Abstract
Background
Little is known about the clinical outcome of children and adolescent patients with primary malignant sacral tumours.
Method
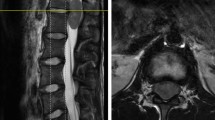
We retrospectively reviewed 40 patients with malignant sacral tumours aged ≤ 18 years, receiving surgery based on the previous proposed surgical resection classification at our centre from 2003 to 2018. The following data were collected in the present study: age, gender, radiological images, detailed information of the surgical procedure, pulmonary and other metastasis at presentation, complications, local recurrence, metastasis, and death during the follow-up were recorded from the clinical and follow-up files.
Results
The mean follow-up was 30.7 months (range, 5.2–146.7 months). The incidence of local recurrence was 27.5% (11/40). Seven cases had surgical site infection and there were 12 cases of wound dehiscence. One had a deep venous thrombosis and one had femoral artery thrombosis. Three had fixation breakage and then received a revision. Tenty-two patients (22/40, 55%) were free of disease. A total of 13 deaths (13/40, 32.5%) were observed and the mean overall survival period was 17.1 months (range, 6.3–34.2 months), and a pulmonary metastasis occurred in 18 patients (45%, 18/45) at the 12.0 ± 10.3 months (range, 2.2–35.3 months) after initial surgery. The overall survival rates at one, two and five years were respectively 88.3%, 62.5%, and 51.9%. In the stratification analysis of young patients with primary malignant tumours at the sacrum after surgery, it revealed the influence of pathological grade, location, and age on the oncological outcomes. Kaplan-Meier estimated a survivorship curve of patients with high and low-grade malignant tumours and showed statistical differences in the overall survival and distant relapse-free survival rates between two groups. Afterwards, the result demonstrated that paediatric patients aged ≤ 14 years had worse prognosis than those aged > 14 years.
Conclusions
It is satisfactory for the outcome of surgical treatment of children and adolescent patients with primary malignant sacral tumours based on proposed surgical classification. Furthermore, paediatric patients aged ≤ 14 years have the tendency of poor prognosis compared to adolescent aged > 14 years.









Similar content being viewed by others
References
Billmire DF (2006) Malignant germ cell tumors in childhood. Semin Pediatr Surg 15:30–36
De Corti F, Sarnacki S, Patte C et al (2012) Prognosis of malignant sacrococcygeal germ cell tumours according to their natural history and surgical management. Surg Oncol 21:e31–ee7
Kurugoglu S, Adaletli I, Mihmanli I, Kanberoglu K (2008) Lumbosacral osseous tumors in children. Eur J Radiol 65:257–269
Loh JK, Lin CK, Hwang YF, Hwang SL, Kwan AL, Howng SL (2005) Primary spinal tumors in children. J Clin Neurosci 12:246–248
Tsitouras V, Wang S, Dirks P et al (2016) Management and outcome of chordomas in the pediatric population: the hospital for sick children experience and review of the literature. J Clin Neurosci 34:169–176
Wang Y, Guo W, Shen D et al (2017) Surgical treatment of primary osteosarcoma of the sacrum. Spine 42:1207–1213
Arkader A, Yang CH, Tolo VT (2012) High long-term local control with sacrectomy for primary high-grade bone sarcoma in children. Clin Orthop Relat Res 470:1491–1497
Li D, Guo W, Tang X, Ji T, Zhang Y (2011) Surgical classification of different types of en bloc resection for primary malignant sacral tumors. Eur Spine J 20:2275–2281
Ozaki T, Flege S, Liljenqvist U et al (2002) Osteosarcoma of the spine: experience of the cooperative osteosarcoma study group. Cancer 94:1069–1077
Kiiski J, Kuokkanen HO, Kaariainen M, Kaartinen IS, Pakarinen TK, Laitinen MK (2018) Clinical results and quality of life after reconstruction following sacrectomy for primary bone malignancy. J Plast Reconstr Aesthet Surg 71:1730–1739
Li D, Guo W, Tang X et al (2014) Preservation of the contralateral sacral nerves during hemisacrectomy for sacral malignancies. Eur Spine J 23:1933–1939
Wei R, Guo W, Ji T, Zhang Y, Liang H (2017) One-step reconstruction with a 3D-printed, custom-made prosthesis after total en bloc sacrectomy: a technical note. Eur Spine J 26:1902–1909
Ozkan E, Gupta S (2011) Embolization of spinal tumors: vascular anatomy, indications, and technique. Tech Vasc Interv Radiol 14(3):129–140
Yang HL, Chen KW, Wang GL et al (2010) Pre-operative transarterial embolization for treatment of primary sacral tumors. J Clin Neurosci 17:1280–1285
Kerr DL, Dial BL, Lazarides AL et al (2019) Epidemiologic and survival trends in adult primary bone tumors of the spine. Spine J 19:1941–1949
Groves ML, Zadnik PL, Kaloostian P et al (2015) Epidemiologic, functional, and oncologic outcome analysis of spinal sarcomas treated surgically at a single institution over 10 years. Spine J 15:110–114
Li D, Guo W, Qu H et al (2013) Experience with wound complications after surgery for sacral tumors. Eur Spine J 22:2069–2076
Ruggieri P, Angelini A, Pala E, Mercuri M (2012) Infections in surgery of primary tumors of the sacrum. Spine 37:420–428
Ricciardi BF, Bostrom MP, Lidgren L, Ranstam J, Merollini KM, A WD (2014) Prevention of surgical site infection in total joint arthroplasty: an international tertiary care center survey. HSS J 10:45–51
Yamamoto Y, Kanzaki R, Kanou T et al (2019) Long-term outcomes and prognostic factors of pulmonary metastasectomy for osteosarcoma and soft tissue sarcoma. Int J Clin Oncol 24:863–870
Weeden S, Grimer RJ, Cannon SR, Taminiau AH, Uscinska BM, Intergroup EO (2001) The effect of local recurrence on survival in resected osteosarcoma. Eur J Cancer 37:39–46
Smeland S, Bielack SS, Whelan J et al (2019) Survival and prognosis with osteosarcoma: outcomes in more than 2000 patients in the EURAMOS-1 (European and American Osteosarcoma Study) cohort. Eur J Cancer 109:36–50
Min D, Lin F, Shen Z et al (2013) Analysis of prognostic factors in 333 Chinese patients with high-grade osteosarcoma treated by multidisciplinary combined therapy. Asia Pac J Clin Oncol 9:71–79
Cho HW, Lee JW, Ma Y, Yoo KH, Sung KW, Koo HH (2018) Treatment outcomes in children and adolescents with relapsed or progressed solid tumors: a 20-year, single-center study. J Korean Med Sci 33:e260
Wang Z, Wu B, Zhou Y et al (2019) Predictors of the survival of primary and secondary older osteosarcoma patients. J Cancer 10:4614–4622
Duchman KR, Gao Y, Miller BJ (2015) Prognostic factors for survival in patients with high-grade osteosarcoma using the surveillance, epidemiology, and end results (SEER) program database. Cancer Epidemiol 39:593–599
Morsy AM, Abdelgawad MI, Ahmed BM et al (2019) Pediatric osteosarcoma of extremities-a 15-year experience from a tertiary care cancer center in upper Egypt. J Pediatr Hematol Oncol 41:e371–ee83
Acknowledgments
Not applicable.
Funding
This work was supported by the Natural Science Foundation of China (NO:81702657) and Beijing Municipal Science & Technology Commission (No:Z181100001918025).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Rights and permissions
About this article
Cite this article
Wang, J., Li, D., Yang, R. et al. Outcome of surgical treatment of children and adolescents with primary malignant sacral tumours. International Orthopaedics (SICOT) 44, 1841–1851 (2020). https://doi.org/10.1007/s00264-020-04641-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-020-04641-7