Abstract
Purpose
To evaluate the association between prostate-specific antigen (PSA) response and progression-free and overall survival in men with metastatic castration-resistant prostate cancer (mCRPC) treated with cabazitaxel.
Methods
Men with mCRPC receiving cabazitaxel (25 mg/m2, every 3 weeks) plus oral prednis(ol)one (10 mg/day) were enrolled in the non-interventional, prospective QoLiTime study. Main outcome measures were progression-free survival and overall survival, in all patients and in those who showed a ≥ 50 or a ≥ 30% decrease in PSA relative to baseline after four cycles of cabazitaxel, as well as quality-of-life parameters.
Results
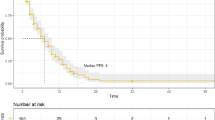
Of the 527 men (median age 72 years), 266 received ≥ 4 cycles of cabazitaxel and had PSA response data. After four cycles, 34.6% of men achieved a PSA decrease ≥ 50% and 49.6% a decrease ≥ 30%. Median progression-free survival was 7.7 (95% CI 6.2, 9.5) months, and overall survival was 19.5 (95% CI 16.0, 30.9) months, corresponding to 1-year event rates of 39.4 and 78.8%, respectively. Median progression-free survival was longer in PSA responders versus non-responders (15.7 vs 5.5 months at 50% cut-off; 15.7 vs 5.3 months for 30% cut-off; both P < 0.0001). Overall survival (50% cut-off) was 23.3 months in responders and 16.0 months in non-responders (P = 0.068); corresponding data at the 30% cut-off are 21.7 and 16.0 months (P = 0.057). Overall, 55.4% of men experienced ≥ 1 adverse event, 59.6% of whom had a serious adverse event.
Conclusion
PSA response after four cycles of cabazitaxel is associated with improved progression-free survival in men with mCRPC treated with cabazitaxel plus prednis(ol)one.


Similar content being viewed by others
References
Tannock IF, de Wit R, Berry WR et al (2004) Docetaxel plus prednisone or mitoxantrone plus prednisone for advanced prostate cancer. N Engl J Med 351:1502–1512
Attard G, Greystoke A, Kaye S et al (2006) Update on tubulin-binding agents. Pathol Biol (Paris) 54:72–84
Mita AC, Denis LJ, Rowinsky EK et al (2009) Phase I and pharmacokinetic study of XRP6258 (RPR 116258A), a novel taxane, administered as a 1-h infusion every 3 weeks in patients with advanced solid tumors. Clin Cancer Res 15:723–730
de Bono JS, Oudard S, Ozguroglu M et al (2010) Prednisone plus cabazitaxel or mitoxantrone for metastatic castration-resistant prostate cancer progressing after docetaxel treatment: a randomised open-label trial. Lancet 376:1147–1154
Parker C, Gillessen S, Heidenreich A et al (2015) Cancer of the prostate: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol 26(Suppl 5):69–77
Kelly WK, Scher HI, Mazumdar M et al (1993) Prostate-specific antigen as a measure of disease outcome in metastatic hormone-refractory prostate cancer. J Clin Oncol 11:607–615
Bubley GJ, Carducci M, Dahut W et al (1999) Eligibility and response guidelines for phase II clinical trials in androgen-independent prostate cancer: recommendations from the Prostate-Specific Antigen Working Group. J Clin Oncol 17:3461–3467
Francini E, Petrioli R, Rossi G et al (2014) PSA response rate as a surrogate marker for median overall survival in docetaxel-based first-line treatments for patients with metastatic castration-resistant prostate cancer: an analysis of 22 trials. Tumour Biol 35:10601–10607
Halabi S, Armstrong AJ, Sartor O et al (2013) Prostate-specific antigen changes as surrogate for overall survival in men with metastatic castration-resistant prostate cancer treated with second-line chemotherapy. J Clin Oncol 31:3944–3950
Scher HI, Morris MJ, Basch E et al (2011) End points and outcomes in castration-resistant prostate cancer: from clinical trials to clinical practice. J Clin Oncol 29:3695–3704
Armstrong AJ, Garrett-Mayer ES, Yang YC et al (2007) A contemporary prognostic nomogram for men with hormone-refractory metastatic prostate cancer: a TAX327 study analysis. Clin Cancer Res 13:6396–6403
Hofheinz RD, Lange C, Ecke T et al (2017) Quality of life and pain relief in men with metastatic castration-resistant prostate cancer on cabazitaxel: the non-interventional ‘QoLiTime’ study. BJU Int 119:731–740
Bahl A, Oudard S, Tombal B et al (2013) Impact of cabazitaxel on 2-year survival and palliation of tumour-related pain in men with metastatic castration-resistant prostate cancer treated in the TROPIC trial. Ann Oncol 24:2402–2408
Berthold DR, Pond GR, Roessner M et al (2008) Treatment of hormone-refractory prostate cancer with docetaxel or mitoxantrone: relationships between prostate-specific antigen, pain, and quality of life response and survival in the TAX-327 study. Clin Cancer Res 14:2763–2767
Karnofsky D, Burchenal J (1949) The clinical evaluation of chemotherapeutic agents in cancer. In: MacLeod C (ed) Evaluation of chemotherapeutic agents. Columbia University Press, New York, pp 191–205
Acknowledgements
Study funding and medical writing were funded by Sanofi. Sophie Rushton-Smith, PhD (MedLink Healthcare Communications Ltd) provided medical writing services under direction of the authors.
Author information
Authors and Affiliations
Contributions
PH collected the data and wrote the manuscript; S-EA-B and R-DH collected the data and edited the manuscript; CW-K performed statistical analysis and manuscript editing; MK contributed to project development and manuscript editing.
Corresponding author
Ethics declarations
Ethical standards
The study was performed according to Good Epidemiological Practice. All patients provided written informed consent.
Conflict of interest
Peter Hammerer is an Advisor/Speaker for Amgen, Astellas, Janssen, Sanofi, and Takeda. Salah-Eddin Al-Batran has an advisory role for Sanofi, Merck, Roche, Celgene, Lilly, Nordic pharma and has received research grants from Sanofi, Merck, Roche, Celgene, Vifor, Medac, Hospira, and Lilly. Christine Windemuth-Kieselbach, Alcedis GmbH, was commissioned for the statistical analyses by Sanofi. Martin Keller is an employee of Sanofi-Aventis Deutschland GmbH. Ralf-Dieter Hofheinz has received honoraria and research grants from Sanofi-Aventis.
Funding
This study is sponsored by Sanofi. The sponsor provided financial support for the conduct of the research and/or preparation of the article and was involved in the study design, analysis, and interpretation of data and in the writing of the report.
Rights and permissions
About this article
Cite this article
Hammerer, P., Al-Batran, SE., Windemuth-Kieselbach, C. et al. PSA response to cabazitaxel is associated with improved progression-free survival in metastatic castration-resistant prostate cancer: the non-interventional QoLiTime study. World J Urol 36, 375–381 (2018). https://doi.org/10.1007/s00345-017-2138-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-017-2138-x