reserved
Takiyama Y (2006) Autosomal recessive spastic ataxia of Charlevoix-Saguenay. Neuropathology 26(4):368–375
Peyronnard JM, Charron L, Barbeau A (1979) The neuropathy of Charlevoix-Saguenay ataxia: an electrophysiological and pathological study. Can J Neurol Sci 6(2):199–203
Kupper H, Kaiser N, Winter N, Kehrer C, Groeschel S, Bevot A et al (2020) Enlargement of peripheral nerves in Krabbe disease: the diagnostic value of nerve ultrasound. Muscle Nerve 61(4):E24–E27
Leadbetter R, Weatherall M, Pelosi L (2019) Nerve ultrasound as a diagnostic tool for sensory neuronopathy in spinocerebellar ataxia syndrome. Clin Neurophysiol 130(4):568–572
Oudeman J, Eftimov F, Strijkers GJ, Schneiders JJ, Roosendaal SD, Engbersen MP et al (2020) Diagnostic accuracy of MRI and ultrasound in chronic immune-mediated neuropathies. Neurology 94(1):e62–e74
Acknowledgements
This project was supported by the Deutsche Forschungsgemeinschaft No 441409627, as part of the PROSPAX consortium under the frame of the European Joint Programme on Rare Diseases N° 825575 (to M.S. and D.T.). FB, LS, and MS are members of the European Reference Network for Rare Neurological Diseases—Project-No 739510.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
KK contributed to formal analysis (lead), writing—original draft (lead), and writing—review and editing (equal). SS, JHS, JW, NW, and LS were involved in writing—review and editing (equal). MS was responsible for conceptualization (supporting) and writing—review and editing (equal). FB was involved in writing—original draft (lead) and writing—review and editing (equal). AG was responsible for conceptualization (lead) and writing—review and editing (equal).
Corresponding author
Ethics declarations
Conflict of interest
All authors report no conflicts of interest in connection with this article.
Informed consent
Written consent was obtained by every patient prior to clinical and electrophysiological examination.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kneer, K., Straub, S., Wittlinger, J. et al. Neuropathy in ARSACS is demyelinating but without typical nerve enlargement in nerve ultrasound. J Neurol 271, 2494–2502 (2024). https://doi.org/10.1007/s00415-023-12159-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-023-12159-2