Abstract
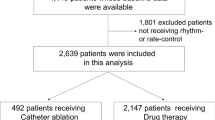
Management of atrial fibrillation (AF) with current rhythm-control therapy has an uncertain impact on outcomes. Among 3731 patients in the Fushimi AF Registry, a community-based prospective survey of AF patients in Fushimi-ku, Kyoto, we investigated the characteristics and outcomes in 478 patients receiving rhythm-control therapy (anti-arrhythmic drug and/or catheter ablation) alone, with 1279 patients receiving rate-control therapy (beta-blockers, calcium channel blockers, and digoxin) alone serving as a reference. The Rhythm-control group, 26% of which had prior catheter ablation, was younger (70.5 ± 10.8 vs. 74.3 ± 10.4 years, P < 0.001) with lower CHA2DS2-VASc score (2.71 ± 1.63 vs. 3.64 ± 1.62, P < 0.001) and received oral anticoagulants less frequently than the Rate-control group. During the median follow-up of 1107 days, the incidence of the composite of cardiac death and heart failure (HF) hospitalization was lower with rhythm control (hazard ratio (HR) 0.24, 95% confidence interval (CI) 0.14–0.36; P < 0.001), whereas that of ischemic stroke/systemic embolism was not significantly different (HR 0.64, 95% CI 0.35–1.10; P = 0.12), when compared to rate control. Propensity score-matching analysis as well as multivariate analysis further supported the relation of Rhythm-control group to the lower incidence of the composite of cardiac death and HF hospitalization. Rhythm-control therapy by anti-arrhythmic drug and/or catheter ablation in the contemporary clinical practice was associated with the lower incidence of the composite of cardiac death and HF hospitalization, as compared with rate-control therapy in a Japanese AF cohort. However, given the fundamental differences in baseline clinical characteristics between the rhythm- and Rate-control groups, the results cannot be generalizable.




Similar content being viewed by others
Change history
27 June 2018
In the original publication of the article, the data of Body mass index ≥ 25 (kg/m2)a is published incorrectly in Table 1. Since this is categorical variable, the data should have been expressed as a number (percentage), not as mean ± standard deviation. The corrected version of Table 1 is as below,
References
Wyse DG, Waldo AL, DiMarco JP, Domanski MJ, Rosenberg Y, Schron EB, Kellen JC, Greene HL, Mickel MC, Dalquist JE, Corley SD, Atrial Fibrillation Follow-up Investigation of Rhythm Management I (2002) A comparison of rate control and rhythm control in patients with atrial fibrillation. N Engl J Med 347:1825–1833
Van Gelder IC, Hagens VE, Bosker HA, Kingma JH, Kamp O, Kingma T, Said SA, Darmanata JI, Timmermans AJ, Tijssen JG, Crijns HJ, Rate Control versus Electrical Cardioversion for Persistent Atrial Fibrillation Study G (2002) A comparison of rate control and rhythm control in patients with recurrent persistent atrial fibrillation. N Engl J Med 347:1834–1840
Roy D, Talajic M, Nattel S, Wyse DG, Dorian P, Lee KL, Bourassa MG, Arnold JM, Buxton AE, Camm AJ, Connolly SJ, Dubuc M, Ducharme A, Guerra PG, Hohnloser SH, Lambert J, Le Heuzey JY, O’Hara G, Pedersen OD, Rouleau JL, Singh BN, Stevenson LW, Stevenson WG, Thibault B, Waldo AL, Atrial F, Congestive Heart Failure I (2008) Rhythm control versus rate control for atrial fibrillation and heart failure. N Engl J Med 358:2667–2677
Wilber DJ, Pappone C, Neuzil P, De Paola A, Marchlinski F, Natale A, Macle L, Daoud EG, Calkins H, Hall B, Reddy V, Augello G, Reynolds MR, Vinekar C, Liu CY, Berry SM, Berry DA, ThermoCool AFTI (2010) Comparison of antiarrhythmic drug therapy and radiofrequency catheter ablation in patients with paroxysmal atrial fibrillation: a randomized controlled trial. JAMA 303:333–340
Morillo CA, Verma A, Connolly SJ, Kuck KH, Nair GM, Champagne J, Sterns LD, Beresh H, Healey JS, Natale A, Investigators R (2014) Radiofrequency ablation vs antiarrhythmic drugs as first-line treatment of paroxysmal atrial fibrillation (RAAFT-2): a randomized trial. JAMA 311:692–700
Jones DG, Haldar SK, Hussain W, Sharma R, Francis DP, Rahman-Haley SL, McDonagh TA, Underwood SR, Markides V, Wong T (2013) A randomized trial to assess catheter ablation versus rate control in the management of persistent atrial fibrillation in heart failure. J Am Coll Cardiol 61:1894–1903
Hunter RJ, Berriman TJ, Diab I, Kamdar R, Richmond L, Baker V, Goromonzi F, Sawhney V, Duncan E, Page SP, Ullah W, Unsworth B, Mayet J, Dhinoja M, Earley MJ, Sporton S, Schilling RJ (2014) A randomized controlled trial of catheter ablation versus medical treatment of atrial fibrillation in heart failure (the CAMTAF trial). Circ Arrhythm Electrophysiol 7:31–38
Bunch TJ, Crandall BG, Weiss JP, May HT, Bair TL, Osborn JS, Anderson JL, Muhlestein JB, Horne BD, Lappe DL, Day JD (2011) Patients treated with catheter ablation for atrial fibrillation have long-term rates of death, stroke, and dementia similar to patients without atrial fibrillation. J Cardiovasc Electrophysiol 22:839–845
Chang CH, Lin JW, Chiu FC, Caffrey JL, Wu LC, Lai MS (2014) Effect of radiofrequency catheter ablation for atrial fibrillation on morbidity and mortality: a nationwide cohort study and propensity score analysis. Circ Arrhythm Electrophysiol 7:76–82
Friberg L, Tabrizi F, Englund A (2016) Catheter ablation for atrial fibrillation is associated with lower incidence of stroke and death: data from Swedish health registries. Eur Heart J 37:2478–2487
Chiang CE, Naditch-Brule L, Brette S, Silva-Cardoso J, Gamra H, Murin J, Zharinov OJ, Steg PG (2016) Atrial fibrillation management strategies in routine clinical practice: insights from the international RealiseAF survey. PLoS ONE 11:e0147536
Akao M, Chun YH, Wada H, Esato M, Hashimoto T, Abe M, Hasegawa K, Tsuji H, Furuke K, Fushimi AFRI (2013) Current status of clinical background of patients with atrial fibrillation in a community-based survey: the Fushimi AF Registry. J Cardiol 61:260–266
Akao M, Chun YH, Esato M, Abe M, Tsuji H, Wada H, Hasegawa K, Fushimi AFRI (2014) Inappropriate use of oral anticoagulants for patients with atrial fibrillation. Circ J 78:2166–2172
Takabayashi K, Hamatani Y, Yamashita Y, Takagi D, Unoki T, Ishii M, Iguchi M, Masunaga N, Ogawa H, Esato M, Chun YH, Tsuji H, Wada H, Hasegawa K, Abe M, Lip GY, Akao M (2015) Incidence of stroke or systemic embolism in paroxysmal versus sustained atrial fibrillation: the Fushimi Atrial Fibrillation Registry. Stroke 46:3354–3361
Suzuki S, Sagara K, Otsuka T, Matsuno S, Funada R, Uejima T, Oikawa Y, Yajima J, Koike A, Nagashima K, Kirigaya H, Sawada H, Aizawa T, Yamashita T (2012) A new scoring system for evaluating the risk of heart failure events in Japanese patients with atrial fibrillation. Am J Cardiol 110:678–682
Schnabel RB, Rienstra M, Sullivan LM, Sun JX, Moser CB, Levy D, Pencina MJ, Fontes JD, Magnani JW, McManus DD, Lubitz SA, Tadros TM, Wang TJ, Ellinor PT, Vasan RS, Benjamin EJ (2013) Risk assessment for incident heart failure in individuals with atrial fibrillation. Eur J Heart Fail 15:843–849
Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ (2010) Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest 137:263–272
Corley SD, Epstein AE, DiMarco JP, Domanski MJ, Geller N, Greene HL, Josephson RA, Kellen JC, Klein RC, Krahn AD, Mickel M, Mitchell LB, Nelson JD, Rosenberg Y, Schron E, Shemanski L, Waldo AL, Wyse DG, Investigators A (2004) Relationships between sinus rhythm, treatment, and survival in the Atrial Fibrillation Follow-Up Investigation of Rhythm Management (AFFIRM) Study. Circulation 109:1509–1513
Tsadok MA, Jackevicius CA, Essebag V, Eisenberg MJ, Rahme E, Humphries KH, Tu JV, Behlouli H, Pilote L (2012) Rhythm versus rate control therapy and subsequent stroke or transient ischemic attack in patients with atrial fibrillation. Circulation 126:2680–2687
Ionescu-Ittu R, Abrahamowicz M, Jackevicius CA, Essebag V, Eisenberg MJ, Wynant W, Richard H, Pilote L (2012) Comparative effectiveness of rhythm control vs rate control drug treatment effect on mortality in patients with atrial fibrillation. Arch Intern Med 172:997–1004
Zhang YY, Qiu C, Davis PJ, Jhaveri M, Prystowsky EN, Kowey P, Weintraub WS (2013) Predictors of progression of recently diagnosed atrial fibrillation in REgistry on Cardiac Rhythm DisORDers Assessing the Control of Atrial Fibrillation (RecordAF)-United States cohort. Am J Cardiol 112:79–84
Lopes RD, Rordorf R, De Ferrari GM, Leonardi S, Thomas L, Wojdyla DM, Ridefelt P, Lawrence JH, De Caterina R, Vinereanu D, Hanna M, Flaker G, Al-Khatib SM, Hohnloser SH, Alexander JH, Granger CB, Wallentin L, Committees A and Investigators (2018) Digoxin and mortality in patients with atrial fibrillation. J Am Coll Cardiol 71:1063–1074
January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC Jr, Conti JB, Ellinor PT, Ezekowitz MD, Field ME, Murray KT, Sacco RL, Stevenson WG, Tchou PJ, Tracy CM, Yancy CW, Members AATF (2014) 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation 130:e199–e267
Miyazaki S, Kuwahara T, Kobori A, Takahashi Y, Takei A, Sato A, Isobe M, Takahashi A (2009) Pharmacological cardioversion preceding left atrial ablation: bepridil predicts the clinical outcome following ablation in patients with persistent atrial fibrillation. Europace 11:1620–1623
Kondo T, Miake J, Kato M, Ogura K, Iitsuka K, Yamamoto K (2016) Impact of postprocedural antiarrhythmic drug therapy with bepridil on maintaining sinus rhythm after catheter ablation for persistent atrial fibrillation. J Cardiol 68:229–235
Marrouche NF, Brachmann J, Andresen D, Siebels J, Boersma L, Jordaens L, Merkely B, Pokushalov E, Sanders P, Proff J, Schunkert H, Christ H, Vogt J, Bansch D, Investigators C-A (2018) Catheter ablation for atrial fibrillation with heart failure. N Engl J Med 378:417–427
Ghanbari H, Baser K, Jongnarangsin K, Chugh A, Nallamothu BK, Gillespie BW, Baser HD, Suwanagool A, Crawford T, Latchamsetty R, Good E, Pelosi F Jr, Bogun F, Morady F, Oral H (2014) Mortality and cerebrovascular events after radiofrequency catheter ablation of atrial fibrillation. Heart Rhythm 11:1503–1511
Darrat YH, Shah J, Elayi CS, Morales GX, Naditch-Brule L, Brette S, Taniou C, Kowey PR, Schwartz PJ (2017) Regional lack of consistency in the management of atrial fibrillation (from the RECORD-AF Trial). Am J Cardiol 119:47–51
Bassand JP, Accetta G, Camm AJ, Cools F, Fitzmaurice DA, Fox KA, Goldhaber SZ, Goto S, Haas S, Hacke W, Kayani G, Mantovani LG, Misselwitz F, Ten Cate H, Turpie AG, Verheugt FW, Kakkar AK, Investigators G-A (2016) Two-year outcomes of patients with newly diagnosed atrial fibrillation: results from GARFIELD-AF. Eur Heart J 37:2882–2889
Acknowledgements
M. Akao had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. We sincerely appreciate the efforts of the clinical research coordinators (T. Shinagawa, M. Mitamura, M. Fukahori, M. Kimura, M. Fukuyama, and C. Kamata).
The following is a list of the institutions participating in the registry.
Chief investigator: Akao M (National Hospital Organization Kyoto Medical Center).
Vice-chief investigator: Esato M (Ijinkai Takeda General Hospital).
Steering committee: Abe M (National Hospital Organization Kyoto Medical Center), Tsuji H (Tsuji Clinic), and Furuke K (Furuke Clinic).
Statistical analysis: Wada H (National Hospital Organization Kyoto Medical Center).
Coordinator: Ogawa T (Ogawa Medical Office), Tasato H (Tasato Clinic), Taniguchi Y (Taniguchi Clinic), Nishikawa M (Nishikawa Clinic), Furukawa K (Furukawa Medical Clinic), Kawai C, Hashimoto T, Kanda M (Ijinkai Takeda General Hospital), Tsukahara T, Fukuda S, Nakamura M, Ohtani R, Ito T, and Hasegawa K (National Hospital Organization Kyoto Medical Center).
Clinical event committee: Kawabata Y, Yasuda K, and Kameyama K (National Hospital Organization Kyoto Medical Center).
Participating institutions: Department of Cardiology, National Hospital Organization Kyoto Medical Center (Akao M, Abe M, Ogawa H, Masunaga N, Iguchi M, Ishii M, An Y, Unoki T, Niki S, Takabayashi K, Hamatani Y, Yamashita Y, Takagi D, Tezuka Y, Doi K, Aono Y, Ikeda S, Osakada G, Nakashima Y, Kanasaki M, Nakano T, Funatsu J, Nishio M, and Takenaka Y); Department of Arrhythmia, Ijinkai Takeda General Hospital (Chun YH, Esato M, Kida Y, Nishina N); Koujinkai Oshima Hospital (Terada K); Division of Translational Research, National Hospital Organization Kyoto Medical Center (Hasegawa K, Wada H); Kanai Hospital (Nishio M, Kamiya Y, Abe M, Ishii M); Tsuji clinic (Tsuji H); Furukawa Medical Clinic (Furukawa K); Nishikawa Clinic (Nishikawa M); Taniguchi Clinic (Taniguchi Y); Gushiken Clinic (Gushiken T); Kyoto Rehabilitation Hospital (Hirata Y); Yoda Clinic (Yoda J); Tasato Clinic (Tasato H); Ogawa Medical Office (Ogawa T); Mukaijima Hospital (Wakatsuki Y, Yahata M, Higashitani N); Itoh Hemodialysis Clinic (Itoh H); Itoh Clinic (Itoh H, Ohmori Y); Ryokuhoukai Tsuji Clinic (Tsuji K); Kitamura Clinic (Kitamura S); Izumikawa Clinic (Izumikawa F); Hirota Clinic (Hirota N); Kyomachi-Oota Clinic (Oota K); Kouseikai Rehabilitation Clinic (Kou K); Inariyama Takeda Hospital (Tanaka T, Iguchi M); Matsushita Clinic (Matsushita N); Kitani Clinic (Kitani K); Kimura Clinic (Kimura F); Hayashi Clinic (Hayashi S); Handa Clinic (Handa S); Soseikai General Hospital (Hasegawa S, Kono T, Otsuka K, Soyama A, Okamoto J, Nakai Y); Asamoto Clinic (Asamoto H); Sugano Clinic (Tanaka H, Murata T); Fushimi Momoyama General Hospital (Kayawake S, Kinoshita Y); Furuke Clinic (Furuke K); Kanehisa Clinic (Asano N); Tahara Clinic (Tahara K); Matsumoto Medical Office (Matsumoto K); Kuroda Clinic (Kuroda O); Ochiai Clinic (Ochiai K, Ochiai J); Fujii Clinic (Fujii M); Kurihara Clinic (Kurihara M); Kuzuyama Clinic (Ito A); Kenkokai Fushimi Clinic (Totsuzaki S); Nakayama Orthopedic Clinic (Nakayama H); Department of Cardiovascular Medicine, Ijinkai Takeda General Hospital (Kawai C, Hashimoto T, Kakio T, Watanabe C, Takeda S, Sasaki Y, Shirasawa K, Beppu K, Inoue T, Shirasaka A, Doi T); Tatsumi Clinic (Ueda T); Oishi Clinic (Oishi M); Koizumi Clinic (Kasahara A); Kishida Clinic (Kishida Su, Kishida Sa); Shibata Clinic (Shibata M); Shimizu Clinic (Shimizu J); Shirasu Clinic (Shirasu M); Fujinokai Clinic (Tateishi S); Tsukuda Clinic (Tsukuda N); Shinseikai Tsuji Clinic (Tsuji K); Nishi Clinic (Nishi T); Nishimura Clinic (Nishimura S); Haba Clinic (Haba T); Higashimae Clinic (Higashimae R); Fujimori Clinic (Fujimori C); Hotta Clinic (Hotta T); Matsui Clinic (Matsui H, Matsui H); Shadan Matsumoto Clinic (Matsumoto H); Maruo Clinic (Maruo N); Misu Clinic (Mikami M); Mekata Clinic (Mekata H); Mori Pediatric Clinic (Mori H); Wakabayashi Clinic (Wakabayashi M); Nakatsugawa Clinic (Sasaki Z); Shiseikai Nishimura Clinic (Nishimura S); Yuge Eye Clinic (Yuge K); Gokita Hospital (Haruta M); Soseikai Clinic (Tsuda E); Toujinkai Hospital (Nishimura M); Kouno Clinic (Kouno T, Kouno Y); Matsumura Clinic (Matsumura S); Fujita Clinic (Fujita A); Takayasu Clinic (Takayasu F, Takayasu S); Yano Clinic (Yano Y), Niki Clinic (Niki S); Hasegawa Meiando Clinic (Hasegawa S); Watanabe Medical Clinic (Watanabe T).
Funding
The Fushimi AF Registry is supported by research funding from Boehringer Ingelheim, Bayer Healthcare, Pfizer, Bristol-Myers Squibb, Astellas Pharma, AstraZeneca, Daiichi Sankyo, Novartis Pharma, MSD, Sanofi-Aventis and Takeda Pharmaceutical. The sponsors had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript. This research is partially supported by the Practical Research Project for Lifestyle-related Diseases including Cardiovascular Diseases and Diabetes Mellitus from Japan Agency for Medical Research and Development, AMED (18ek0210082h0002, 18ek0210056h0003).
Author information
Authors and Affiliations
Contributions
YA analyzed the data and wrote the paper. YH and GL helped data analysis and interpretation. ME, YC, MI, MI, NM, HT, HW, KH, HO and M. Abe are executive members of the organizing committee of the Fushimi AF Registry. M. Akao is a principal investigator of the Fushimi AF Registry, and the corresponding author of this paper.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Akao received lecture fees from Pfizer, Bristol-Myers Squibb, Boehringer Ingelheim, Bayer Healthcare and Daiichi Sankyo. Dr Lip has served as a consultant for Bayer, Merck, Sanofi, BMS/Pfizer, Daiichi Sankyo, Biotronik, Medtronic, Portola and Boehringer Ingelheim and has been on the speakers bureau for Bayer, BMS/Pfizer, Boehringer Ingelheim, Daiichi Sankyo, Medtronic. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Additional information
Gregory Y. H. Lip and Masaharu Akao are joint senior authors.
Electronic supplementary material
Below is the link to the electronic supplementary material.

380_2018_1194_MOESM1_ESM.jpg
Supplementary material 1 (JPEG 273 kb) Figure S1 Unadjusted Kaplan–Meier curves for the incidence of cardiac death/HF hospitalization between those with and without previous catheter ablation among the Rhythm-control group. CA = catheter ablation

380_2018_1194_MOESM2_ESM.jpg
Supplementary material 2 (JPEG 440 kb) Figure S2 Unadjusted hazard ratio for cardiac death/HF hospitalization, according to major subgroups. Forest plots show hazard ratio with error bars indicating 95% confidence interval. BMI = body mass index. Anemia was defined as the hemoglobin level < 11 g/dl. Renal dysfunction was defined as the estimated glomerular filtration rate < 60 ml/min/m2
Rights and permissions
About this article
Cite this article
An, Y., Esato, M., Ishii, M. et al. Clinical characteristics and cardiovascular outcomes in patients with atrial fibrillation receiving rhythm-control therapy: the Fushimi AF Registry. Heart Vessels 33, 1534–1546 (2018). https://doi.org/10.1007/s00380-018-1194-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-018-1194-5