Abstract
Purpose
To describe the prevalence and predictors of nocturnal polyuria (NP) in women with overactive bladder syndrome (OAB).
Methods
Between July 2009 and January 2018, women with OAB were enrolled. NP was defined when the nocturnal polyuria index (NPI) (nighttime voided volume over 24-h voided volume) was > 33% (NPI33) in women ≥ 65 years-old and > 20% (NPI20) in women < 65 years old. Repeated analysis was also performed for NP defined by the NPI33 definition at all ages.
Results
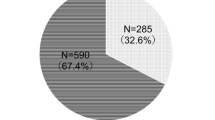
A total of 1071 women with OAB were analyzed. The overall prevalence of NP was 30% (319/1071), with the highest prevalence in women in the perimenopausal period (46–50 years old), while NP was diagnosed by age-dependent NPI. The overall prevalence of NP was 12% (128/1071), with an increasing trend with increasing age, while NP was diagnosed by the NPI33 definition only. Daytime frequency and nocturia episodes were both predictors for NP in both definitions. Receiver operating characteristic curve analysis revealed that more than 5 nocturia episodes noted in the 3-day bladder diary were an optimal cutoff value to predict nocturnal polyuria [(sensitivity = 85.6%, specificity = 61.0%; area = 0.80, 95% CI 0.77–0.82) and (sensitivity = 88.3%, specificity = 65.9%; area = 0.83, 95% CI 0.80–0.85), respectively, in the two definitions].
Conclusions
NP is common in women with OAB, especially in women with more than 5 nocturia episodes in their 3-day bladder diaries, and adjuvant therapy for better treatment efficacy is needed.




Similar content being viewed by others
Availability of data and material
The datasets analyzed during the study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
References
Hsiao SM, Lin HH (2018) Medical treatment of female overactive bladder syndrome and treatment-related effects. J Formos Med Assoc 117:871–878. https://doi.org/10.1016/j.jfma.2018.01.011
Stewart WF, Van Rooyen JB, Cundiff GW et al (2003) Prevalence and burden of overactive bladder in the United States. World J Urol 20:327–336. https://doi.org/10.1007/s00345-002-0301-4
Haylen BT, de Ridder D, Freeman RM et al (2010) An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J 21:5–26. https://doi.org/10.1002/nau.20798
Hashim H, Blanker MH, Drake MJ et al (2019) International Continence Society (ICS) report on the terminology for nocturia and nocturnal lower urinary tract function. Neurourol Urodyn 38:499–508. https://doi.org/10.1002/nau.23917
Hetta J (1999) The impact of sleep deprivation caused by nocturia. BJU Int 84(Suppl 1):27–28. https://doi.org/10.1046/j.1464-410x.84.s1.3.x
Irwin DE, Milsom I, Hunskaar S et al (2006) Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol 50:1306–1314. https://doi.org/10.1016/j.eururo.2006.09.019
Tsai KH, Hsiao SM, Lin HH (2017) Tolterodine treatment of women with overactive bladder syndrome: comparison of night-time and daytime dosing for nocturia. J Obstet Gynaecol Res 43:1719–1725
Hofmeester I, Kollen BJ, Steffens MG et al (2015) Impact of the International Continence Society (ICS) report on the standardisation of terminology in nocturia on the quality of reports on nocturia and nocturnal polyuria: a systematic review. BJU Int 115:520–536. https://doi.org/10.1111/bju.12753
Lightner DJ, Gomelsky A, Souter L et al (2019) Diagnosis and treatment of overactive bladder (non-neurogenic) in adults: AUA/SUFU guideline amendment 2019. J Urol 202(3):558–563. https://doi.org/10.1097/JU.0000000000000309
Uebersax JS, Wyman JF, Shumaker SA, McClish DK, Fantl JA (1995) Short forms to assess life quality and symptom distress for urinary incontinence in women: the Incontinence Impact Questionnaire and the Urogenital Distress Inventory. Continence program for women research group. Neurourol Urodyn 14:131–139. https://doi.org/10.1002/nau.1930140206
Homma Y, Yoshida M, Seki N et al (2006) Symptom assessment tool for overactive bladder syndrome–overactive bladder symptom score. Urology 68:318–323. https://doi.org/10.1016/j.urology.2006.02.042
Nixon A, Colman S, Sabounjian L et al (2005) A validated patient reported measure of urinary urgency severity in overactive bladder for use in clinical trials. J Urol 174:604–607. https://doi.org/10.1097/01.ju.0000165461.38088.7b
Sand PKOD (ed) (1995) Urodynamics and the evaluation of female incontinence: a practical guide. Springer-Verlag, London
Wu WY, Sheu BC, Lin HH (2006) Comparison of 20-minute pad test versus 1-hour pad test in women with stress urinary incontinence. Urology 68:764–768. https://doi.org/10.1016/j.urology.2006.04.018
Wu WY, Sheu BC, Lin HH (2008) Twenty-minute pad test: comparison of infusion of 250 ml of water with strong-desire amount in the bladder in women with stress urinary incontinence. Eur J Obstet Gynecol Reprod Biol 136:121–125. https://doi.org/10.1016/j.ejogrb.2007.02.030
Voelker R (2017) Nocturnal polyuria drug approved. JAMA 317:1518. https://doi.org/10.1001/jama.2017.3344
Weiss JP, Blaivas JG (2002) Nocturnal polyuria versus overactive bladder in nocturia. Urology 60(5 suppl 1):28–32. https://doi.org/10.1016/s0090-4295(02)01789-2
Lopes Mendes AL, Decalf V, Denys MA, Tubaro A, Everaert K (2017) The impact of nocturnal polyuria in older people with nocturnal LUTS. Minerva Urol Nefrol 69:377–383. https://doi.org/10.23736/S0393-2249.16.02745-4
Niimi A, Suzuki M, Yamaguchi Y et al (2016) Sleep apnea and circadian extracellular fluid change as independent factors for nocturnal polyuria. J Urol 196:1183–1189. https://doi.org/10.1016/j.juro.2016.04.060
McKeigue PM, Reynard JM (2000) Relation of nocturnal polyuria of the elderly to essential hypertension. Lancet 355:486–488. https://doi.org/10.1016/S0140-6736(00)82039-5
Yokoyama O, Nishizawa O, Homma Y et al (2017) Nocturnal polyuria and hypertension in patients with lifestyle related diseases and overactive bladder. J Urol 197:423–431. https://doi.org/10.1016/j.juro.2016.08.087
Hofmeester I, Kollen BJ, Steffens MG et al (2014) The association between nocturia and nocturnal polyuria in clinical and epidemiological studies: a systematic review and meta-analyses. J Urol 191:1028–1033. https://doi.org/10.1016/j.juro.2013.10.100
van Kerrebroeck P, Abrams P, Chaikin D et al (2002) The standardisation of terminology in nocturia: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn 21:179–183. https://doi.org/10.1002/nau.10053
Olesen TK, Denys MA, Vande Walle J, Everaert K (2018) Systematic review of proposed definitions of nocturnal polyuria and population-based evidence of their diagnostic accuracy. Acta Clin Belg 73:268–274. https://doi.org/10.1080/17843286.2018.1427821
Drake NL, Flynn MK, Romero AA, Weidner AC, Amundsen CL (2005) Nocturnal polyuria in women with overactive bladder symptoms and nocturia. Am J Obstet Gynecol 192:1682–1686. https://doi.org/10.1016/j.ajog.2004.11.033
Hsieh CH, Chang WC, Hsu MI et al (2010) Risk factors of urinary frequency among women aged 60 and older in Taiwan. Taiwan J Obstet Gynecol 49:260–265. https://doi.org/10.1016/S1028-4559(10)60058-7
Asplund R, Aberg HE (2005) Development of nocturia in relation to health, age and the menopause. Maturitas 51:358–362. https://doi.org/10.1016/j.maturitas.2004.09.001
Kurtzman JT, Bergman AM, Weiss JP (2016) Nocturia in women. Curr Opin Urol 26:315–320. https://doi.org/10.1016/10.1097/MOU.0000000000000287
Monaghan TF, Weiss JP, Everaert K, Wein AJ (2021) Pharmacologic management of nocturnal polyuria: a contemporary assessment of efficacy, safety, and progress toward individualized treatment. Ther Adv Urol 13:1756287220988438. https://doi.org/10.1177/1756287220988438
Monaghan TF, Suss NR, Epstein MR et al (2018) Differential nocturnal diuresis rates among patients with and without nocturnal polyuria syndrome. Eur Urol Focus. https://doi.org/10.1016/j.euf.2018.10.015
Hsiao SM, Wu PC, Chang TC, Chen CH, Lin HH (2019) Urodynamic and bladder diary factors predict overactive bladder-wet in women: a comparison with overactive bladder-dry. Int Neurourol J 23:69–74. https://doi.org/10.5213/inj.1836212.106
Barakat B, Franke K, May M, Gauger U, Vo¨geli TA (2021) Efficacy and safety of desmopressin on frequency and urgency in female patients with overactive bladder and nocturia, current clinical features and outcomes: a systematic review. Asian J Urol. https://doi.org/10.1016/j.ajur.2021.05.005
Smith AL, Wein AJ (2011) Outcomes of pharmacological management of nocturia with non-antidiuretic agents: does statistically significant equal clinically significant? BJU Int 107:1550–1554. https://doi.org/10.1111/j.1464-410X.2010.09972.x
Acknowledgements
None.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
P-CW: manuscript writing. S-MH: data collection and data analysis. H-HL: protocol development and manuscript editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical approval
This study received approval from the Research Ethics Committee of the National Taiwan University Hospital (ID No. 201810091RIND).
Consent to participate
Not applicable for the retrospective study.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wu, PC., Hsiao, SM. & Lin, HH. Prevalence and predictors of nocturnal polyuria in females with overactive bladder syndrome. World J Urol 40, 519–527 (2022). https://doi.org/10.1007/s00345-021-03865-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-021-03865-5