Abstract
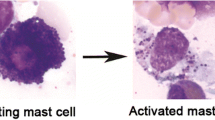
CD69 is an activation marker on leukocytes. Early studies showed that the CD69+ cells were detected in the lung of patients with asthmatic and eosinophilic pneumonia, suggesting that CD69 might play crucial roles in the pathogenesis of such inflammatory diseases, rather than simply being an activation marker. Intensive studies using mouse models have since clarified that CD69 is a functional molecule regulating the immune responses. We discovered that Myosin light chain 9, 12a, 12b (Myl9/12) are ligands for CD69 and that platelet-derived Myl9 forms a net-like structure (Myl9 nets) that is strongly detected inside blood vessels in inflamed lung. CD69-expressing activated T cells attached to the Myl9 nets can thereby migrate into the inflamed tissues through a system known as the CD69-Myl9 system. In this review, we summarize the discovery of the CD69-Myl9 system and discuss how this system is important in inflammatory immune responses. In addition, we discuss our recent finding that CD69 controls the exhaustion status of tumor-infiltrating T cells and that the blockade of the CD69 function enhances anti-tumor immunity. Finally, we discuss the possibility of CD69 as a new therapeutic target for patients with intractable inflammatory disorders and tumors


Similar content being viewed by others
References
Ziegler SF, Ramsdell F, Hjerrild KA, Armitage RJ, Grabstein KH, Hennen KB, Farrah T, Fanslow WC, Shevach EM, Alderson MR (1993) Molecular characterization of the early activation antigen CD69: a type II membrane glycoprotein related to a family of natural killer cell activation antigens. Eur J Immunol 23:1643–1648
Lopez-Cabrera M, Santis AG, Fernandez-Ruiz E, Blacher R, Esch F, Sanchez-Mateos P, Sanchez-Madrid F (1993) Molecular cloning, expression, and chromosomal localization of the human earliest lymphocyte activation antigen AIM/CD69, a new member of the C-type animal lectin superfamily of signal-transmitting receptors. J Exp Med 178:537–547
Kimura MY, Hayashizaki K, Tokoyoda K, Takamura S, Motohashi S, Nakayama T (2017) Crucial role for CD69 in allergic inflammatory responses: CD69-Myl9 system in the pathogenesis of airway inflammation. Immunol Rev 278:87–100
Llera AS, Viedma F, Sanchez-Madrid F, Tormo J (2001) Crystal structure of the C-type lectin-like domain from the human hematopoietic cell receptor CD69. J Biol Chem 276:7312–7319
Lin CR, Wei TY, Tsai HY, Wu YT, Wu PY, Chen ST (2015) Glycosylation-dependent interaction between CD69 and S100A8/S100A9 complex is required for regulatory T-cell differentiation. FASEB J 29:5006–5017
de la Fuente H, Cruz-Adalia A, Martinez Del Hoyo G, Cibrian-Vera D, Bonay P, Perez-Hernandez D, Vazquez J, Navarro P, Gutierrez-Gallego R, Ramirez-Huesca M, Martin P, Sanchez-Madrid F (2014) The leukocyte activation receptor CD69 controls T cell differentiation through its interaction with galectin-1. Mol Cell Biol 34:2479–2487
Hayashizaki K, Kimura MY, Tokoyoda K, Hosokawa H, Shinoda K, Hirahara K, Ichikawa T, Onodera A, Hanazawa A, Iwamura C, Kakuta J, Muramoto K, Motohashi S, Tumes DJ, Iinuma T, Yamamoto H, Ikehara Y, Okamoto H, Nakayama T (2016) Myosin light chains 9 and 12 are functional ligands for CD69 that regulate airway inflammation. Sci Immunol 1:eaaf9154
Mendez-Huergo SP, Blidner AG, Rabinovich GA (2017) Galectins: emerging regulatory checkpoints linking tumor immunity and angiogenesis. Curr Opin Immunol 45:8–15
Stillman BN, Hsu DK, Pang M, Brewer CF, Johnson P, Liu FT, Baum LG (2006) Galectin-3 and galectin-1 bind distinct cell surface glycoprotein receptors to induce T cell death. J Immunol 176:778–789
Starossom SC, Mascanfroni ID, Imitola J, Cao L, Raddassi K, Hernandez SF, Bassil R, Croci DO, Cerliani JP, Delacour D, Wang Y, Elyaman W, Khoury SJ, Rabinovich GA (2012) Galectin-1 deactivates classically activated microglia and protects from inflammation-induced neurodegeneration. Immunity 37:249–263
Bonzi J, Bornet O, Betzi S, Kasper BT, Mahal LK, Mancini SJ, Schiff C, Sebban-Kreuzer C, Guerlesquin F, Elantak L (2015) Pre-B cell receptor binding to galectin-1 modifies galectin-1/carbohydrate affinity to modulate specific galectin-1/glycan lattice interactions. Nat Commun 6:6194
Gebhardt C, Nemeth J, Angel P, Hess J (2006) S100A8 and S100A9 in inflammation and cancer. Biochem Pharmacol 72:1622–1631
Testi R, Pulcinelli F, Frati L, Gazzaniga PP, Santoni A (1990) CD69 is expressed on platelets and mediates platelet activation and aggregation. J Exp Med 172:701–707
Testi R, D’Ambrosio D, De Maria R, Santoni A (1994) The CD69 receptor: a multipurpose cell-surface trigger for hematopoietic cells. Immunol Today 15:479–483
Gonzalez-Amaro R, Cortes JR, Sanchez-Madrid F, Martin P (2013) Is CD69 an effective brake to control inflammatory diseases? Trends Mol Med 19:625–632
Martin P, Gomez M, Lamana A, Cruz-Adalia A, Ramirez-Huesca M, Ursa MA, Yanez-Mo M, Sanchez-Madrid F (2010) CD69 association with Jak3/Stat5 proteins regulates Th17 cell differentiation. Mol Cell Biol 30:4877–4889
Cyster JG, Schwab SR (2012) Sphingosine-1-phosphate and lymphocyte egress from lymphoid organs. Annu Rev Immunol 30:69–94
Bankovich AJ, Shiow LR, Cyster JG (2010) CD69 suppresses sphingosine 1-phosophate receptor-1 (S1P1) function through interaction with membrane helix 4. J Biol Chem 285:22328–22337
Spiegel S, Milstien S (2003) Sphingosine-1-phosphate: an enigmatic signalling lipid. Nat Rev Mol Cell Biol 4:397–407
Shiow LR, Rosen DB, Brdickova N, Xu Y, An J, Lanier LL, Cyster JG, Matloubian M (2006) CD69 acts downstream of interferon-alpha/beta to inhibit S1P1 and lymphocyte egress from lymphoid organs. Nature 440:540–544
Feng C, Woodside KJ, Vance BA, El-Khoury D, Canelles M, Lee J, Gress R, Fowlkes BJ, Shores EW, Love PE (2002) A potential role for CD69 in thymocyte emigration. Int Immunol 14:535–544
Nakayama T, Kasprowicz DJ, Yamashita M, Schubert LA, Gillard G, Kimura M, Didierlaurent A, Koseki H, Ziegler SF (2002) The generation of mature, single-positive thymocytes in vivo is dysregulated by CD69 blockade or overexpression. J Immunol 168:87–94
Zachariah MA, Cyster JG (2010) Neural crest-derived pericytes promote egress of mature thymocytes at the corticomedullary junction. Science 328:1129–1135
Murata K, Inami M, Hasegawa A, Kubo S, Kimura M, Yamashita M, Hosokawa H, Nagao T, Suzuki K, Hashimoto K, Shinkai H, Koseki H, Taniguchi M, Ziegler SF, Nakayama T (2003) CD69-null mice protected from arthritis induced with anti-type II collagen antibodies. Int Immunol 15:987–992
Lauzurica P, Sancho D, Torres M, Albella B, Marazuela M, Merino T, Bueren JA, Martinez AC, Sanchez-Madrid F (2000) Phenotypic and functional characteristics of hematopoietic cell lineages in CD69-deficient mice. Blood 95:2312–2320
Kimura MY, Igi A, Hayashizaki K, Mita Y, Shinzawa M, Kadakia T, Endo Y, Ogawa S, Yagi R, Motohashi S, Singer A, Nakayama T (2018) CD69 prevents PLZF(hi) innate precursors from prematurely exiting the thymus and aborting NKT2 cell differentiation. Nat Commun 9:3749
Hall JG, Morris B (1965) The immediate effect of antigens on the cell output of a lymph node. Br J Exp Pathol 46:450–454
Grigorova IL, Panteleev M, Cyster JG (2010) Lymph node cortical sinus organization and relationship to lymphocyte egress dynamics and antigen exposure. Proc Natl Acad Sci U S A 107:20447–20452
Schenkel JM, Masopust D (2014) Tissue-resident memory T cells. Immunity 41:886–897
Miki-Hosokawa T, Hasegawa A, Iwamura C, Shinoda K, Tofukuji S, Watanabe Y, Hosokawa H, Motohashi S, Hashimoto K, Shirai M, Yamashita M, Nakayama T (2009) CD69 controls the pathogenesis of allergic airway inflammation. J Immunol 183:8203–8215
Wang HY, Dai Y, Wang JL, Yang XY, Jiang XG (2015) Anti-CD69 monoclonal antibody treatment inhibits airway inflammation in a mouse model of asthma. J Zhejiang Univ Sci B 16:622–631
Tsuyusaki J, Kuroda F, Kasuya Y, Ishizaki S, Yamauchi K, Sugimoto H, Kono T, Iwamura C, Nakayama T, Tatsumi K (2011) Cigarette smoke-induced pulmonary inflammation is attenuated in CD69-deficient mice. J Recept Signal Transduct Res 31:434–439
Yamauchi K, Kasuya Y, Kuroda F, Tanaka K, Tsuyusaki J, Ishizaki S, Matsunaga H, Iwamura C, Nakayama T, Tatsumi K (2011) Attenuation of lung inflammation and fibrosis in CD69-deficient mice after intratracheal bleomycin. Respir Res 12:131
Hasegawa A, Iwamura C, Kitajima M, Hashimoto K, Otsuyama K, Ogino H, Nakayama T, Shirai M (2013) Crucial role for CD69 in the pathogenesis of dextran sulphate sodium-induced colitis. PLoS One 8:e65494
Radulovic K, Manta C, Rossini V, Holzmann K, Kestler HA, Wegenka UM, Nakayama T, Niess JH (2012) CD69 regulates type I IFN-induced tolerogenic signals to mucosal CD4 T cells that attenuate their colitogenic potential. J Immunol 188:2001–2013
Radulovic K, Rossini V, Manta C, Holzmann K, Kestler HA, Niess JH (2013) The early activation marker CD69 regulates the expression of chemokines and CD4 T cell accumulation in intestine. PLoS One 8:e65413
Cortes JR, Sanchez-Diaz R, Bovolenta ER, Barreiro O, Lasarte S, Matesanz-Marin A, Toribio ML, Sanchez-Madrid F, Martin P (2014) Maintenance of immune tolerance by Foxp3+ regulatory T cells requires CD69 expression. J Autoimmun 55:51–62
Shinoda K, Tokoyoda K, Hanazawa A, Hayashizaki K, Zehentmeier S, Hosokawa H, Iwamura C, Koseki H, Tumes DJ, Radbruch A, Nakayama T (2012) Type II membrane protein CD69 regulates the formation of resting T-helper memory. Proc Natl Acad Sci U S A 109:7409–7414
Nakayama T, Yoshikawa M, Asaka D, Okushi T, Matsuwaki Y, Otori N, Hama T, Moriyama H (2011) Mucosal eosinophilia and recurrence of nasal polyps—new classification of chronic rhinosinusitis. Rhinology 49:392–396
Shinoda K, Hirahara K, Iinuma T, Ichikawa T, Suzuki AS, Sugaya K, Tumes DJ, Yamamoto H, Hara T, Tani-Ichi S, Ikuta K, Okamoto Y, Nakayama T (2016) Thy1+IL-7+ lymphatic endothelial cells in iBALT provide a survival niche for memory T-helper cells in allergic airway inflammation. Proc Natl Acad Sci U S A 113:E2842–E2851
Garcia BA, Smalley DM, Cho H, Shabanowitz J, Ley K, Hunt DF (2005) The platelet microparticle proteome. J Proteome Res 4:1516–1521
Gilles L, Bluteau D, Boukour S, Chang Y, Zhang Y, Robert T, Dessen P, Debili N, Bernard OA, Vainchenker W, Raslova H (2009) MAL/SRF complex is involved in platelet formation and megakaryocyte migration by regulating MYL9 (MLC2) and MMP9. Blood 114:4221–4232
Seri M, Cusano R, Gangarossa S, Caridi G, Bordo D, Lo Nigro C, Ghiggeri GM, Ravazzolo R, Savino M, Del Vecchio M, d’Apolito M, Iolascon A, Zelante LL, Savoia A, Balduini CL, Noris P, Magrini U, Belletti S, Heath KE, Babcock M, Glucksman MJ, Aliprandis E, Bizzaro N, Desnick RJ, Martignetti JA (2000) Mutations in MYH9 result in the May-Hegglin anomaly, and Fechtner and Sebastian syndromes. The May-Heggllin/Fechtner Syndrome Consortium. Nat Genet 26:103–105
Lopez-Cabrera M, Munoz E, Blazquez MV, Ursa MA, Santis AG, Sanchez-Madrid F (1995) Transcriptional regulation of the gene encoding the human C-type lectin leukocyte receptor AIM/CD69 and functional characterization of its tumor necrosis factor-alpha-responsive elements. J Biol Chem 270:21545–21551
Kohlmeier JE, Miller SC, Woodland DL (2007) Cutting edge: antigen is not required for the activation and maintenance of virus-specific memory CD8+ T cells in the lung airways. J Immunol 178:4721–4725
Ledgerwood LG, Lal G, Zhang N, Garin A, Esses SJ, Ginhoux F, Merad M, Peche H, Lira SA, Ding Y, Yang Y, He X, Schuchman EH, Allende ML, Ochando JC, Bromberg JS (2008) The sphingosine 1-phosphate receptor 1 causes tissue retention by inhibiting the entry of peripheral tissue T lymphocytes into afferent lymphatics. Nat Immunol 9:42–53
Takamura S, Roberts AD, Jelley-Gibbs DM, Wittmer ST, Kohlmeier JE, Woodland DL (2010) The route of priming influences the ability of respiratory virus-specific memory CD8+ T cells to be activated by residual antigen. J Exp Med 207:1153–1160
Casey KA, Fraser KA, Schenkel JM, Moran A, Abt MC, Beura LK, Lucas PJ, Artis D, Wherry EJ, Hogquist K, Vezys V, Masopust D (2012) Antigen-independent differentiation and maintenance of effector-like resident memory T cells in tissues. J Immunol 188:4866–4875
Skon CN, Lee JY, Anderson KG, Masopust D, Hogquist KA, Jameson SC (2013) Transcriptional downregulation of S1pr1 is required for the establishment of resident memory CD8+ T cells. Nat Immunol 14:1285–1293
Esplugues E, Sancho D, Vega-Ramos J, Martinez C, Syrbe U, Hamann A, Engel P, Sanchez-Madrid F, Lauzurica P (2003) Enhanced antitumor immunity in mice deficient in CD69. J Exp Med 197:1093–1106
Esplugues E, Vega-Ramos J, Cartoixa D, Vazquez BN, Salaet I, Engel P, Lauzurica P (2005) Induction of tumor NK-cell immunity by anti-CD69 antibody therapy. Blood 105:4399–4406
Wei SM, Pan HL, Wang L, Yin GL, Zhong K, Zhou Y, Yang SJ, Xin ZL (2017) Combination therapy with dendritic cell-based vaccine and anti-CD69 antibody enhances antitumor efficacy in renal cell carcinoma-bearing mice. Turk J Med Sci 47:658–667
Mita Y, Kimura MY, Hayashizaki K, Koyama-Nasu R, Ito T, Motohashi S, Okamoto Y, Nakayama T (2018) Crucial role of CD69 in anti-tumor immunity through regulating the exhaustion of tumor-infiltrating T cells. Int Immunol 30:559–567
Budhu S, Schaer DA, Li Y, Toledo-Crow R, Panageas K, Yang X, Zhong H, Houghton AN, Silverstein SC, Merghoub T, Wolchok JD (2017) Blockade of surface-bound TGF-beta on regulatory T cells abrogates suppression of effector T cell function in the tumor microenvironment. Sci Signal 10:eaak9702
Mariathasan S, Turley SJ, Nickles D, Castiglioni A, Yuen K, Wang Y, Kadel EE III, Koeppen H, Astarita JL, Cubas R, Jhunjhunwala S, Banchereau R, Yang Y, Guan Y, Chalouni C, Ziai J, Senbabaoglu Y, Santoro S, Sheinson D, Hung J, Giltnane JM, Pierce AA, Mesh K, Lianoglou S, Riegler J, Carano RAD, Eriksson P, Hoglund M, Somarriba L, Halligan DL, van der Heijden MS, Loriot Y, Rosenberg JE, Fong L, Mellman I, Chen DS, Green M, Derleth C, Fine GD, Hegde PS, Bourgon R, Powles T (2018) TGFbeta attenuates tumour response to PD-L1 blockade by contributing to exclusion of T cells. Nature 554:544–548
Tauriello DVF, Palomo-Ponce S, Stork D, Berenguer-Llergo A, Badia-Ramentol J, Iglesias M, Sevillano M, Ibiza S, Canellas A, Hernando-Momblona X, Byrom D, Matarin JA, Calon A, Rivas EI, Nebreda AR, Riera A, Attolini CS, Batlle E (2018) TGFbeta drives immune evasion in genetically reconstituted colon cancer metastasis. Nature 554:538–543
Yang ZZ, Grote DM, Xiu B, Ziesmer SC, Price-Troska TL, Hodge LS, Yates DM, Novak AJ, Ansell SM (2014) TGF-beta upregulates CD70 expression and induces exhaustion of effector memory T cells in B-cell non-Hodgkin’s lymphoma. Leukemia 28:1872–1884
Webb JR, Milne K, Watson P, Deleeuw RJ, Nelson BH (2014) Tumor-infiltrating lymphocytes expressing the tissue resident memory marker CD103 are associated with increased survival in high-grade serous ovarian cancer. Clin Cancer Res 20:434–444
Djenidi F, Adam J, Goubar A, Durgeau A, Meurice G, de Montpreville V, Validire P, Besse B, Mami-Chouaib F (2015) CD8+CD103+ tumor-infiltrating lymphocytes are tumor-specific tissue-resident memory T cells and a prognostic factor for survival in lung cancer patients. J Immunol 194:3475–3486
Wang B, Wu S, Zeng H, Liu Z, Dong W, He W, Chen X, Dong X, Zheng L, Lin T, Huang J (2015) CD103+ tumor infiltrating lymphocytes predict a favorable prognosis in urothelial cell carcinoma of the bladder. J Urol 194:556–562
Ganesan AP, Clarke J, Wood O, Garrido-Martin EM, Chee SJ, Mellows T, Samaniego-Castruita D, Singh D, Seumois G, Alzetani A, Woo E, Friedmann PS, King EV, Thomas GJ, Sanchez-Elsner T, Vijayanand P, Ottensmeier CH (2017) Tissue-resident memory features are linked to the magnitude of cytotoxic T cell responses in human lung cancer. Nat Immunol 18:940–950
Koh J, Kim S, Kim MY, Go H, Jeon YK, Chung DH (2017) Prognostic implications of intratumoral CD103+ tumor-infiltrating lymphocytes in pulmonary squamous cell carcinoma. Oncotarget 8:13762–13769
Edwards J, Wilmott JS, Madore J, Gide TN, Quek C, Tasker A, Ferguson A, Chen J, Hewavisenti R, Hersey P, Gebhardt T, Weninger W, Britton WJ, Saw RPM, Thompson JF, Menzies AM, Long GV, Scolyer RA, Palendira U (2018) CD103(+) tumor-resident CD8(+) T cells are associated with improved survival in immunotherapy-naive melanoma patients and expand significantly during anti-PD-1 treatment. Clin Cancer Res 24:3036–3045
Duhen T, Duhen R, Montler R, Moses J, Moudgil T, de Miranda NF, Goodall CP, Blair TC, Fox BA, McDermott JE, Chang SC, Grunkemeier G, Leidner R, Bell RB, Weinberg AD (2018) Co-expression of CD39 and CD103 identifies tumor-reactive CD8 T cells in human solid tumors. Nat Commun 9:2724
Simoni Y, Becht E, Fehlings M, Loh CY, Koo SL, Teng KWW, Yeong JPS, Nahar R, Zhang T, Kared H, Duan K, Ang N, Poidinger M, Lee YY, Larbi A, Khng AJ, Tan E, Fu C, Mathew R, Teo M, Lim WT, Toh CK, Ong BH, Koh T, Hillmer AM, Takano A, Lim TKH, Tan EH, Zhai W, Tan DSW, Tan IB, Newell EW (2018) Bystander CD8(+) T cells are abundant and phenotypically distinct in human tumour infiltrates. Nature 557:575–579
Park SL, Buzzai A, Rautela J, Hor JL, Hochheiser K, Effern M, McBain N, Wagner T, Edwards J, McConville R, Wilmott JS, Scolyer RA, Tuting T, Palendria U, Gyorki D, Mueller SN, Huntington ND, Bedoui S, Holzel M, Mackay LK, Waithman J, Gebhardt T (2019) Tissue-resident memory CD8(+) T cells promote melanoma-immune equilibrium in skin. Nature 565:366–371
Schreiber RD, Old LJ, Smyth MJ (2011) Cancer immunoediting: integrating immunity’s roles in cancer suppression and promotion. Science 331:1565–1570
Acknowledgments
The authors acknowledge grants from the Ministry of Education, Culture, Sports, Science and Technology, Japan: Grants-in Aid for Scientific Research (S) #26221305, (C) 18K07257, (C) 18K07165 and 17K15715, Grants-in Aid for Scientific Research on Innovative Areas #17H05787, Grants-in Aid for Challenging Research (Exploratory) #18K19466 and Practical Research Project for Allergic Diseases and Immunology from Japan Agency for Medical Research and Development (AMED) [JP18ek0410030], Project for Cancer Research and Therapeutic Evolution (P-CREATE) (AMED) [JP18cm0106339], Advanced Research & Development Programs for Medical Innovation, (AMED-CREST) (AMED) [JP18gm1210003].
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
T. Nakayama has received research fund from Genefrontier (Chiba, Japan). M.Y. Kimura, R. Koyama-Nasu, and R. Yagi declare that they have no conflict of interest.
Additional information
This article is a contribution to the special issue on The Pathogenicity of Acquired Immunity in Human Diseases - Guest Editor: Kiyoshi Hirahara
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kimura, M.Y., Koyama-Nasu, R., Yagi, R. et al. A new therapeutic target: the CD69-Myl9 system in immune responses. Semin Immunopathol 41, 349–358 (2019). https://doi.org/10.1007/s00281-019-00734-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00281-019-00734-7