Abstract
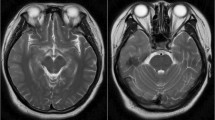
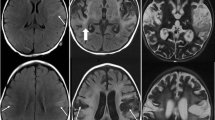
Discordant elevations of cerebrospinal fluid (CSF) human immunodeficiency virus (HIV) ribonucleic acid (RNA) in chronically treated patients known as ‘CSF escape’ may present as acute encephalitis. Infectious encephalitis caused by herpes simplex virus (HSV) and other neurotropic viruses have been identified as potential triggers of anti-N-methyl-D-aspartate receptor (NMDAR) encephalitis. Autoantibody-mediated encephalitis has been infrequently reported in HIV infected patients and may mimic HIV encephalitis. We report two adults infected with HIV presenting with encephalopathy and seizures. Case 1 had a monophasic encephalopathy with detection of NMDAR antibodies in the context of HIV CSF escape. There was a clinical response to immunotherapy and anti-retroviral therapy adjustment. Case 2 initially presented in non-convulsive status epilepticus associated with HIV CSF escape. He responded to treatment with anti-epileptic drugs and anti-retroviral therapy alteration, but had two further neurological relapses. NMDAR antibodies were detected during the relapses and a clinical response was observed following treatment with immunotherapy. Clinicians should consider autoimmune encephalitis in HIV infected patients presenting with encephalopathy and seizures, particularly in cases with concomitant HIV CSF escape.

Similar content being viewed by others
References
Peluso MJ, Ferretti F, Peterson J, Lee E, Fuchs D, Boschini A, Gisslén M, Angoff N, Price RW, Cinque P, Spudich S (2012) Cerebrospinal fluid HIV escape associated with progressive neurologic dysfunction in patients on antiretroviral therapy with well-controlled plasma viral load. AIDS 26(14):1765–1774
Mukerji SS, Misra V, Lorenz D, Cervantes-Arslanian AM, Lyons J, Chalkias S, Wurcel A, Burke D, Venna N, Morgello S, Koralnik IJ, Gabuzda D (2017) Temporal patterns and drug resistance in CSF viral escape among ART-experienced HIV-1 infected adults. J Acquir Immune Defic Syndr 75:246–255
Anguizola-Tamayo D, Bocos-Portillo J, Pardina-Viella L, Rodriguez-Sainz A, Vicente-Olabarria I, Martínez E, Gomez-Beldarrain M, Garcia-Monco JC (2019) Psychosis of dual origin in HIV infection: viral escape syndrome and autoimmune encephalitis. Neurol Clin Pract 9(2):178–180
Haneche F, Demeret S, Psimaras D, Katlama C, Pourcher V (2018) An anti-NMDA receptor encephalitis mimicking an HIV encephalitis. Clin Immunol 193:10–11
Armangue T, Spatola M, Vlagea A et al (2018) Frequency, symptoms, risk factors, and outcomes of autoimmune encephalitis after herpes simplex encephalitis: a prospective observational study and retrospective analysis. Lancet Neurol 17:760–772
Armangue T, Leypoldt F, Malaga I et al (2014) Herpes simplex virus encephalitis is a trigger of brain autoimmunity. Ann Neurol 75:317–323
Armangue T, Moris G, Cantarin-Extremera V et al (2015) Autoimmune post-herpes simplex encephalitis of adults and teenagers. Neurology 85:1736–1743
DeSena A, Graves D, Warnack W, Greenberg BM (2014) Herpes simplex encephalitis as a potential cause of anti–N-methyl-D-aspartate receptor antibody encephalitis: report of 2 cases. JAMA Neurol 71(3):344–346
Nosadini M, Mohammad SS, Corazza F, Ruga EM, Kothur K, Perilongo G, Frigo AC, Toldo I, Dale RC, Sartori S (2017) Herpes simplex virus-induced anti-N-methyl-d-aspartate receptor encephalitis: a systematic literature review with analysis of 43 cases. Dev Med Child Neurol 59:796–805
Salovin A, Glanzman J, Roslin K, Armangue T, Lynch DR, Panzer JA (2018) Anti-NMDA receptor encephalitis and nonencephalitic HSV-1 infection. Neurol Neuroimmunol Neurinflamm 5(4):e458
Prüss H, Finke C, Holtje M et al (2012) N-methyl-D-aspartate receptor antibodies in herpes simplex encephalitis. Ann Neurol 72:902–911
Schäbitz WR, Rogalewski A, Hagemeister C, Bien CG (2014) VZV brainstem encephalitis triggers NMDA receptor immunoreaction. Neurology 83:2309–2311
Linnoila JJ, Binnicker MJ, Majed M, Klein CJ, McKeon A (2016) CSF herpes virus and autoantibody profiles in the evaluation of encephalitis. Neurol Neuroimmunol Neuroinflamm 3(4):e245
Bundell C, Brunt SJ, Cysique LA, Brusch A, Brew BJ, Price P (2018) The high frequency of autoantibodies in HIV patients declines on antiretroviral therapy. Pathology 50(3):313–316
Graus F, Titulaer MJ, Balu R et al (2016) A clinical approach to diagnosis of autoimmune encephalitis. Lancet Neurol 15:391–404
Massabki PS, Accetturi C, Nishie IA, da Silva NP, Sato EI, Andrade LE (1997) Clinical implications of autoantibodies in HIV infection. AIDS 11(15):1845–1850
Zandi MS, Paterson RW, Ellul MA, Jacobson L et al (2015) Clinical relevance of serum antibodies to extracellular N-methyl-D-aspartate receptor epitopes. J Neurol Neurosurg Psychiatr 86:708–713
King JE, Eugenin EA, Hazleton JE, Morgello S, Berman JW (2010) Mechanisms of HIV-tat-induced phosphorylation of anti–N-methyl-D-aspartate receptor subunit 2A in human primary neurons: implications for NeuroAIDS pathogenesis. Am J Pathol 176:2819–2830
Author information
Authors and Affiliations
Contributions
PBM and AMCA contributed to the article conception and design. All authors contributed to the interpretation of the data. The first draft of the manuscript was written by PBM and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethical standards
The authors declare that they acted in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Moloney, P.B., Hutchinson, S., Heskin, J. et al. Possible N-methyl-D-aspartate receptor antibody-mediated encephalitis in the setting of HIV cerebrospinal fluid escape. J Neurol 267, 1348–1352 (2020). https://doi.org/10.1007/s00415-019-09693-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-019-09693-3