Abstract
Background
Hip fractures frequently necessitate hospitalization, especially among patients aged 75 and above who might concurrently suffer from aortic stenosis (AS). This study focuses on postoperative outcomes, potential determinants of morbidity and mortality, as well as evolving trends in patients with AS undergoing surgical repair of hip fractures.
Methods
A retrospective analysis of the Nationwide Inpatient Sample from 2008 to 2019 was conducted. Hip fracture cases were identified, and a subgroup with AS was isolated using the ICD-9 and ICD-10 diagnostic codes. We compared baseline characteristics, postoperative in-hospital outcomes and trends in mortality and morbidity between patients with and without AS.
Results
From the dataset, 2,834,919 patients with hip fracture were identified on weighted analysis. Of these, 94,270 (3.3%) were found to have concurrent AS. The AS cohort was characterized by higher mean age and elevated burden of cardiovascular comorbidities, such as coronary artery disease, peripheral vascular disease, pulmonary hypertension, congestive heart failure and cardiac arrhythmias. Postoperative mortality following hip fracture surgery was greater in the AS groups compared to non-AS group (3.3% vs 1.57%, p < 0.001). Risk factors such as congestive heart failure (OR, 2.3[CI, 2.1–2.6]), age above 85 years (OR, 3.2[CI, 2.2–4.7]), cardiac arrhythmias (OR, 2.4[CI, 2.2–2.6]), end-stage renal disease (OR, 3.4[CI, 2.7–4.1]), malnutrition (OR, 2.3[CI, 2.1–2.7]) and AS (OR, 1.2[CI, 1.08–1.5] were associated with increased adjusted odds of postoperative mortality. AS was linked to higher adjusted odds of postoperative mortality (OR, 1.2 [CI, 1.1–1.5]) and complications such as acute myocardial infarction (OR, 1.2 [CI, 1.01–1.4]), cardiogenic shock (OR, 2.0[CI, 1.4–2.9]) and acute renal failure (OR, 1.1[CI, 1.02–1.2]). While hospital stay duration was comparable in both groups (average 5 days), the AS group incurred higher costs (mean $50,673 vs $44,607). The presence of acute heart failure in patients with AS and hip fracture significantly increased mortality, hospital stay, and cost. A notable decline in postoperative in-hospital mortality was observed in both groups from 2008–2019 though the rate of major in-hospital complications rose.
Conclusion
AS significantly influences postoperative in-hospital mortality and complication rates in hip fracture patients. While a reduction in postoperative mortality was observed in both AS and non-AS cohorts, the incidence of major in-hospital complications increased across both groups.
Similar content being viewed by others
Introduction/Background
Hip fractures, representing a significant orthopedic emergency, are a common cause of hospitalization. With an annual incidence of over 340,000 fractures [1], the United States (US) has one of the highest hip fracture rates in the world [2]. The incidence of hip fractures is estimated to double worldwide by 2025 [3], mainly affecting the elderly population, particularly those aged 75 years and above [1, 4,5,6,7]. This patient population is also burdened with an elevated prevalence of cardiovascular comorbidities [8], of which aortic stenosis (AS) is the predominant valvular heart disease [9, 10].
Surgery is the principal treatment approach for hip fractures [11]. However, the presence of concurrent AS can increase the risk of perioperative major cardiovascular events and mortality [12,13,14]. Existing literature on the outcomes of patients with AS undergoing hip fracture surgery has produced inconsistent findings. In a retrospective study by Adunsky et al [15] on elderly patients with mean age of 86 years, AS was associated with high in-hospital postoperative mortality and major complications. Keswani et al [16] reported increased risk of perioperative complications and mortality in patients ≥ 65 years of age with moderate to severe AS undergoing hip fracture surgical treatment. Similar results are published by Rostagno et al in patients with severe AS [17]. Conversely, another case–control study did not manifest significant differences in 30-days mortality (6.2% vs 6.8%) between severe AS group and controls [18]. These single center studies are performed on elderly population with moderate to severe AS only, underscoring the need for further investigation into the association of AS with hip fracture postoperative outcomes and mortality on nationally representative data, as it can inform the guidelines for improved outcomes for this patient population.
The objective of this study was to analyze the postoperative outcomes, predictors and trends of in-hospital mortality in patients undergoing hip fracture surgery who had concomitant AS, using data from the Nationwide Inpatient Sample (NIS).
Methods
Study sample and design
We conducted a retrospective cohort study using the NIS database from 2008–2019. It is the largest publicly available all-payer inpatient healthcare database that is designed to produce US regional and national estimates of inpatient utilization, access, cost, quality and outcomes [19]. Unweighted, it contains data from more than 7 million hospital stays annually. Weighted, it estimates more than 35 million hospitalizations nationally. As data are deidentified and publicly available, this study is exempted from approval by the institutional review board.
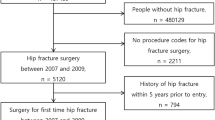
Hip fracture hospitalizations were identified in the database using International Classification for disease (ICD) 9 and 10 diagnostic codes. Within the hip fracture group, a subgroup of AS was created using ICD codes (424.1, I35.0). We excluded cases with rheumatic and congenital AS (Fig. 1). Patients under the age of 18 years were also excluded from this study. Baseline demographic characteristics, including age, sex and race, are available in the dataset. Comorbidities were identified from the database using ICD 9 and 10 diagnostic codes and Charlson comorbidities as reported in the HCUP dataset (Supplementary table 1).
Within the hip fracture patient population, a subgroup of clinically significant AS was created by identifying patients who had both AS and acute or AS and acute on chronic congestive heart failure (CHF) within the same hospitalization using ICD-9 and ICD-10 diagnostic codes.
We adhered to Nationwide Database Data Use Agreement (DUA) while conducting this analysis.
Study outcomes
The primary outcome was inpatient all-cause mortality. The secondary outcomes included acute myocardial infarction (AMI), acute pulmonary edema, cardiogenic shock, acute deep venous thrombosis/pulmonary embolism (DVT/PE), septic shock, pneumonia, acute respiratory failure, acute ischemic & hemorrhagic cerebrovascular accident (CVA), acute renal failure, acute delirium, postoperative surgical site infection (SSI) and postoperative bleeding.
Statistical analysis
Continuous variables were reported as the mean with standard deviation (SD) or median with interquartile range (IQR). Linear regression was used to compare weighted estimates of continuous variables. Categorical variables were reported as proportions and compared using Pearson’s chi-square test.
A multivariable logistic regression model was developed to determine independent predictors of inpatient mortality in all hip fracture patients while adjusting for demographics (age, sex, race) and comorbidities: hypertension, diabetes mellitus (DM), smoking, coronary artery disease (CAD), CHF, cardiac arrhythmias, long-term anticoagulation use, end-stage renal disease (ESRD), AS, malnutrition, alcohol use disorder, chronic obstructive pulmonary disease (COPD), dementia, vitamin D deficiency and osteoporosis.
Another multivariable logistic regression model was developed to determine the association of AS with postoperative outcomes while adjusting for age, sex, race and the following comorbid conditions: pulmonary hypertension, ESRD, chronic kidney disease (CKD), dementia, CAD, smoking status, obesity, AS, osteoporosis, DM, hypertension, COPD, cardiac arrhythmias, long-term use of anticoagulation, vitamin D deficiency, alcoholism, and malnutrition.
Odds ratios (ORs) and 95% confidence intervals (CIs) were reported. Yearly trends of postoperative mortality and morbidity were studied and reported as percentages. Temporal trends were demonstrated graphically, linear trends were calculated using the Cochrane Armitage method, and p-trends were reported. Survey analysis methodology using weights of hospital-level discharge from NIS was used to calculate nationally representative estimates.
Inflation-adjusted total hospital cost was calculated from total charges and cost-to-charge files available from the healthcare cost and utilization project (HCUP) website.
A P value < 0.05 was considered statistically significant. We used Stata v. 17.0 (StataCorp, Longview, TX) for all statistical analyses.
Results
Demographics and baseline characteristics
Over the study period of 2008–2019, a total of 2,834,919 (mean (SD) age 77.3 (12.9), 68% females, 85.6% whites) patients with a primary diagnosis of hip fracture were hospitalized in the US. Of these, 94,270 (3.3%) had a concomitant diagnosis of AS. A total of 84.6% of hospitalized patients with hip fracture underwent surgery. Of the patients who underwent surgery for hip fracture, 80,305 (3.3%) had a concomitant diagnosis of AS.
Patients who had hip fracture and AS were more likely to be older (62% being 85 years or older) and female (68%) and had a higher prevalence of comorbidities such as DM, hypertension, CAD, cardiac arrhythmias, long-term anticoagulation use, pulmonary hypertension, CKD, ESRD and dementia. A total of 87.2% of hip fracture hospitalizations were noted in large urban hospitals (Table 1).
Hip fracture surgery postoperative outcomes in patients with underlying AS
In patients undergoing hip fracture surgery who had underlying AS, 2,665 (3.3%) deaths occurred compared to 36,330 (1.57%) deaths in patients without underlying AS.
Patients with AS had more in-hospital complications, including AMI (3.97% vs 1.57%, p < 0.001), acute pulmonary edema (0.33% vs 0.16%, p < 0.001), cardiogenic shock (0.60% vs 0.16%, p < 0.001), pneumonia (7.5% vs 5.6% p < 0.001), acute respiratory failure (8.8% vs 6.0% p < 0.001), acute ischemic CVA (5.1% vs 2.71% p < 0.001) and acute renal failure (18.8% vs 12.6 p < 0.001) (Table 2).
There was no statistically significant difference in the length of hospitalization between groups.
In a multivariable logistic regression model, AS was independently associated with mortality (aOR 1.28; 95% CI 1.08–1.51, p = 0.003) among patients who underwent hip fracture surgery.
Other significant predictors of mortality were age > 85 years (p < 0.001), pulmonary hypertension (p < 0.001), CKD (p < 0.001), ESRD (p < 0.001), CHF (p < 0.001) and malnutrition (p < 0.001). In the adjusted analysis, CAD was not identified as a predictor of mortality (p = 0.69) (Table 3, Fig. 2).
In hip fracture patients with AS undergoing surgery, AS was associated with higher adjusted odds of mortality (aOR, 1.2 [CI, 1.1–1.50], p = 0.004), AMI (aOR, 1.2 [CI, 1.0–1.4], p = 0.030), cardiogenic shock (aOR, 2.0 [CI, 1.4–2.9] p < 0.001), and acute renal failure (aOR, 1.1 [CI, 1.0–1.19], p = 0.008) compared to the group undergoing hip fracture surgery without concomitant AS. In the adjusted analysis, AS was not statistically associated with acute pulmonary edema, pneumonia, septic shock, acute DVT/PE, acute postoperative bleeding, and acute delirium (Table 4).
Postoperative outcomes in patients with underlying clinically significant AS
In patients who underwent hip fracture surgery and had AS with acutely decompensated CHF in the same hospitalization, 485 (9.4%) deaths occurred compared to 38,510 (1.6%) among hip fracture surgery patients without AS. There was a higher prevalence of AMI (13.5% vs. 1.6%, p < 0.001), acute pulmonary edema (0.7% vs 0.16%, p < 0.001), acute respiratory failure (34% vs 6%, p < 0.001) and other in-hospital complications, such as septic shock, pneumonia, acute ischemic CVA, acute delirium and cardiogenic shock, compared to the group undergoing hip fracture surgery without underlying clinically significant AS. Additionally, the length of hospitalization was higher in the former group than the latter group (Supplementary Table 3).
Mortality and morbidity trends
In the study period of 2008 to 2019, there was a statistically significant (p-trend < 0.05) decline in hip fracture postoperative mortality in patients with and without AS (Fig. 3). There was an increase in the rate of one or more major postoperative complications in both groups (Fig. 4).
Discussion
To our knowledge, this is the most comprehensive study of hospitalized hip fracture patients who underwent surgery with concomitant AS. We found that AS with hip fracture is common and was present in 3.3% of hospitalized patients. The in-hospital postoperative mortality rate of these patients was 3.3%. Notably, this rate decreased from 3.7% in 2008 to 2.7% in 2019 (p for trend < 0.05).
A significant proportion of patients (37.6%) experienced at least one major complication following hip fracture surgery. Importantly, AS was an independent predictor of postoperative in-hospital mortality. This association was particularly strong among AS patients with acutely decompensated CHF.
In population-based studies, some degree of AS is present in 1 in 10 patients aged over 75 years [21]. In our cohort of hospitalized patients with hip fracture, 1 in 30 had AS, and the prevalence was much higher in patients above 75 years of age. This is likely because our study is based on only hospitalized hip fracture patients. AS patients had higher burden of comorbidities in this study. CAD was present in 40% of hospitalized AS patients with hip fracture, which is in agreement with other studies where 44–50% of AS patients had underlying CAD [22, 23]. However, our study did not identify CAD as an independent predictor of postoperative mortality in AS patients. This finding might be attributed to the shared risk factors between AS and CAD. Patients are also routinely evaluated for CAD perioperatively due to its association with 30-day postoperative mortality [24] in both cardiac and noncardiac surgery, but evaluation of AS is not routinely performed perioperatively.
Progression of AS can lead to the development of decompensated CHF [25]. Within this study, 0.21% of all AS patients with hip fracture had acute or acute on chronic CHF. This subgroup experienced significantly higher postoperative in-hospital mortality and morbidity rates than AS patients without acute CHF. Patients may develop pulmonary hypertension (PH) with increasing severity of AS, a significant risk factor for postoperative mortality in noncardiac surgery. A study by Cignoni et al. [26] reported 2.5 times higher in-hospital mortality for patients undergoing hip fracture surgery with both AS and PH compared to patients with AS alone. In this study, PH in the adjusted analysis was independently associated with postoperative mortality (aOR 1.34, p < 0.001) in AS patients.
In one retrospective case–controlled review of elderly (≥ 65 years) hip fracture patients treated surgically, moderate/severe AS and pulmonary and renal diseases were identified as independent predictors of severe 30-day postoperative complications [16]. Our study corroborates these findings, with the strongest association of in-hospital mortality noted with age ≥ 85 years.
CKD and ESRD [27] are known risk factors for perioperative adverse cardiovascular events and postoperative mortality. They can predispose patients to changes in the sodium and fluid balance, vascular calcification, and inflammatory changes leading to atherosclerotic plaque destabilization [28]. In this analysis, both CKD (aOR 1.44, p < 0.001) and ESRD (aOR 3.40, p < 0.001) were associated with higher odds of postoperative mortality in AS patients. Malnutrition and poor functional status are associated with poor outcomes after hip fracture surgery. Malnourished patients are 7 times more likely to suffer complications and have a higher length of hospitalization than non-malnourished patients when admitted to the hospital with acetabular fracture and undergo surgery [29]. In our study, 5.7% of all patients admitted with hip fracture were malnourished, which was associated with higher odds of postoperative mortality (aOR 2.38, p < 0.001). The identification of malnutrition and benefits of nutritional interventions in hospitalized patients with hip fracture are not well studied.
Postoperative mortality in hip fracture patients with AS decreased in this study period from 2008–2019 (p-trend < 0.05). In the AHA/ACC guidelines on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery [14], the use of 3 calculators [24, 30, 31] to assess a patient’s surgical risk is recommended. These risk calculators use different comorbidities as variables to calculate surgical risk; however, none of them take into consideration aortic valve function.
AS patients requiring noncardiac surgery pose a clinical challenge due to their higher mortality risk and likelihood of perioperative complications. This patient cohort could benefit from careful preoperative assessment, management of comorbid conditions, and surgical optimization through a multidisciplinary team. A careful preoperative assessment of volume status and invasive hemodynamic monitoring intraoperatively, especially in patients who have developed CHF and pulmonary hypertension from moderate to severe AS, can lead to improved outcomes.
According to the European Society of Cardiology preoperative cardiovascular disease management guidelines [32], asymptomatic patients with severe AS preparing for noncardiac surgery should be evaluated for potential aortic valve replacement, either surgical or transcatheter (Class IIa recommendation). Transcatheter aortic valve implantation (TAVI) in recent years has been identified as a minimally invasive option with improved outcomes in patients at higher surgical replacement risk [33]. However, utilization of TAVI and percutaneous balloon aortic valvuloplasty (BAV) in moderate to severe AS patients during the perioperative period for time-sensitive intermediate cardiac risk surgeries, such as hip fracture, remains understudied [34]. In this cohort, very few patients with hip fracture underwent TAVI in the same hospitalization. We were unable to determine if TAVI in high-risk patients before hip fracture surgery improves postoperative outcomes due to the absence of AS severity data in the NIS dataset. Given the increased postoperative mortality and morbidity rates associated with delays in hip fracture surgery [35,36,37], further research should investigate how deferring surgery for endovascular procedures such as TAVI or BAV may influence these outcomes. This highlights the importance of understanding the potential impacts of treatment timing on patient outcomes in this complex clinical scenario.
Strengths and limitations of the study
In this retrospective cohort study on a large inpatient dataset, demographic features and comorbidities were taken into consideration while studying factors predicting outcomes such as in-hospital mortality and postoperative complications. We excluded patients with rheumatic and congenital AS from this analysis, as their presentation and course may differ from those of patients with calcific and age-related AS. The HCUP NIS database, however, does not specify the severity of AS by providing the valve area. To identify patients with clinically significant AS, we studied patients who had acutely decompensated CHF diagnosis while hospitalized for hip fracture and had underlying AS, which may over- or underestimate the actual severity of AS in this group of patients. Each patient in the NIS database represents an index hospitalization. This sample is not designed to follow patients longitudinally; hence, long-term outcomes such as mortality, complications after discharge and rate of readmissions cannot be studied. NIS identifies the diagnosis based on the ICD coding system, which may be subject to error; however, we identified the codes for conditions that are frequently used in inpatient settings. The timeline of events is not provided in the NIS dataset hence we are cautiously reporting association of variables with outcomes rather than causation.
Conclusion
Patients with AS who undergo hip fracture surgery exhibit significantly higher in-hospital mortality and morbidity rates than non-AS patients. Although our study from 2008–2019 documented a decline in postoperative mortality among AS patients with hip fracture, the occurrence of in-hospital complications appears to be on the rise. A multidisciplinary approach is needed to identify high-risk patients, risk stratify and medically optimize them for surgery to reduce mortality and postoperative complications. Studies are required to discern whether deferring hip fracture surgery for procedures such as TAVI or percutaneous BAV in high-risk AS patients influences postoperative mortality and outcomes.
Availability of data and materials
The dataset analyzed during the current study is available at the HCUP website: https://hcup-us.ahrq.gov/
Abbreviations
- AS:
-
Aortic stenosis
- NIS:
-
Nationwide inpatient sample
- SD:
-
Standard deviation
- IQR:
-
Interquartile range
- ICD:
-
International classification for disease
- CHF:
-
Congestive heart failure
- AMI:
-
Acute myocardial infarction
- DVT:
-
Deep venous thrombosis
- PE:
-
Pulmonary embolism
- CVA:
-
Cerebrovascular accident
- COPD:
-
Chronic obstructive pulmonary disease
- SSI:
-
Surgical site infection
- CKD:
-
Chronic kidney disease
- ESRD:
-
End-stage renal disease
- CAD:
-
Coronary artery disease
- DM:
-
Diabetes mellitus
- OR:
-
Odds ratio
- aOR:
-
Adjusted odds ratio
- CI:
-
Confidence interval
- TAVI:
-
Transcatheter aortic valve implantation
- BAV:
-
Balloon aortic valvuloplasty
References
Brauer CA, Coca-Perraillon M, Cutler DM, Rosen AB. Incidence and mortality of hip fractures in the United States. JAMA. 2009;302(14):1573–9.
Dhanwal DK, Dennison EM, Harvey NC, Cooper C. Epidemiology of hip fracture: worldwide geographic variation. Indian J Orthop. 2011;45(1):15–22.
Gullberg B, Johnell O, Kanis JA. World-wide projections for hip fracture. Osteoporos Int. 1997;7(5):407–13.
Chang KP, Center JR, Nguyen TV, Eisman JA. Incidence of hip and other osteoporotic fractures in elderly men and women: Dubbo osteoporosis epidemiology study. J Bone Miner Res Off J Am Soc Bone Miner Res. 2004;19(4):532–6.
Remily EA, Mohamed NS, Wilkie WA, Mahajan AK, Patel NG, Andrews TJ, et al. Hip fracture trends in America between 2009 and 2016. Geriatr Orthop Surg Rehabil. 2020;11:2151459320929581.
Sullivan KJ, Husak LE, Altebarmakian M, Brox WT. Demographic factors in hip fracture incidence and mortality rates in California, 2000–2011. J Orthop Surg. 2016;11(1):4.
Cooper C, Campion G, Melton LJ. Hip fractures in the elderly: a world-wide projection. Osteoporos Int J Establ Result Coop Eur Found Osteoporos Natl Osteoporos Found USA. 1992;2(6):285–9.
Sennerby U, Melhus H, Gedeborg R, Byberg L, Garmo H, Ahlbom A, et al. Cardiovascular diseases and risk of hip fracture. JAMA. 2009;302(15):1666–73.
Osnabrugge RLJ, Mylotte D, Head SJ, Van Mieghem NM, Nkomo VT, LeReun CM, et al. Aortic stenosis in the elderly: disease prevalence and number of candidates for transcatheter aortic valve replacement: a meta-analysis and modeling study. J Am Coll Cardiol. 2013;62(11):1002–12.
Nkomo VT, Gardin JM, Skelton TN, Gottdiener JS, Scott CG, Enriquez-Sarano M. Burden of valvular heart diseases: a population-based study. The Lancet. 2006;368(9540):1005–11.
Ossendorf C, Scheyerer MJ, Wanner GA, Simmen HP, Werner CM. Treatment of femoral neck fractures in elderly patients over 60 years of age - which is the ideal modality of primary joint replacement? Patient Saf Surg. 2010;4:16.
Kertai MD, Bountioukos M, Boersma E, Bax JJ, Thomson IR, Sozzi F, et al. Aortic stenosis: an underestimated risk factor for perioperative complications in patients undergoing noncardiac surgery. Am J Med. 2004;116(1):8–13.
Agarwal S, Rajamanickam A, Bajaj NS, Griffin BP, Catacutan T, Svensson LG, et al. Impact of aortic stenosis on postoperative outcomes after noncardiac surgeries. Circ Cardiovasc Qual Outcomes. 2013;6(2):193–200.
Fleisher LA, Fleischmann KE, Auerbach AD, Barnason SA, Beckman JA, Bozkurt B, et al. 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and Management of Patients Undergoing Noncardiac Surgery: a report of the American College of Cardiology/American Heart Association task force on practice guidelines. J Am Coll Cardiol. 2014;64(22):e77-137.
Adunsky A, Kaplan A, Arad M, Mizrahi EH, Gottlieb S. Aortic stenosis in elderly hip fractured patients. Arch Gerontol Geriatr. 2008;46(3):401–8.
Keswani A, Lovy A, Khalid M, Blaufarb I, Moucha C, Forsh D, et al. The effect of aortic stenosis on elderly hip fracture outcomes: a case control study. Injury. 2016;47(2):413–8.
Rostagno C, Cartei A, Rubbieri G, Ceccofiglio A, Civinini R, Curcio M, et al. Hip fracture surgery in severe aortic stenosis: a study of factors affecting mortality. Clin Interv Aging. 2022;17:1163–71.
Leibowitz D, Rivkin G, Schiffman J, Rott D, Weiss AT, Mattan Y, et al. Effect of severe aortic stenosis on the outcome in elderly patients undergoing repair of hip fracture. Gerontology. 2009;55(3):303–6.
HCUP-US NIS Overview [Internet]. [cited 2022 Aug 15]. Available from: https://www.hcup-us.ahrq.gov/nisoverview.jsp
Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8.
Eveborn GW, Schirmer H, Heggelund G, Lunde P, Rasmussen K. The evolving epidemiology of valvular aortic stenosis. The tromsø study. Heart. 2013;99(6):396–400.
Faggiano P, Frattini S, Zilioli V, Rossi A, Nistri S, Dini FL, et al. Prevalence of comorbidities and associated cardiac diseases in patients with valve aortic stenosis. Potential implications for the decision-making process. Int J Cardiol. 2012;159(2):94–9.
Kodali SK, Moses JW. Coronary artery disease and aortic stenosis in the transcatheter aortic valve replacement era. Circulation. 2012;125(8):975–7.
Lee TH, Marcantonio ER, Mangione CM, Thomas EJ, Polanczyk CA, Cook EF, et al. Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation. 1999;100(10):1043–9.
Généreux P, Pibarot P, Redfors B, et al. Staging classification of aortic stenosis based on the extent of cardiac damage. Eur Heart J. 2017;38(45):3351–8.
Cignoni CB, Vuu SKM, Liu H, Clark JM, Watson CD, Ferber LR, et al. Increased mortality in hip fracture patients with aortic stenosis and pulmonary hypertension compared to aortic stenosis alone. Am Surg. 2021;00031348211054525.
Palamuthusingam D, Johnson DW, Hawley CM, Pascoe E, Sivalingam P, Fahim M. Perioperative outcomes and risk assessment in dialysis patients: current knowledge and future directions. Intern Med J. 2019;49(6):702–10.
Briasoulis A, Bakris GL. Chronic kidney disease as a coronary artery disease risk equivalent. Curr Cardiol Rep. 2013;15(3):340.
Zamanzadeh RS, Aspang JS, Bonsu JM, Maceroli MA, Boissonneault A. Malnutrition is associated with 30-day postoperative complications and increased length of hospital stay in patients with surgically treated acetabular fractures. J Am Coll Surg. 2022;235(5):S165.
Cohen ME, Ko CY, Bilimoria KY, Zhou L, Huffman K, Wang X, et al. Optimizing ACS NSQIP modeling for evaluation of surgical quality and risk: patient risk adjustment, procedure mix adjustment, shrinkage adjustment, and surgical focus. J Am Coll Surg. 2013;217(2):336-346.e1.
Gupta PK, Gupta H, Sundaram A, Kaushik M, Fang X, Miller WJ, et al. Development and validation of a risk calculator for prediction of cardiac risk after surgery. Circulation. 2011;124(4):381–7.
Halvorsen S, Mehilli J, Cassese S, Hall TS, Abdelhamid M, Barbato E, et al. 2022 ESC guidelines on cardiovascular assessment and management of patients undergoing non-cardiac surgery: developed by the task force for cardiovascular assessment and management of patients undergoing non-cardiac surgery of the European Society of Cardiology (ESC) endorsed by the European Society of Anaesthesiology and Intensive Care (ESAIC). Eur Heart J. 2022;43(39):3826–924.
Popma JJ, Adams DH, Reardon MJ, Yakubov SJ, Kleiman NS, Heimansohn D, et al. Transcatheter aortic valve replacement using a self-expanding bioprosthesis in patients with severe aortic stenosis at extreme risk for surgery. J Am Coll Cardiol. 2014;63(19):1972–81.
Rostagno C, Falchetti G, Rostagno AC, Mattesini A. TAVR in patients with hip fracture and severe aortic stenosis: how and when? Intern Emerg Med. 2021;16(6):1419–22.
Moran CG, Wenn RT, Sikand M, Taylor AM. Early mortality after hip fracture: is delay before surgery important? JBJS. 2005;87(3):483.
Pincus D, Ravi B, Wasserstein D, Huang A, Paterson JM, Nathens AB, et al. Association between wait time and 30-day mortality in adults undergoing hip fracture surgery. JAMA. 2017;318(20):1994–2003.
Klestil T, Röder C, Stotter C, Winkler B, Nehrer S, Lutz M, et al. Impact of timing of surgery in elderly hip fracture patients: a systematic review and meta-analysis. Sci Rep. 2018;8(1):13933.
Acknowledgements
Thankful to Waqas T. Qureshi, MD of UMass Medical Center, Worcester, MA for supervision of data analysis and manuscript development.
Funding
None.
Author information
Authors and Affiliations
Contributions
SH: Conceptualization, Methodology, Formal data collection and analysis, Writing - Original draft, Revision. WA: Methodology, Visualization, Writing – Review and Editing. SM: Formal data collection and analysis, Writing – Review and Editing. MIH: Formal data analysis, Visualization, Supervision. AK: Writing – Review and editing, supervision. AJB: Conceptualization, Writing Review and Editing, Visualization, Supervision.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
As this analysis was conducted on publicly available deidentified data, it was exempted from ethics committee approval.
Consent for publication
Not applicable.
Competing interests
Dr. Blood receives grant support from Novo Nordisk, Boehringer Ingelheim, and General Electric Healthcare and consulting income from Color Health and Walgreens Health, and equity in Knownwell Inc. All other authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary Table 1.
ICD 9 and ICD 10 codes. Supplementary Table 2. Baseline characteristics of hip fracture patients undergoing surgery. Supplementary Table 3. Outcomes post hip fracture surgery stratified by clinically significant AS (Acute CHF with AS).
Additional file 2:
Supplementry Table 4. Checklist for working with the NIS.
Additional file 3: Supplementary Table 5.
The RECORD statement – checklist of items, extended from the STROBE statement that should be reported in observational studies using routinely collected health data.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hassan, S., Anwar, W., Mehta, S. et al. Postoperative outcomes, predictors and trends of mortality and morbidity in patients undergoing hip fracture surgery with underlying aortic stenosis: a nationwide inpatient sample analysis. BMC Cardiovasc Disord 23, 535 (2023). https://doi.org/10.1186/s12872-023-03584-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-023-03584-2