Abstract
Purpose
Cardiovascular complications constitute morbidity and mortality for hip fracture patients. Relatively little data exist exploring risk factors for post-operative complications. Using the American College of Surgeons National Surgical Quality Improvement (ACS-NSQIP) database, we identified significant risk factors associated with adverse cardiac events in hip fracture patients and provide recommendations for practising orthopaedists.
Methods
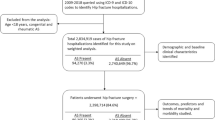
A cohort of 27,441 patients with hip fractures from 2006 to 2013 was identified using Current Procedural Terminology codes. Cardiac complications were defined as cardiac arrests or myocardial infarctions occurring within 30 days after surgery. Bivariate analysis was run on over 30 patient and surgical factors to determine significant associations with cardiac events. Multivariate logistical analysis was then performed to determine risk factors most predictive for cardiac events.
Results
Of the 27,441 hip fracture patients, 594 (2.2 %) had cardiac complications within 30 days post-operatively. There was no significant association with respect to type of hip fracture surgery and adverse cardiac event rates (p = 0.545). After multivariate analysis, dialysis use (OR: 2.22, p = 0.026), and histories of peripheral vascular disease (OR: 2.11, p = 0.016), stroke (OR: 1.83, p = 0.009), COPD (OR: 1.69, p = 0.014), and cardiac disease (OR: 1.55, p = 0.017) were significantly predictive of post-operative cardiac events in all hip fracture patients.
Conclusion
Orthopaedic trauma surgeons should be aware of cardiac disease history and atherosclerotic conditions (PVD, stroke) in risk stratifying patients to prevent cardiac complications. Our recommendations to reduce cardiac events include simple pre-operative lab-work to full-fledged cardiac work-up and referrals to specific medicine disciplines based on the specific risk factors present.
Similar content being viewed by others
References
Agency for Healthcare Research and Quality (2007) Healthcare cost and utilization project. www.ahrq.gov/data/hcup. Accessed on March 2015
Brauer CA, Coca-Perraillon M, Cutler DM, Rosen AB (2009) Incidence and mortality of hip fractures in the United States. JAMA 302:1573–1579
Stevens JA, Rudd RA (2013) The impact of decreasing US hip fracture rates on future hip fracture estimates. Osteoporos Int 24:2725–2728
Chiang CH, Liu CJ, Chen PJ, Huang CC, Hsu CY, Chen ZY, Chan WL, Huang PH, Chen TJ, Chung CM, Lin SJ, Chen JW, Leu HB (2013) Hip fracture and risk of acute myocardial infarction: a nationwide study. J Bone Miner Res 28:404–411
Golinvaux NS, Bohl DD, Basques BA, Baumgaertner MR, Grauer JN (2015) Diabetes confers little to no increased risk of postoperative complications after hip fracture surgery in geriatric patients. Clin Orthop Relat Res 473:1043–1051
Hietala P, Strandberg M, Strandberg N, Gullichsen E, Airaksinen KE (2013) Perioperative myocardial infarctions are common and often unrecognized in patients undergoing hip fracture surgery. J Trauma Acute Care Surg 74:1087–1091
Chen Y, Yang X, Meng K, Zeng Z, Ma B, Liu X, Qi B, Cui S, Cao P, Yang Y (2013) Stress-induced hyperglycemia after hip fracture and the increased risk of acute myocardial infarction in nondiabetic patients. Diabetes Care 36:3328–3332
Daveport DL, Ferraris VA, Hosokawa P, Henderson WG, Khuri SF, Mentzer RM Jr (2007) Multivariable predictors of postoperative cardiac adverse events after general and vascular surgery: results from the patient safety in surgery study. J Am Coll Surg 204:1199–1210
User Guide for the 2010 ACS NSQIP Participant Use Data File (2012). ACS NSQIP. http://site.acsnsqip.org/wp-content/uploads/2013/10/ACSNSQIP.PUF_.UserGuide.2012.pdf. Accessed April 2015
Huddleston JM, Gullerud RE, Smither F, Huddleston PM, Larson DR, Phy MP, Melton LJ 3rd, Roger VL (2012) Myocardial infarction after hip fracture: a population-based study. J Am Geriatr Soc 60:2020–2026
Talsnes O, Hjelmstedt F, Dahl OE, Pripp AH, Reikerås O (2011) Clinical and biochemical prediction of early fatal outcome following hip fracture in the elderly. Int Orthop 35:903–907
Sathiyakumar V, Greenberg SE, Molina CS, Thakore RV, Obremskey WT, Sethi MK (2015) Hip fractures are risky business: an analysis of NSQIP data. Injury 46(4):703–708. doi:10.1016/j.injury.2014.10.051
Khan MA, Hossain FS, Ahmed I, Muthukumar N, Mohsen A (2013) Predictors of early mortality after hip fracture surgery. Int Orthop 37:2119–2124
Menendez ME, Memtsoudis SG, Opperer M, Boettner F, Gonzalez Della Valle A (2015) A nationwide analysis of risk factors for in-hospital myocardial infarction. Int Orthop 4:777–786
Katsanos S, Babalis D, Kafkas N, Mavrogenis A, Leong D, Parissis J, Varounis C, Makris K, van der Heijden A, Anastasiou-Nana M, Filippatos G (2015) B-type natriuretic peptide vs. cardiac risk scores for prediction of outcome following major orthopedic surgery. J Cardiovasc Med (Hagerstown) 16(6):465–471
Campo G, Pavasini R, Malagu M, Mascetti S, Biscaglia S, Ceconi C, Papi A, Contoli M (2015) Chronic obstructive pulmonary disease and ischemic heart disease comorbidity: overview of mechanisms and clinical management. Cardiovasc Drugs Ther 29(2):147–157. doi:10.1007/s10557-014-6569-y
Licker M, Schweizer A, Ellenberger C, Tschopp J-M, Diaper J, Clergue F (2007) Perioperative medical management of patients with COPD. Int J Chron Obstruct Pulmon Dis 2:493–515
Choi HY, Park HC, Ha SK (2014) How do we manage coronary artery disease in patients with CKD and ESRD? Electrolyte Blood Press 12:41–54
Khanagavi J, Gupta T, Aronow WS, Shah T, Garg J, Ahn C, Sule S, Peterson S (2014) Hyperkalemia among hospitalized patients and association between duration of hyperkalemia and outcomes. Arch Med Sci 10:251–257
Rossi E, Biasucci LM, Citterio F, Pelliccioni S, Monaco C, Ginnetti F, Angiolillo DJ, Grieco G, Liuzzo G, Maseri A (2002) Risk of myocardial infarction and angina in patients with severe peripheral vascular disease: role of C-reactive protein. Circulation 105:800–803
Jorgensen ME, Torp-Pedersen C, Gislason GH, Jensen F, Berger SM, Christiansen CB, Overgaard C, Schmiegelow MD, Andersson C (2014) Time elapsed after ischemic stroke and risk of adverse cardiovascular events and mortality following elective noncardiac surgery. JAMA 312:269–277
Mansour J, Graf K, Lafferty P (2012) Bleeding disorders in orthopedic surgery. Orthopedics 35:1053–1062
Robinson TN, Eiseman B (2008) Postoperative delirium in the elderly: diagnosis and management. Clin Interv Aging 3:351–355
Grimes JP, Gregory PM, Noveck H, Butler MS, Carson JL (2002) The effects of time-to-surgery on mortality and morbidity in patients following hip fracture. Am J Med 112:702–709
Orosz GM, Magaziner J, Hannan EL, Morrison RS, Koval K, Gilbert M et al (2004) Association of timing of surgery for hip fracture and patient outcomes. JAMA 291:1738–1743
Antonova E, Boye ME, Sen N, O’Sullivan AK, Burge R (2015) Can bundled payment improve quality and efficiency of care for patients with hip fractures? J Aging Soc Policy 27:1–20
Conflicts of interest
Author William Obremskey has previously consulted for biometrics, done expert testimony in legal matters, has a grant from the Department of Defense, and has been a Board Member of the OTA and SEFC.
The remaining authors have no competing interests to declare.
Ethical review committee statement and approval
This study was performed in accordance with the relevant regulations of the US Health Insurance Portability and Accountability Act (HIPAA) and the ethical standards of the 1964 Declaration of Helsinki. The protocol was approved by the Vanderbilt Institutional Review Board.
This study used no previously copyrighted materials or signed patient consent forms.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Author information
Authors and Affiliations
Corresponding author
Appendix: Patient factors included in analysis
Appendix: Patient factors included in analysis
Patient demographics |
Age (>65 years vs <65 years), gender (male vs. female), and race (Caucasian, African American, Asian, other) |
Preoperative patient comorbidities |
History of chronic obstructive pulmonary disease (COPD), diabetes, cigarette use, ventilator use, ascites, disseminated cancer, wound infections, steroid use, weight loss, bleeding disorder, alcohol use, pneumonia, varices, hypertension requiring medications, peripheral vascular disease (PVD), rest pain as a result of peripheral vascular occlusion, renal failure, dialysis use, altered sensorium, coma, hemiplegia, paraplegia, quadriplegia, transient ischemic attack (TIA), cerebral vascular accident (CVA), CNS tumour, transfusion, radiation therapy, chemotherapy, dyspnea, and sepsis |
Surgical factors |
ASA score (1–2 vs 3–4), type of anaesthesia (general vs. other), do not resuscitate (DNR) status, operation within the previous 30 days, and whether the case was deemed emergent (based on timing of between operation and diagnosis reported by the surgeon which usually occurred within 48 h of hospitalization) |
Rights and permissions
About this article
Cite this article
Sathiyakumar, V., Avilucea, F.R., Whiting, P.S. et al. Risk factors for adverse cardiac events in hip fracture patients: an analysis of NSQIP data. International Orthopaedics (SICOT) 40, 439–445 (2016). https://doi.org/10.1007/s00264-015-2832-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-015-2832-5