Abstract
Purpose
6-Shogaol, an active phenolic compound from ginger (Zingiber officinale), can inhibit the growth of a variety of human cancer cells. Nevertheless, its underlying molecular mechanisms in cervical cancer remain unclear. In this study, we systematically examine the inhibitory effect of 6-shogaol on cervical cancer in vitro and in vivo.
Methods
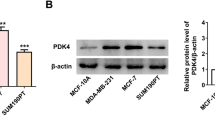
Cell proliferation was assessed by CCK8 assay and colony formation assay in HeLa and SiHa cells. We analyzed cell cycle and apoptosis through flow cytometry. GFP-LC3 puncta and transmission electron microscopy were used to observe autophagic bodies. Wound-healing assay and transwell assay were used for evaluating the migration of cells. Western blot was applied to detect protein expression levels.
Results
6-Shogaol could suppress cell proliferation and migration, cause cell cycle arrest in the G2/M phase in HeLa and SiHa cells. Moreover, 6-shogaol triggered the apoptosis process through the mitochondrial pathway by downregulating the expression levels of p-PI3K, p-Akt and p-mTOR. Further research indicated that the induction of apoptosis by 6-shogaol was remarkably decreased after the treatment of ROS scavenger and PI3K agonist. Additionally, 6-shogaol increased the number of LC3-positive puncta and autophagic bodies per cell in both HeLa and SiHa cells. Pretreatment of cells with Bafilomycin A1, an autophagy inhibitor, accelerated 6-shogaol mediated cell apoptosis, suggesting that induction of autophagy by 6-shogaol is suppressive to apoptosis. Furthermore, in vivo data revealed that 6-shogaol significantly inhibited tumor growth and cell proliferation in tumor tissues.
Conclusion
These findings suggested that 6-shogaol could be developed as a functional food ingredient, which is potentially used as therapeutic agents for patients with cervical cancer.








Similar content being viewed by others
Abbreviations
- PI3K:
-
Phosphatidylinositol 3-kinase
- AKT:
-
Protein kinase B
- mTOR:
-
Mammalian target of rapamycin
- CCK:
-
Cell-counting kit
- DMEM:
-
Dulbecco’s modified Eagle’s medium
- DMSO:
-
Dimethyl sulfoxide
- FBS:
-
Fetal bovine serum
- HRP:
-
Horseradish peroxidase
- PBS:
-
Phosphate-buffered saline
- Δψm:
-
Mitochondrial membrane potential
- PCNA:
-
Proliferating cell nuclear antigen
- EDTA:
-
Ethylene dinitrilotetraacetic acid
- NAC:
-
N-Acetyl-cysteine
- PARP:
-
Poly ADP-ribose polymerase
- IGF-1:
-
Insulin-like growth factors-1
- ROS:
-
Reactive oxygen species
- DCFH-DA:
-
2, 7-dichlorofluorescein diacetate
- CDK:
-
Cyclin-dependent kinases
- SDS-PAGE:
-
Sulfate-polyacrylamide gel electrophoresis
- Cdc:
-
Cell division cycle
- H&E:
-
Hematoxylin and eosin
References
Chrysostomou AC, Stylianou DC, Constantinidou A, Kostrikis LG (2018) Cervical cancer screening programs in Europe: the transition towards HPV vaccination and population-based HPV testing. Viruses. https://doi.org/10.3390/v10120729
Li H, Wu X, Cheng X (2016) Advances in diagnosis and treatment of metastatic cervical cancer. J Gynecol Oncol 27(4):e43. https://doi.org/10.3802/jgo.2016.27.e43
Mrklas KJ, MacDonald S, Shea-Budgell MA, Bedingfield N, Ganshorn H, Glaze S, Bill L, Healy B, Healy C, Guichon J, Colquhoun A, Bell C, Richardson R, Henderson R, Kellner J, Barnabe C, Bednarczyk RA, Letendre A, Nelson GS (2018) Barriers, supports, and effective interventions for uptake of human papillomavirus- and other vaccines within global and Canadian Indigenous peoples: a systematic review protocol. Syst Rev 7(1):40. https://doi.org/10.1186/s13643-018-0692-y
Ali BH, Blunden G, Tanira MO, Nemmar A (2008) Some phytochemical, pharmacological and toxicological properties of ginger (Zingiber officinale Roscoe): a review of recent research. Food Chem Toxicol 46(2):409–420. https://doi.org/10.1016/j.fct.2007.09.085
Lantz RC, Chen GJ, Sarihan M, Solyom AM, Jolad SD, Timmermann BN (2007) The effect of extracts from ginger rhizome on inflammatory mediator production. Phytomedicine 14(2–3):123–128. https://doi.org/10.1016/j.phymed.2006.03.003
Shukla Y, Singh M (2007) Cancer preventive properties of ginger: a brief review. Food Chem Toxicol 45(5):683–690. https://doi.org/10.1016/j.fct.2006.11.002
Ling H, Yang H, Tan SH, Chui WK, Chew EH (2010) 6-Shogaol, an active constituent of ginger, inhibits breast cancer cell invasion by reducing matrix metalloproteinase-9 expression via blockade of nuclear factor-kappaB activation. Br J Pharmacol 161(8):1763–1777. https://doi.org/10.1111/j.1476-5381.2010.00991.x
Jolad SD, Lantz RC, Solyom AM, Chen GJ, Bates RB, Timmermann BN (2004) Fresh organically grown ginger (Zingiber officinale): composition and effects on LPS-induced PGE2 production. Phytochemistry 65(13):1937–1954. https://doi.org/10.1016/j.phytochem.2004.06.008
Jolad SD, Lantz RC, Chen GJ, Bates RB, Timmermann BN (2005) Commercially processed dry ginger (Zingiber officinale): composition and effects on LPS-stimulated PGE2 production. Phytochemistry 66(13):1614–1635. https://doi.org/10.1016/j.phytochem.2005.05.007
Hung JY, Hsu YL, Li CT, Ko YC, Ni WC, Huang MS, Kuo PL (2009) 6-Shogaol, an active constituent of dietary ginger, induces autophagy by inhibiting the AKT/mTOR pathway in human non-small cell lung cancer A549 cells. J Agric Food Chem 57(20):9809–9816. https://doi.org/10.1021/jf902315e
Tan BS, Kang O, Mai CW, Tiong KH, Khoo AS, Pichika MR, Bradshaw TD, Leong CO (2013) 6-Shogaol inhibits breast and colon cancer cell proliferation through activation of peroxisomal proliferator activated receptor gamma (PPARgamma). Cancer Lett 336(1):127–139. https://doi.org/10.1016/j.canlet.2013.04.014
Liang T, He Y, Chang YH, Liu XT (2019) 6-shogaol a active component from ginger inhibits cell proliferation and induces apoptosis through inhibition of STAT-3 translocation in ovarian cancer cell lines (A2780). Biotechnol Bioproc E 24(3):560–567. https://doi.org/10.1007/s12257-018-0502-3
Li TY, Chiang BH (2017) 6-shogaol induces autophagic cell death then triggered apoptosis in colorectal adenocarcinoma HT-29 cells. Biomed Pharmacother 93:208–217. https://doi.org/10.1016/j.biopha.2017.06.038
Kondo Y, Kanzawa T, Sawaya R, Kondo S (2005) The role of autophagy in cancer development and response to therapy. Nat Rev Cancer 5(9):726–734. https://doi.org/10.1038/nrc1692
Levine B, Klionsky DJ (2004) Development by self-digestion: molecular mechanisms and biological functions of autophagy. Dev Cell 6(4):463–477. https://doi.org/10.1016/s1534-5807(04)00099-1
Codogno P, Mehrpour M, Proikas-Cezanne T (2011) Canonical and non-canonical autophagy: variations on a common theme of self-eating? Nat Rev Mol Cell Biol 13(1):7–12. https://doi.org/10.1038/nrm3249
Carew JS, Nawrocki ST, Kahue CN, Zhang H, Yang C, Chung L, Houghton JA, Huang P, Giles FJ, Cleveland JL (2007) Targeting autophagy augments the anticancer activity of the histone deacetylase inhibitor SAHA to overcome Bcr-Abl-mediated drug resistance. Blood 110(1):313–322. https://doi.org/10.1182/blood-2006-10-050260
Man S, Wang H, Zhou J, Lu Y, Su Y, Ma L (2019) Cardiac glycoside compound isolated from Helleborus thibetanus Franch displays potent toxicity against HeLa cervical carcinoma cells through ROS-independent autophagy. Chem Res Toxicol 32(12):2479–2487. https://doi.org/10.1021/acs.chemrestox.9b00318
Wang Q, Yan SP, Chu DX, Xie Y, Wang CF, Zhang JY, Li WC, Guo RX (2019) Silencing of Long Non-Coding RNA RP1-93H18.6 acts as a tumor suppressor in cervical cancer through the blockade of the PI3K/Akt axis. Mol Ther Nucleic Acids 19:304–317. https://doi.org/10.1016/j.omtn.2019.10.041
Weidner MS, Sigwart K (2000) The safety of a ginger extract in the rat. J Ethnopharmacol 73(3):513–520. https://doi.org/10.1016/s0378-8741(00)00340-8
Mahomoodally MF, Aumeeruddy MZ, Rengasamy KRR, Roshan S, Hammad S, Pandohee J, Hu X, Zengin G (2019) Ginger and its active compounds in cancer therapy: from folk uses to nano-therapeutic applications. Semin Cancer Biol. https://doi.org/10.1016/j.semcancer.2019.08.009
Schwartz GK, Shah MA (2005) Targeting the cell cycle: a new approach to cancer therapy. J Clin Oncol 23(36):9408–9421. https://doi.org/10.1200/JCO.2005.01.5594
Wu JJ, Omar HA, Lee YR, Teng YN, Chen PS, Chen YC, Huang HS, Lee KH, Hung JH (2015) 6-Shogaol induces cell cycle arrest and apoptosis in human hepatoma cells through pleiotropic mechanisms. Eur J Pharmacol 762:449–458. https://doi.org/10.1016/j.ejphar.2015.06.032
Ray A, Vasudevan S, Sengupta S (2015) 6-Shogaol inhibits breast cancer cells and stem cell-like spheroids by modulation of notch signaling pathway and induction of autophagic cell death. PLoS One 10(9):e0137614. https://doi.org/10.1371/journal.pone.0137614
Ishiguro K, Ando T, Watanabe O, Goto H (2008) Specific reaction of alpha, beta-unsaturated carbonyl compounds such as 6-shogaol with sulfhydryl groups in tubulin leading to microtubule damage. FEBS Lett 582(23–24):3531–3536. https://doi.org/10.1016/j.febslet.2008.09.027
Gan FF, Nagle AA, Ang X, Ho OH, Tan SH, Yang H, Chui WK, Chew EH (2011) Shogaols at proapoptotic concentrations induce G(2)/M arrest and aberrant mitotic cell death associated with tubulin aggregation. Apoptosis 16(8):856–867. https://doi.org/10.1007/s10495-011-0611-3
Park M, Chae HD, Yun J, Jung M, Kim YS, Kim SH, Han MH, Shin DY (2000) Constitutive activation of cyclin B1-associated cdc2 kinase overrides p53-mediated G2-M arrest. Cancer Res 60(3):542–545
Xu C, Wang X, Zhu Y, Dong X, Liu C, Zhang H, Liu L, Huang S, Chen L (2016) Rapamycin ameliorates cadmium-induced activation of MAPK pathway and neuronal apoptosis by preventing mitochondrial ROS inactivation of PP2A. Neuropharmacology 105:270–284. https://doi.org/10.1016/j.neuropharm.2016.01.030
Youle RJ, Strasser A (2008) The BCL-2 protein family: opposing activities that mediate cell death. Nat Rev Mol Cell Biol 9(1):47–59. https://doi.org/10.1038/nrm2308
Gong L, Tang Y, An R, Lin M, Chen L, Du J (2017) RTN1-C mediates cerebral ischemia/reperfusion injury via ER stress and mitochondria-associated apoptosis pathways. Cell Death Dis 8(10):e3080. https://doi.org/10.1038/cddis.2017.465
Maiuri MC, Zalckvar E, Kimchi A, Kroemer G (2007) Self-eating and self-killing: crosstalk between autophagy and apoptosis. Nat Rev Mol Cell Biol 8(9):741–752. https://doi.org/10.1038/nrm2239
Schumacker PT (2006) Reactive oxygen species in cancer cells: live by the sword, die by the sword. Cancer Cell 10(3):175–176. https://doi.org/10.1016/j.ccr.2006.08.015
Valko M, Leibfritz D, Moncol J, Cronin MT, Mazur M, Telser J (2007) Free radicals and antioxidants in normal physiological functions and human disease. Int J Biochem Cell Biol 39(1):44–84. https://doi.org/10.1016/j.biocel.2006.07.001
White E (2012) Deconvoluting the context-dependent role for autophagy in cancer. Nat Rev Cancer 12(6):401–410. https://doi.org/10.1038/nrc3262
Wang G, Zhang T, Sun W, Wang H, Yin F, Wang Z, Zuo D, Sun M, Zhou Z, Lin B, Xu J, Hua Y, Li H, Cai Z (2017) Arsenic sulfide induces apoptosis and autophagy through the activation of ROS/JNK and suppression of Akt/mTOR signaling pathways in osteosarcoma. Free Radic Biol Med 106:24–37. https://doi.org/10.1016/j.freeradbiomed.2017.02.015
Sui X, Chen R, Wang Z, Huang Z, Kong N, Zhang M, Han W, Lou F, Yang J, Zhang Q, Wang X, He C, Pan H (2013) Autophagy and chemotherapy resistance: a promising therapeutic target for cancer treatment. Cell Death Dis 4:e838. https://doi.org/10.1038/cddis.2013.350
Thiery JP, Acloque H, Huang RY, Nieto MA (2009) Epithelial-mesenchymal transitions in development and disease. Cell 139(5):871–890. https://doi.org/10.1016/j.cell.2009.11.007
Savagner P (2015) Epithelial-mesenchymal transitions: from cell plasticity to concept elasticity. Curr Top Dev Biol 112:273–300. https://doi.org/10.1016/bs.ctdb.2014.11.021
Javadian M, Gharibi T, Shekari N, Abdollahpour-Alitappeh M, Mohammadi A, Hossieni A, Mohammadi H, Kazemi T (2019) The role of microRNAs regulating the expression of matrix metalloproteinases (MMPs) in breast cancer development, progression, and metastasis. J Cell Physiol 234(5):5399–5412. https://doi.org/10.1002/jcp.27445
Cheng G, Gao F, Sun X, Bi H, Zhu Y (2016) Paris saponin VII suppresses osteosarcoma cell migration and invasion by inhibiting MMP2/9 production via the p38 MAPK signaling pathway. Mol Med Rep 14(4):3199–3205. https://doi.org/10.3892/mmr.2016.5663
Porta C, Paglino C, Mosca A (2014) Targeting PI3K/Akt/mTOR signaling in cancer. Front Oncol 4:64. https://doi.org/10.3389/fonc.2014.00064
Ciruelos Gil EM (2014) Targeting the PI3K/AKT/mTOR pathway in estrogen receptor-positive breast cancer. Cancer Treat Rev 40(7):862–871. https://doi.org/10.1016/j.ctrv.2014.03.004
Acknowledgements
This research was supported by State Key Laboratory of Bioactive Substance and Function of Natural Medicines, Institute of Materia Medica, Chinese Academy of Medical Sciences and Peking Union Medical College (Grant No. GTZK201810); Key laboratory of High-Incidence-Tumor Prevention & Treatment (Guangxi Medical University), Ministry of Education (Grant No. GKE2018-KF01); Guangdong Academic of Sciences Special Project of Science and Technology Development (Grant No. 2016GDASRC-0104); and Guangdong Key Laboratory of Animal Conservation and Resource Utilization (Grant No. GIABR-KF201901); The Beijing Engineering and Technology Research Center of Food Additives, Beijing Technology & Business University (BTBU); Open Project of Hubei Key Laboratory of Wudang Local Chinese Medicine Research (Hubei University of Medicine) (Grant No. WDCM2019012).
Author information
Authors and Affiliations
Contributions
XDP: Conceived, Designed, Data curation, Formal analysis, Writing-review & editing. ZLH: Data curation and Formal analysis. HLY: Data curation and Writing-review & editing. JSX: Writing-review & editing. LL: Data curation and Formal analysis. JZG: Data curation and Formal analysis. PZS: Data curation and Formal analysis. JHW: Data curation, Formal analysis and Writing-review and editing. LHJ: Conceived, Designed, Data curation, Formal analysis and Writing-review and editing; Undertake related research programs and fund this study. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflicts of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Pei, XD., He, ZL., Yao, HL. et al. 6-Shogaol from ginger shows anti-tumor effect in cervical carcinoma via PI3K/Akt/mTOR pathway. Eur J Nutr 60, 2781–2793 (2021). https://doi.org/10.1007/s00394-020-02440-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-020-02440-9