Abstract
Purpose
Three-dimensional (3D) vision technology has recently been validated for the improvement of surgical skills in a simulated setting. This study assessed the current evidence regarding the efficiency and potential advantages of 3D compared with two-dimensional (2D) laparoscopic rectal surgery for rectal cancer.
Methods
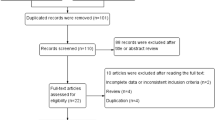
We comprehensively searched PubMed, EMBASE and the Cochrane Library and performed a systematic review and cumulative meta-analysis of all randomized controlled trials (RCTs) and non-randomized controlled trials (nRCTs) assessing the two approaches.
Results
Four trials including a total 331 cases were identified. The positive circumferential resection margins (CRMs) were significantly lower for the 3D group (P = 0.02). The operative time was significantly shorter in the 3D group than in the 2D group (P < 0.00001). There was less estimated blood loss (EBL) in the 3D group than in the 2D group (P = 0.02). Perioperative complication rates, conversion rate, harvested lymph nodes, first flatus, length of stay, pneumonia, wound infection, ileus, anastomotic fistula and urinary retention did not differ significantly between the two groups (P > 0.05).
Conclusions
In summary, 3D laparoscopic rectal surgery appears to have advantages over 2D laparoscopic rectal surgery in terms of positive CRM and operation time; however, it is not better than 2D laparoscopic rectal surgery in terms of the conversion rate and postoperative complications.




Similar content being viewed by others
References
Iversen LH, Norgaard M, Jepsen P, Jacobsen J, Christensen MM, Gandrup P, … Northern Danish Cancer Quality Assessment, G (2007) Trends in colorectal cancer survival in northern Denmark: 1985-2004. Color Dis 9:210–217
Pramateftakis MG, Kanellos D, Tekkis PP, Touroutoglou N, Kanellos I (2012) Rectal cancer: multimodal treatment approach. Int J Surg Oncol 2012:279341
Kang SB, Park JW, Jeong SY, Nam BH, Choi HS, Kim DW, … Oh JH (2010) Open versus laparoscopic surgery for mid or low rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): short-term outcomes of an open-label randomised controlled trial. Lancet Oncol 11:637–645
Denoya P, Wang H, Sands D, Nogueras J, Weiss E, Wexner SD (2010) Short-term outcomes of laparoscopic total mesorectal excision following neoadjuvant chemoradiotherapy. Surg Endosc 24:933–938
Sara S, Poncet G, Voirin D, Laverriere MH, Anglade D, Faucheron JL (2010) Can adequate lymphadenectomy be obtained by laparoscopic resection in rectal cancer? Results of a case-control study in 200 patients. J Gastrointest Surg 14:1244–1247
Leroy J, Jamali F, Forbes L, Smith M, Rubino F, Mutter D, Marescaux J (2004) Laparoscopic total mesorectal excision (TME) for rectal cancer surgery: long-term outcomes. Surg Endosc 18:281–289
Lusch A, Bucur PL, Menhadji AD, Okhunov Z, Liss MA, Perez-Lanzac A, … Landman J (2014) Evaluation of the impact of three-dimensional vision on laparoscopic performance. J Endourol 28:261–266
Storz P, Buess GF, Kunert W, Kirschniak A (2012) 3D HD versus 2D HD: surgical task efficiency in standardised phantom tasks. Surg Endosc 26:1454–1460
Curro G, La Malfa G, Caizzone A, Rampulla V, Navarra G (2015) Three-dimensional (3D) versus two-dimensional (2D) laparoscopic bariatric surgery: a single-surgeon prospective randomized comparative study. Obes Surg 25:2120–2124
Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, McQuay HJ (1996) Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trial 17:1–12
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25:603–605
Higgins J, Green S (2008) Cochrane handbook for systematic reviews of interventions. Cochrane Collaboration, John Wileyand Sons, New York
Hozo SP, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 5:13
Zhang Q, Liu Y, Zhang X, Wang Y, Yan X, Guo X (2017) Effect of flexible 3D laparoscopic surgery on rectal cancer after neoadjuvant chemoradiotherapy. Cancer Res Clin 29:112–115
Zeng Q, Lei F, Gao Z, Wang Y, Gao QK (2017) Case-matched study of short-term effects of 3D vs 2D laparoscopic radical resectionA of rectal cancer. World J Surg Oncol 15:178
Ji F, Fang X, Fei B (2017) Comparative study of 3D and 2D laparoscopic surgery for gastrointestinal tumors. Zhonghua Wei Chang Wai Ke Za Zhi 20:509–513
Curtis NJ, Conti JA, Dalton R, Rockall TA, Allison AS, Ockrim JB, … Francis NK (2019) 2D versus 3D laparoscopic total mesorectal excision: a developmental multicentre randomised controlled trial. Surg Endosc
Sutton AJ, Duval SJ, Tweedie RL, Abrams KR, Jones DR (2000) Empirical assessment of effect of publication bias on meta-analyses. BMJ 320:1574–1577
Cologne KG, Zehetner J, Liwanag L, Cash C, Senagore AJ, Lipham JC (2015) Three-dimensional laparoscopy: does improved visualization decrease the learning curve among trainees in advanced procedures? Surg Laparosc Endosc Percutan Tech 25:321–323
Ghedi A, Donarini E, Lamera R, Sgroi G, Turati L, Ercole C (2015) 3D vs 2D laparoscopic systems: development of a performance quantitative validation model. Conf Proc IEEE Eng Med Biol Soc 2015:6884–6887
Tung KL, Yang GP, Li MK (2015) Comparative study of 2-D and bichanneled 3-D laparoscopic images: is there a difference? Asian J Endosc Surg 8:275–280
Tao K, Liu X, Deng M, Shi W, Gao J (2016) Three-dimensional against 2-dimensional laparoscopic colectomy for right-sided colon cancer. Surg Laparosc Endosc Percutan Tech 26:324–327
Cicione A, Autorino R, Laguna MP, de Sio M, Micali S, Turna B, Sanchez-Salas R, Quattrone C, Dias E, Mota P, Bianchi G, Damano R, Rassweiler J, Lima E (2015) Three-dimensional technology facilitates surgical performance of novice laparoscopy surgeons: a quantitative assessment on a porcine kidney model. Urology 85:1252–1256
Nolan GJ, Howell S, Hewett P (2015) Impact of three-dimensional imaging in acquisition of laparoscopic skills in novice operators. J Laparoendosc Adv Surg Tech A 25:301–304
Velayutham V, Fuks D, Nomi T, Kawaguchi Y, Gayet B (2016) 3D visualization reduces operating time when compared to high-definition 2D in laparoscopic liver resection: a case-matched study. Surg Endosc 30:147–153
Jayne D, Pigazzi A, Marshall H, Croft J, Corrigan N, Copeland J, Quirke P, West N, Rautio T, Thomassen N, Tilney H, Gudgeon M, Bianchi PP, Edlin R, Hulme C, Brown J (2017) Effect of robotic-assisted vs conventional laparoscopic surgery on risk of conversion to open laparotomy among patients undergoing resection for rectal cancer: the ROLARR randomized clinical trial. JAMA 318:1569–1580
Strobel O, Buchler MW (2013) The problem of the poor control arm in surgical randomized controlled trials. Br J Surg 100:172–173
Liang JT, Cheng JC, Huang KC, Lai HS, Sun CT (2013) Comparison of tumor recurrence between laparoscopic total mesorectal excision with sphincter preservation and laparoscopic abdominoperineal resection for low rectal cancer. Surg Endosc 27:3452–3464
Rullier A, Laurent C, Capdepont M, Vendrely V, Bioulac-Sage P, Rullier E (2010) Impact of tumor response on survival after radiochemotherapy in locally advanced rectal carcinoma. Am J Surg Pathol 34:562–568
Arezzo A, Vettoretto N, Francis NK, Bonino MA, Curtis NJ, Amparore D, Arolfo S, Barberio M, Boni L, Brodie R, Bouvy N, Cassinotti E, Carus T, Checcucci E, Custers P, Diana M, Jansen M, Jaspers J, Marom G, Momose K, Müller-Stich BP, Nakajima K, Nickel F, Perretta S, Porpiglia F, Sánchez-Margallo F, Sánchez-Margallo JA, Schijven M, Silecchia G, Passera R, Mintz Y (2018) The use of 3D laparoscopic imaging systems in surgery: EAES consensus development conference. Surg Endosc
Liao H, Inomata T, Sakuma I, Dohi T (2010) 3-D augmented reality for MRI-guided surgery using integral videography autostereoscopic image overlay. IEEE Trans Biomed Eng 57:1476–1486
Curro G, Cogliandolo A, Bartolotta M, Navarra G (2016) Three-dimensional versus two-dimensional laparoscopic right hemicolectomy. J Laparoendosc Adv Surg Tech A 26:213–217
Funding
This work was supported by the National Basic Research Program of China (973 Program) (No. 2015CB554001, JW), the National Natural Science Foundation of China (No. 81472257, YL; No. 81502022, XW), the Natural Science Fund for Distinguished Young Scholars of Guangdong Province (No. 2016A030306002, YL), the Outstanding Young Scholars Supported by Special Program to Cultivate Top Experts in Guangdong Province (No. 2015TQ01R454, YL), the Natural Science Foundation of Guangdong Province (No. 2016A030310222, HY; No. 2018A0303130303, HY), the Science and Technology Program of Guangzhou (No. 2014Y2-00160, JW), the Fundamental Research Funds for the Central Universities (Sun Yat-sen University) (No. 16ykpy35, XW), the Program of Introducing Talents of Discipline to Universities, the National Key Clinical Discipline (2012) and Science and Technology project of Gansu province (No. 18JR3RA05, LF).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
Informed consent does not apply to the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, L., Gao, X., Guo, Y. et al. Comparison of three-dimensional versus two-dimensional laparoscopic surgery for rectal cancer: a meta-analysis. Int J Colorectal Dis 34, 1577–1583 (2019). https://doi.org/10.1007/s00384-019-03353-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-019-03353-8