Abstract
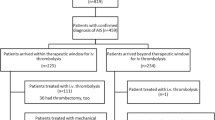
Patients with in-hospital strokes (IHS) may be eligible for recanalization therapies. The objective of this study is to compare outcomes in patients with IHS and community-onset strokes (COS) treated by recanalization therapy. We analysed data prospectively collected in consecutive patients treated by thrombolysis, thrombectomy, or both for cerebral ischemia at the Lille University Hospital. We compared four outcomes measures at 3 months in patients with IHS and COS: (1) modified Rankin scale (mRS) 0–1, (2) mRS 0–2, (3) death, and (4) symptomatic intracranial haemorrhage (ECASS 2 definition). Of 1209 patients, 64 (5.3%) had IHS, with an increasing proportion over time (p = 0.001). Their median onset-to-needle time was 128 min vs. 145 in COS (p < 0.001). They were more likely to have had a recent TIA [odds ratio (OR) 30.1; 95% confidence interval (CI) 11.5–78.7], to have been treated by vitamin K antagonist before (OR 4.2; 95% CI 1.4–12.0) and to undergo mechanical thrombectomy (45 vs. 10%, p < 0.001). They were less likely to have a pre-stroke mRS 0–1 (OR 0.22; 95% CI 0.09–0.50). After adjustment, IHS was not associated with any of the four outcome measures. Patients with IHS are treated 17 min earlier than patients with COS, but, taking into account that they were already in the hospital, delays are still too long. Their outcome does not differ from that of patients with COS, suggesting room for improvement if delays can be reduced. IHS being frequent, pre-specified pathways should be organised.



Similar content being viewed by others
References
Masjuan J, Simal P, Fuentes B et al (2008) In-hospital stroke treated with intravenous tissue plasminogen activator. Stroke 39:2614–2616
Saltman AP, Silver FL, Fang J et al (2015) Care and outcomes of patients with in-hospital stroke. JAMA Neurol 72:749–755
Blacker DJ (2003) In-hospital stroke. Lancet Neurol 2:741–746
Berkhemer OA, Fransen PSSS, Beumer D et al (2015) A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med 372:11–20
Campbell BCV, Mitchell PJ, Kleinig TJ et al (2015) Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med 372:1009–1018
Goyal M, Demchuk AM, Menon BK et al (2015) Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med 372:1019–1030
Saver JL, Goyal M, Bonafe A et al (2015) Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med 372:2285–2295
Jovin TG, Chamorro A, Cobo E et al (2015) Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med 372:2296–2306
Bracard S, Ducrocq X, Mas JL et al (2016) Mechanical thrombectomy after intravenous alteplase versus alteplase alone after stroke (THRACE): a randomised controlled trial. Lancet Neurol 15:1138–1147
Badhiwala JH, Nassiri F, Alhazzani W et al (2015) Endovascular thrombectomy for acute ischemic stroke: a meta-analysis. JAMA 314:1832–1843
Cordonnier C, Girot M, Dorp E et al (2000) Stroke units from scientific evidence to practice: the experience of the Lille stroke unit. Cerebrovasc Dis 10(Suppl 4):17–20
Decourcelle A, Moulin S, Dequatre-Ponchelle N et al (2017) Are the results of intravenous thrombolysis trials reproduced in clinical practice? Comparison of observed and expected outcomes with the stroke-thrombolytic predictive instrument (s-TPI). Rev Neurol (Paris) 173:381–387
Hacke W, Kaste M, Fieschi C et al (1998) Randomised double-blind placebo-controlled trial of thrombolytic therapy with intravenous alteplase in acute ischaemic stroke (ECASS II). Second European-Australasian Acute Stroke Study Investigators. Lancet 352:1245–1251
Hacke W, Kaste M, Bluhmki E et al (2008) Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med 359:1317–1329
The European Stroke Organisation (ESO) Executive Committee (2008) Guidelines for management of ischaemic stroke and transient ischaemic attack 2008. Cerebrovasc Dis 25:457–507. See update at : http://www.eso-stroke.org
Lyden P, Raman R, Liu L et al (2005) NIHSS training and certification using a new digital video disk is reliable. Stroke 36:2446–2449
Adams HP Jr, Bendixen BH, Kappelle LJ et al (1993) Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke 24:35–41
van Swieten JC, Koudstaal PJ, Visser MC et al (1988) Interobserver agreement for the assessment of handicap in stroke patients. Stroke 19:604–607
Glantz SA, Slinker BK (1990) Primer of applied regression and analysis of variance. McGraw Hill, New York
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Marc Ferrigno, Anais Hochart, Solène Moulin, Nelly Dequatre, Marie Bodenant, Hilde Hénon, Charlotte Cordonnier, and Didier Leys are investigators of ECASS4 (no honoraria). Didier Leys has been member of scientific advisory boards and symposia for Boehringer-Ingelheim (fees paid to ADRINORD). François Caparros and Amélie Decourcelle declare no conflict of interest.
Ethical standards
The registry was approved by the ethical committee of Lille in 2003 and the study classified as observational (CCPPRB, Comité consultatif de protection des personnes dans la recherche biomédicale).
Funding
INSERM U1171, University of Lille, Lille University Hospital, Adrinord.
Rights and permissions
About this article
Cite this article
Caparros, F., Ferrigno, M., Decourcelle, A. et al. In-hospital ischaemic stroke treated with intravenous thrombolysis or mechanical thrombectomy. J Neurol 264, 1804–1810 (2017). https://doi.org/10.1007/s00415-017-8570-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-017-8570-4