Abstract
Objective
Quantitative computed tomography (qCT) is being increasingly incorporated in research studies and clinical trials aimed at understanding lung disease risk, progression, exacerbations, and intervention response. Menstrual cycle–based changes in lung function are recognized; however, the impact on qCT measures is currently unknown. We hypothesize that the menstrual cycle impacts qCT-derived measures of lung structure in healthy women and that the degree of measurement change may be mitigated in subjects on cyclic hormonal birth control.
Methods
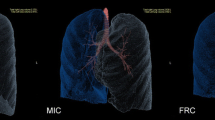
Thirty-one non-smoking, healthy women with regular menstrual cycles (16 of which were on cyclic hormonal birth control) underwent pulmonary function testing and qCT imaging at both menses and early luteal phase time points. Data were evaluated to identify lung measurements which changed significantly across the two key time points and to compare degree of change across metrics for the sub-cohort with versus without birth control.
Results
The segmental airway measurements were larger and mean lung density was higher at menses compared to the early luteal phase. The sub-cohort with cyclic hormonal birth control did not have less evidence of measurement difference over the menstrual cycle compared to the sub-cohort without hormonal birth control.
Conclusions
This study provides evidence that qCT-derived measures from the lung are impacted by the female menstrual cycle. This indicates studies seeking to use qCT as a more sensitive measure of cross-sectional differences or longitudinal changes in these derived lung measurements should consider acquiring data at a consistent time in the menstrual cycle for pre-menopausal women and warrants further exploration.
Key Points
• Lung measurements from chest computed tomography are used in multicenter studies exploring lung disease progression and treatment response.
• The menstrual cycle impacts lung structure measurements.
• Cyclic variability should be considered when evaluating longitudinal change with CT in menstruating women.
Similar content being viewed by others
Abbreviations
- COPD:
-
Chronic obstructive pulmonary disease
- DLCO :
-
Diffusing capacity for carbon monoxide
- E/I ratio:
-
Expiratory/inspiratory ratio
- ELP:
-
Early luteal phase
- FEV1 :
-
Forced expiratory volume in 1 second
- FVC:
-
Forced vital capacity
- LAA:
-
Low attenuation area
- M:
-
Menses
- MLD :
-
Mean lung density
- PFT:
-
Pulmonary function testing
- PMA:
-
Perimenstrual asthma
- qCT:
-
Quantitative computed tomography
- RV:
-
Residual volume
- TLC:
-
Total lung capacity
- VA:
-
Alveolar volume
References
Martinez FJ, Curtis JL, Sciurba F et al (2007) Sex differences in severe pulmonary emphysema. Am J Respir Crit Care Med 176:243–252
Oelsner EC, Ortega VE, Smith BM et al (2019) A genetic risk score associated with chronic obstructive pulmonary disease susceptibility and lung structure on computed tomography. Am J Respir Crit Care Med 200:721–731
Forman MR, Mangini LD, Thelus-Jean R, Hayward MD (2013) Life-course origins of the ages at menarche and menopause. Adolesc Health Med Ther 4:1–21
Farha S, Asosingh K, Laskowski D et al (2009) Effects of the menstrual cycle on lung function variables in women with asthma. Am J Respir Crit Care Med 180:304–310
Tam A, Morrish D, Wadsworth S, Dorscheid D, Man SF, Sin DD (2011) The role of female hormones on lung function in chronic lung diseases. BMC Womens Health 11:24
Han MK, Arteaga-Solis E, Blenis J et al (2018) Female sex and gender in lung/sleep health and disease. Increased understanding of basic biological, pathophysiological, and behavioral mechanisms leading to better health for female patients with lung disease. Am J Respir Crit Care Med 198:850–858
Farha S, Asosingh K, Laskowski D et al (1985) (2007) Pulmonary gas transfer related to markers of angiogenesis during the menstrual cycle. J Appl Physiol 103:1789–1795
Newell JD Jr, Fuld MK, Allmendinger T et al (2015) Very low-dose (0.15 mGy) chest CT protocols using the COPDGene 2 test object and a third-generation dual-source CT scanner with corresponding third-generation iterative reconstruction software. Invest Radiol 50:40–45
Hammond E, Sloan C, Newell JD Jr et al (2017) Comparison of low- and ultralow-dose computed tomography protocols for quantitative lung and airway assessment. Med Phys 44:4747–4757
Hammond E, Chan KS, Ames JC et al (2018) Impact of advanced detector technology and iterative reconstruction on low-dose quantitative assessment of lung computed tomography density in a biological lung model. Med Phys. https://doi.org/10.1002/mp.13057
Hoffman EA, Lynch DA, Barr RG, van Beek EJ, Parraga G (2016) Pulmonary CT and MRI phenotypes that help explain chronic pulmonary obstruction disease pathophysiology and outcomes. J Magn Reson Imaging 43:544–557
Castro M, Fain SB, Hoffman EA, Gierada DS, Erzurum SC, Wenzel S (2011) Lung imaging in asthmatic patients: the picture is clearer. J Allergy Clin Immunol 128:467–478
Sieren JP, Newell JD Jr, Barr RG et al (2016) SPIROMICS protocol for multicenter quantitative computed tomography to phenotype the lungs. Am J Respir Crit Care Med 194:794–806
Zimmerlin L, Donnenberg VS, Donnenberg AD (2011) Rare event detection and analysis in flow cytometry: bone marrow mesenchymal stem cells, breast cancer stem/progenitor cells in malignant effusions, and pericytes in disaggregated adipose tissue. Methods Mol Biol 699:251–273
Donnenberg AD, Donnenberg VS (2007) Rare-event analysis in flow cytometry. Clin Lab Med 27:627–652
Roederer M (2008) How many events is enough? Are you positive? Cytometry A 73:384–385
Tibbe AG, Miller MC, Terstappen LW (2007) Statistical considerations for enumeration of circulating tumor cells. Cytometry A 71:154–162
Hedley BD, Keeney M (2013) Technical issues: flow cytometry and rare event analysis. Int J Lab Hematol 35:344–350
Rose JA, Erzurum S, Asosingh K (2015) Biology and flow cytometry of proangiogenic hematopoietic progenitors cells. Cytometry A 87:5–19
Culver BH, Graham BL, Coates AL et al (2017) Recommendations for a Standardized pulmonary function report. An official American Thoracic Society technical statement. Am J Respir Crit Care Med 196:1463–1472
Seo S (2006) A review and comparison of methods for detecting outliers in univariate data sets Graduate School of Public Health > Biostatistics. University of Pittsburg
Guo J, Fuld M, Alford S, Reinhardt J, Hoffman E (2008) Pulmonary Analysis Software Suite 9.0: integrating quantitative measures of function with structural analyses. Proceedings of the First International Workshop on Pulmonary Image Analysis:283–292
Rees L (1963) An aetiological study of premenstrual asthma. J Psychosom Res 7:191–197
Gibbs CJ, Coutts II, Lock R, Finnegan OC, White RJ (1984) Premenstrual exacerbation of asthma. Thorax 39:833–836
Hanley SP (1981) Asthma variation with menstruation. Br J Dis Chest 75:306–308
Chandler MH, Schuldheisz S, Phillips BA, Muse KN (1997) Premenstrual asthma: the effect of estrogen on symptoms, pulmonary function, and beta 2-receptors. Pharmacotherapy 17:224–234
Nwaru BI, Sheikh A (2015) Hormonal contraceptives and asthma in women of reproductive age: analysis of data from serial national Scottish Health Surveys. J R Soc Med 108:358–371
Macsali F, Real FG, Omenaas ER et al (2009) Oral contraception, body mass index, and asthma: a cross-sectional Nordic-Baltic population survey. J Allergy Clin Immunol 123:391–397
Matheson MC, Burgess JA, Lau MY et al (2015) Hormonal contraception increases risk of asthma among obese but decreases it among nonobese subjects: a prospective, population-based cohort study. ERJ Open Res 1
Kauczor HU, Hast J, Heussel CP, Schlegel J, Mildenberger P, Thelen M (2002) CT attenuation of paired HRCT scans obtained at full inspiratory/expiratory position: comparison with pulmonary function tests. Eur Radiol 12:2757–2763
Mitsunobu F, Ashida K, Hosaki Y et al (2003) Decreased computed tomographic lung density during exacerbation of asthma. Eur Respir J 22:106
Yu N, Yuan H, Duan HF et al (2019) Determination of vascular alteration in smokers by quantitative computed tomography measurements. Medicine (Baltimore) 98:e14438
Soejima K, Yamaguchi K, Kohda E et al (2000) Longitudinal follow-up study of smoking-induced lung density changes by high-resolution computed tomography. Am J Respir Crit Care Med 161:1264–1273
Dixon AE, Peters U (2018) The effect of obesity on lung function. Expert Rev Respir Med 12:755–767
Acknowledgements
We thank Debra O’Connell-Moore and Sue Ellen Salisbury for assistance with regulatory approvals and subject recruitment, Jarron Atha for technical assistance with CT acquisition, Joshua Schirm for facilitating VIDA processing, and Nicholas Wanner for assistance with CD34+CD133+ flow cytometry.
Funding
This work was supported by the National Institutes of Health (NIH) R01HL112986 and P01HL103453. Imaging was performed using a CT system purchased through a shared instrumentation award (NIH S10OD018526).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Jessica Sieren.
Conflict of interest
The authors of this manuscript declare relationships with the following companies: EAH is a founder and shareholder of VIDA Diagnostics Inc., a company commercializing lung image analysis software developed, in part, at the University of Iowa. JG is a shareholder of VIDA Diagnostics Inc. and JCS has a family member that is a shareholder and receives compensation from VIDA Diagnostics. Siemens Healthcare has provided in-kind support for hardware and software residing at the University of Iowa and used in this project.
Statistics and biometry
The first and second authors, as biomedical engineers, have experience with biostatistics methods. No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• Prospective
• Observational
• Performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sieren, J.C., Schroeder, K.E., Guo, J. et al. Menstrual cycle impacts lung structure measures derived from quantitative computed tomography. Eur Radiol 32, 2883–2890 (2022). https://doi.org/10.1007/s00330-021-08404-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-021-08404-9