Abstract
Purpose
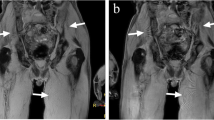
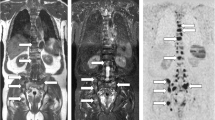
To compare 3D T1-weighted fast spin echo (FSE) and 3D T1-weighted gradient echo (GE) mDixon as morphologic sequences to complement diffusion-weighted imaging (DWI) for the metastatic screening in prostate cancer (PCa) patients.
Materials and methods
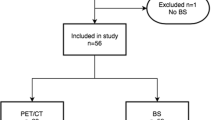
Thirty PCa patients at high risk of metastases prospectively underwent both a 3D T1 FSE (14 min) and a rapid 3D T1 GEmDixon (1 min 20 s) sequences within a WB-MRI protocol. Two readers assessed the diagnostic performance of the FSE/Fat/in-phase (IP)/IP+Fat sequences in detecting bone and node metastases. The reference standard was established by a panel of four physicians on the basis of all baseline and follow-up imaging, biological and clinical information. The reproducibility of readings, predictive accuracy (Acc) from ROC curves analysis, and contrast-to-reference ratio (CRR) in lesions were assessed for each sequence.
Results
In bone and lymph nodes (per-region analysis), reproducibility was at least good for all sequences/readers, except for nodes in the common iliac/inguinal regions. In bone (per-organ analysis), Acc of FSE was superior to that of mDixon (difference + 4%, p < 0.0083). In nodes (per-organ analysis), Acc of Fat was superior to that of other sequences (difference + 4% to + 6% depending on reader, p < 0.0083). In the per-patient analysis, Acc of FSE was superior to that of mDixon (difference + 4% to + 6% depending on sequence, p < 0.0083). Fat images had higher CRR compared with FSE in the thoracic spine, the bony pelvis and lymph node metastases (p < 0.025).
Conclusion
3D T1 GEmDixon may replace 3D T1 FSE to complement DWI in WB-MRI for metastatic screening in PCa. It demonstrates an Acc ranging from + 4% to + 6% (nodes) to − 4% to − 6% (bone and patient staging) compared with FSE and considerably reduces the examination time, offering the perspective of acquiring WB-MRI examinations in less than 20 min.
Key Points
• The replacement of 3D T1 FSE by the 3D T1 GE mDixon as morphologic sequence to complement DWI drastically reduces the acquisition time of WB-MRI studies.
• The 3D T1 GE mDixon sequence offers similar reproducibility of image readings compared with that of the 3D T1 FSE.
• Differences in diagnostic accuracy are limited (+ 4%/+ 6% in favor of mDixon to detect node metastases; + 4%/+ 6% in favor of FSE to detect bone metastases/metastatic disease in a patient).




Similar content being viewed by others
Abbreviations
- Acc:
-
Predictive accuracy
- ADC:
-
Apparent diffusion coefficient
- AUC:
-
Area under the receiver operating characteristic curve
- BCR:
-
Biochemical recurrence
- BS:
-
Bone scintigraphy
- BVC:
-
Best valuable comparator
- CI:
-
Confidence interval
- CRPC:
-
Castrate-resistant prostate cancer
- CRR:
-
Contrast-to-reference ratio
- DWI:
-
Diffusion-weighted imaging
- DWIBS:
-
DWI with background signal suppression
- FSE:
-
Fast spin echo
- GE:
-
Gradient echo
- IP:
-
In-phase
- IR:
-
Inversion recovery
- ND:
-
Newly diagnosed
- OP:
-
Out-phase
- PACS:
-
Picture Archiving and Communication System
- PCa:
-
Prostate cancer
- PET:
-
Positron emission tomography
- PSA:
-
Prostate-specific antigen
- ROC:
-
Receiver operating characteristic
- ROI:
-
Region of interest
- STIR:
-
Short tau inversion recovery
References
Steinborn MM, Heuck AF, Tiling R, Bruegel M, Gauger L, Reiser MF (1999) Whole-body bone marrow MRI in patients with metastatic disease to the skeletal system. J Comput Assist Tomogr 23:123–129
Lecouvet FE (2016) Whole-body MR imaging: musculoskeletal applications. Radiology 279:345–365
Pasoglou V, Michoux N, Tombal B, Jamar F, Lecouvet FE (2015) WbMRI to detect bone metastases: critical review on diagnostic accuracy and comparison to other imaging modalities. Clin Transl Imaging 3:141–157
Padhani AR, Lecouvet FE, Tunariu N et al (2017) Metastasis reporting and data system for prostate cancer: practical guidelines for acquisition, interpretation, and reporting of whole-body magnetic resonance imaging-based evaluations of multiorgan involvement in advanced prostate cancer. Eur Urol 71:81–92
Pasoglou V, Michoux N, Peeters F et al (2015) Whole-body 3D T1-weighted MR imaging in patients with prostate cancer: feasibility and evaluation in screening for metastatic disease. Radiology 275:155–166
Padhani AR, Lecouvet FE, Tunariu N et al (2017) Rationale for modernising imaging in advanced prostate cancer. Eur Urol Focus 3:223–239
Bray TJP, Singh S, Latifoltojar A et al (2017) Diagnostic utility of whole body Dixon MRI in multiple myeloma: a multi-reader study. PLoS One 12:e0180562
Johnston EW, Latifoltojar A, Sidhu HS et al (2018) Multiparametric whole-body 3.0-T MRI in newly diagnosed intermediate- and high-risk prostate cancer: diagnostic accuracy and interobserver agreement for nodal and metastatic staging. Eur Radiol 29(6):3159–3169. https://doi.org/10.1007/s00330-018-5813-4
Guerini H, Omoumi P, Guichoux F et al (2015) Fat suppression with Dixon techniques in musculoskeletal magnetic resonance imaging: a pictorial review. Semin Musculoskelet Radiol 19:335–347
Rambow O, Hazle J, Clark J, Ma J (2013) Direct water and fat determination in two-point Dixon imaging with flexible echo times. Med Phys 40:112302
Larbi A, Omoumi P, Pasoglou V et al (2018) Whole-body MRI to assess bone involvement in prostate cancer and multiple myeloma: comparison of the diagnostic accuracies of the T1, short tau inversion recovery (STIR), and high b-values diffusion-weighted imaging (DWI) sequences. Eur Radiol 29(8):4503–4513. https://doi.org/10.1007/s00330-018-5796-1
Widmann G, Henninger B, Kremser C, Jaschke W (2017) MRI sequences in head & neck radiology - state of the art. Rofo 189:413–422
Metser U, Chan R, Veit-Haibach P, Ghai S, Tau N (2019) Comparison of MRI sequences in whole-body PET/MRI for staging of patients with high-risk prostate cancer. AJR Am J Roentgenol 212:377–381
Bastian PJ, Boorjian SA, Bossi A et al (2012) High-risk prostate cancer: from definition to contemporary management. Eur Urol 61:1096–1106
Heidenreich A, Bastian PJ, Bellmunt J et al (2014) EAU guidelines on prostate cancer. Part II: Treatment of advanced, relapsing, and castration-resistant prostate cancer. Eur Urol 65:467–479
Barentsz JO, Weinreb JC, Verma S et al (2016) Synopsis of the PI-RADS v2 guidelines for multiparametric prostate magnetic resonance imaging and recommendations for use. Eur Urol 69:41–49
Eggers H, Brendel B, Duijndam A, Herigault G (2011) Dual-echo Dixon imaging with flexible choice of echo times. Magn Reson Med 65:96–107
Costelloe CM, Madewell JE, Kundra V, Harrell RK, Bassett RL Jr, Ma J (2013) Conspicuity of bone metastases on fast Dixon-based multisequence whole-body MRI: clinical utility per sequence. Magn Reson Imaging 31:669–675
Scott WA (1955) Reliability of content analysis: the case of nominal scale coding. Public Opin Q:321–325
Maeder Y, Dunet V, Richard R, Becce F, Omoumi P (2018) Bone marrow metastases: T2-weighted Dixon spin-echo fat images can replace T1-weighted spin-echo images. Radiology 286:948–959
Lecouvet FE, Geukens D, Stainier A et al (2007) Magnetic resonance imaging of the axial skeleton for detecting bone metastases in patients with high-risk prostate cancer: diagnostic and cost-effectiveness and comparison with current detection strategies. J Clin Oncol 25:3281–3287
Zweig MH, Campbell G (1993) Receiver-operating characteristic (ROC) plots: a fundamental evaluation tool in clinical medicine. Clin Chem 39:561–577
Curran-Everett D (2000) Multiple comparisons: philosophies and illustrations. Am J Physiol Regul Integr Comp Physiol 279:R1–R8
Messiou C, Hillengass J, Delorme S et al (2019) Guidelines for acquisition, interpretation, and reporting of whole-body MRI in myeloma: Myeloma Response Assessment and Diagnosis System (MY-RADS). Radiology 291:5–13
Park HJ, Lee SY, Rho MH et al (2016) Usefulness of the fast spin-echo three-point Dixon (mDixon) image of the knee joint on 3.0-T MRI: comparison with conventional fast spin-echo T2 weighted image. Br J Radiol 89:20151074
Gaddikeri S, Mossa-Basha M, Andre JB, Hippe DS, Anzai Y (2018) Optimal fat suppression in head and neck MRI: comparison of multipoint Dixon with 2 different fat-suppression techniques, spectral presaturation and inversion recovery, and STIR. AJNR Am J Neuroradiol 39:362–368
Samji K, Alrashed A, Shabana WM, McInnes MD, Bayram E, Schieda N (2016) Comparison of high-resolution T1W 3D GRE (LAVA) with 2-point Dixon fat/water separation (FLEX) to T1W fast spin echo (FSE) in prostate cancer (PCa). Clin Imaging 40:407–413
Kochanek KD, Murphy SL, Xu J, Tejada-Vera B (2016) Deaths: final data for 2014. Natl Vital Stat Rep 65:1–122
Nam JG, Lee JM, Lee SM et al (2019) High acceleration three-dimensional T1-weighted dual echo Dixon hepatobiliary phase imaging using compressed sensing-sensitivity encoding: comparison of image quality and solid lesion detectability with the standard T1-weighted sequence. Korean J Radiol 20:438–448
Wang X, Pirasteh A, Brugarolas J et al (2018) Whole-body MRI for metastatic cancer detection using T2 -weighted imaging with fat and fluid suppression. Magn Reson Med 80:1402–1415
Mosavi F, Laurell A, Ahlstrom H (2015) Whole body MRI, including diffusion-weighted imaging in follow-up of patients with testicular cancer. Acta Oncol 54:1763–1769
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is F.E. Lecouvet.
Conflict of interest
One of the authors of this manuscript (Vincent Denolin) was an employee of Philips Medical Systems International at the time of this study. The remaining authors declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has significant statistical expertise (N. Michoux).
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
Study subjects or cohorts have not been previously reported.
Methodology
• Prospective
• Diagnostic or prognostic study
• Performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 58 kb)
Rights and permissions
About this article
Cite this article
Lecouvet, F.E., Pasoglou, V., Van Nieuwenhove, S. et al. Shortening the acquisition time of whole-body MRI: 3D T1 gradient echo Dixon vs fast spin echo for metastatic screening in prostate cancer. Eur Radiol 30, 3083–3093 (2020). https://doi.org/10.1007/s00330-019-06515-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-019-06515-y