Abstract
Introduction
Brain metastases are a significant source of morbidity and mortality for patients with lung cancer. Lung cancer can induce local and systemic immunosuppression, promoting tumor growth and dissemination. One mechanism of immunosuppression is tumor-induced expansion of programmed death-ligand 1 (PD-L1) expressing myeloid cells. Here, we investigate peripheral blood immune phenotype in NSCLC patients with or without brain metastasis.
Methods
Peripheral blood was collected from patients with lung metastatic brain tumors and pre-metastatic lung cancer. Immunosuppressive monocytes, myeloid-derived suppressor cells (MDSCs), and regulatory T cells (Tregs) were quantified through flow cytometry. T cell reactivity was analyzed via ELISpot. Brain metastasis conditioned media was collected from tumor-derived cell cultures and analyzed for cytokines by ELISA. Naïve monocytes were stimulated with brain metastasis conditioned media to evaluate PD-L1 stimulation.
Results
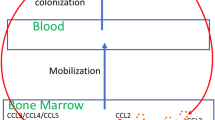
Patients with brain metastatic lung carcinoma demonstrated increased peripheral monocyte PD-L1, MDSC abundance, and Treg percentage compared to early stage pre-metastatic patients and healthy controls. Patients with elevated peripheral monocyte PD-L1 had less reactive T cells and worse survival. Brain metastasis conditioned media stimulation increased monocyte PD-L1, and conditioned media IL-6 levels correlated with PD-L1 induction. Treatment with anti-IL-6 or anti-IL-6 receptor antibodies reduced PD-L1 expression. In summary, patients with lung cancer and brain metastases exhibit multiple markers of peripheral immunosuppression.
Conclusions
The frequency of PD-L1+ myeloid cells correlated with the presence of brain metastases. Tumor-derived IL-6 was capable of inducing PD-L1+ myeloid cells in vitro, suggesting that monitoring of immunosuppressive factors in peripheral blood may identify new targets for therapeutic intervention in selected patients.





Similar content being viewed by others
Abbreviations
- BM:
-
Brain metastasis
- BMCM:
-
Brain metastasis conditioned media
- CTLA-4:
-
Cytotoxic T lymphocyte antigen 4
- ECOG:
-
Eastern Cooperative Oncology Group
- FDA:
-
Food and Drug Administration
- FFPE:
-
Formalin-fixed, paraffin-embedded
- FMO:
-
Fluorescence minus one
- HPFs:
-
High powered fields
- MDSC:
-
Myeloid-derived suppressor cells
- NCI:
-
National Cancer Institute
- NINDS:
-
National Institute of Neurological Disorders and Stroke
- NSCLC:
-
Non-small cell lung cancer
- PBL:
-
Peripheral blood leukocytes
- PBMC:
-
Peripheral blood mononuclear cells
- PD-1:
-
Programmed death 1
- PD-L1:
-
Programmed death-ligand 1
- PFS:
-
Progression-free survival
- PMA:
-
Propidium monoazide
- RECIST:
-
Response evaluation criteria in solid tumors
- SIL:
-
Siltuximab, anti-IL6 antibody
- TCGA:
-
The Cancer Genome Atlas
- TCZ:
-
Tocilizumab, anti-IL6-receptor antibody
- Treg:
-
Regulatory T cell
- TTF-1:
-
Thyroid transcription factor 1
References
Li Y, Lamano J, Lamano JB, Veliceasa D, Kaur G et al (2018) Tumor-induced peripheral immunosuppression promotes brain metastasis in patients with non-small cell lung cancer. J Neurosurg 128(4):961–1272
Siegel RL, Miller KD, Jemal A (2017) Cancer statistics. CA Cancer J Clin 67(1):7–30. https://doi.org/10.3322/caac.21387
Alberg AJ, Ford JG, Samet JM (2007) Epidemiology of lung cancer: ACCP evidence-based clinical practice guidelines (2nd edition). 3 Suppl 132:29–55. https://doi.org/10.1378/chest.07-1347
Schouten LJ, Rutten J, Huveneers HA, Twijnstra A (2002) Incidence of brain metastases in a cohort of patients with carcinoma of the breast, colon, kidney, and lung and melanoma. Cancer 94(10):2698–2705
Arvold ND, Lee EQ, Mehta MP, Margolin K, Alexander BM, Lin NU, Anders CK, Soffietti R, Camidge DR, Vogelbaum MA, Dunn IF, Wen PY (2016) Updates in the management of brain metastases. Neuro Oncol 18(8):1043–1065. https://doi.org/10.1093/neuonc/now127
Borghaei H, Paz-Ares L, Horn L, Spigel DR, Steins M, Ready NE, Chow LQ, Vokes EE, Felip E, Holgado E, Barlesi F, Kohlhaufl M, Arrieta O, Burgio MA, Fayette J, Lena H, Poddubskaya E, Gerber DE, Gettinger SN, Rudin CM, Rizvi N, Crino L, Blumenschein GR Jr, Antonia SJ, Dorange C, Harbison CT, Graf Finckenstein F, Brahmer JR (2015) Nivolumab versus docetaxel in advanced nonsquamous non-small-cell lung cancer. N Engl J Med 373(17):1627–1639. https://doi.org/10.1056/NEJMoa1507643
Massarelli E, Papadimitrakopoulou V, Welsh J, Tang C, Tsao AS (2014) Immunotherapy in lung cancer. Transl Lung Cancer Res 3(1):53–63. https://doi.org/10.3978/j.issn.2218-6751.2014.01.01
Pardoll DM (2012) The blockade of immune checkpoints in cancer immunotherapy. Nat Rev Cancer 12(4):252–264. https://doi.org/10.1038/nrc3239
Brahmer JR, Hammers H, Lipson EJ (2015) Nivolumab: targeting PD-1 to bolster antitumor immunity. Future Oncol 11(9):1307–1326. https://doi.org/10.2217/fon.15.52
Brahmer J, Reckamp KL, Baas P, Crinò L, Eberhardt WEE, Poddubskaya E, Antonia S, Pluzanski A, Vokes EE, Holgado E, Waterhouse D, Ready N, Gainor J, Arén Frontera O, Havel L, Steins M, Garassino MC, Aerts JG, Domine M, Paz-Ares L, Reck M, Baudelet C, Harbison CT, Lestini B, Spigel DR (2015) Nivolumab versus docetaxel in advanced squamous-cell non-small-cell lung cancer. N Engl J Med 373(2):123–135. https://doi.org/10.1056/NEJMoa1504627
Garon EB, Rizvi NA, Hui R, Leighl N, Balmanoukian AS, Eder JP, Patnaik A, Aggarwal C, Gubens M, Horn L, Carcereny E, Ahn MJ, Felip E, Lee JS, Hellmann MD, Hamid O, Goldman JW, Soria JC, Dolled-Filhart M, Rutledge RZ, Zhang J, Lunceford JK, Rangwala R, Lubiniecki GM, Roach C, Emancipator K, Gandhi L (2015) Pembrolizumab for the treatment of non-small-cell lung cancer. N Engl J Med 372(21):2018–2028. https://doi.org/10.1056/NEJMoa1501824
Gettinger SN, Horn L, Gandhi L, Spigel DR, Antonia SJ, Rizvi NA, Powderly JD, Heist RS, Carvajal RD, Jackman DM, Sequist LV, Smith DC, Leming P, Carbone DP, Pinder-Schenck MC, Topalian SL, Hodi FS, Sosman JA, Sznol M, McDermott DF, Pardoll DM, Sankar V, Ahlers CM, Salvati M, Wigginton JM, Hellmann MD, Kollia GD, Gupta AK, Brahmer JR (2015) Overall survival and long-term safety of nivolumab (anti-programmed death 1 antibody, BMS-936558, ONO-4538) in patients with previously treated advanced non-small-cell lung cancer. J Clin Oncol 33(18):2004–2012. https://doi.org/10.1200/jco.2014.58.3708
Herbst RS, Baas P, Kim D-W, Felip E, Pérez-Gracia JL, Han J-Y, Molina J, Kim J-H, Arvis CD, Ahn M-J, Majem M, Fidler MJ, de Castro G Jr, Garrido M, Lubiniecki GM, Shentu Y, Im E, Dolled-Filhart M, Garon EB (2016) Pembrolizumab versus docetaxel for previously treated, PD-L1-positive, advanced non-small-cell lung cancer (KEYNOTE-010): a randomised controlled trial. The Lancet 387(10027):1540–1550. https://doi.org/10.1016/S0140-6736(15)01281-7
Socinski MA, Jotte RM, Cappuzzo F, Orlandi F, Stroyakovskiy D, Nogami N, Rodríguez-Abreu D, Moro-Sibilot D, Thomas CA, Barlesi F, Finley G, Kelsch C, Lee A, Coleman S, Deng Y, Shen Y, Kowanetz M, Lopez-Chavez A, Sandler A, Reck M (2018) Atezolizumab for first-line treatment of metastatic nonsquamous NSCLC. N Engl J Med 378(24):2288–2301. https://doi.org/10.1056/NEJMoa1716948
Antonia SJ, Villegas A, Daniel D, Vicente D, Murakami S, Hui R, Yokoi T, Chiappori A, Lee KH, de Wit M, Cho BC, Bourhaba M, Quantin X, Tokito T, Mekhail T, Planchard D, Kim Y-C, Karapetis CS, Hiret S, Ostoros G, Kubota K, Gray JE, Paz-Ares L, de Castro Carpeño J, Wadsworth C, Melillo G, Jiang H, Huang Y, Dennis PA, Özgüroğlu M (2017) Durvalumab after chemoradiotherapy in stage III non-small-cell lung cancer. N Engl J Med 377(20):1919–1929. https://doi.org/10.1056/NEJMoa1709937
Lee JY, Chong S, Choi YH, Phi JH, Cheon JE, Kim SK, Park SH, Kim IO, Wang KC (2017) Modification of surgical procedure for “probable” limited dorsal myeloschisis. J Neurosurg Pediatr 19(5):616–619. https://doi.org/10.3171/2016.12.PEDS16171
Rizvi NA, Mazieres J, Planchard D, Stinchcombe TE, Dy GK, Antonia SJ, Horn L, Lena H, Minenza E, Mennecier B, Otterson GA, Campos LT, Gandara DR, Levy BP, Nair SG, Zalcman G, Wolf J, Souquet PJ, Baldini E, Cappuzzo F, Chouaid C, Dowlati A, Sanborn R, Lopez-Chavez A, Grohe C, Huber RM, Harbison CT, Baudelet C, Lestini BJ, Ramalingam SS (2015) Activity and safety of nivolumab, an anti-PD-1 immune checkpoint inhibitor, for patients with advanced, refractory squamous non-small-cell lung cancer (CheckMate 063): a phase 2, single-arm trial. Lancet Oncol 16(3):257–265. https://doi.org/10.1016/s1470-2045(15)70054-9
Dunn GP, Bruce AT, Ikeda H, Old LJ, Schreiber RD (2002) Cancer immunoediting: from immunosurveillance to tumor escape. Nat Immunol 3(11):991–998. https://doi.org/10.1038/ni1102-991
Rabinovich GA, Gabrilovich D, Sotomayor EM (2007) Immunosuppressive strategies that are mediated by tumor cells. Annu Rev Immunol 25:267–296. https://doi.org/10.1146/annurev.immunol.25.022106.141609
Huang A, Zhang B, Wang B, Zhang F, Fan KX, Guo YJ (2013) Increased CD14(+)HLA-DR (–/low) myeloid-derived suppressor cells correlate with extrathoracic metastasis and poor response to chemotherapy in non-small cell lung cancer patients. Cancer Immunol Immunother 62(9):1439–1451. https://doi.org/10.1007/s00262-013-1450-6
Vetsika E-K, Koinis F, Gioulbasani M, Aggouraki D, Koutoulaki A, Skalidaki E, Mavroudis D, Georgoulias V, Kotsakis A (2014) A circulating subpopulation of monocytic myeloid-derived suppressor cells as an independent prognostic/predictive factor in untreated non-small lung cancer patients. J Immunol Res 2014:12. https://doi.org/10.1155/2014/659294
Bloch O, Crane CA, Kaur R, Safaee M, Rutkowski MJ, Parsa AT (2013) Gliomas promote immunosuppression through induction of B7-H1 expression in tumor-associated macrophages. Clin Cancer Res 19(12):3165–3175. https://doi.org/10.1158/1078-0432.CCR-12-3314
Bloch O, Lim M, Sughrue ME, Komotar RJ, Abrahams JM, O’Rourke DM, D’Ambrosio A, Bruce JN, Parsa AT (2017) Autologous heat shock protein peptide vaccination for newly diagnosed glioblastoma: impact of peripheral PD-L1 expression on response to therapy. Clin Cancer Res 23(14):3575–3584. https://doi.org/10.1158/1078-0432.Ccr-16-1369
Kotsakis A, Koinis F, Katsarou A, Gioulbasani M, Aggouraki D, Kentepozidis N, Georgoulias V, Vetsika EK (2016) Prognostic value of circulating regulatory T cell subsets in untreated non-small cell lung cancer patients. Sci Rep 6:39247. https://doi.org/10.1038/srep39247
Lamano J, Lamano J, Choy W, Veliceasa D, DiDomenico J, Oyon D, Quaggin-Smith J, Fakurnejad S, Ampie L, Li D, Kesavabhotla K, Kaur R, James CD, Parsa A, Bloch O (2017) IMMU-38. glioblastoma-derived IL-6 induces immunosuppressive peripheral myeloid cell PD-L1 expression and tumor progression. Neuro-Oncol 19(suppl_6):vi120–vi121. https://doi.org/10.1093/neuonc/nox168.496
Gao J, Aksoy BA, Dogrusoz U, Dresdner G, Gross B, Sumer SO, Sun Y, Jacobsen A, Sinha R, Larsson E, Cerami E, Sander C, Schultz N (2013) Integrative analysis of complex cancer genomics and clinical profiles using the cBioPortal. Sci Signal 6(269):pl1. https://doi.org/10.1126/scisignal.2004088
Cerami E, Gao J, Dogrusoz U, Gross BE, Sumer SO, Aksoy BA, Jacobsen A, Byrne CJ, Heuer ML, Larsson E, Antipin Y, Reva B, Goldberg AP, Sander C, Schultz N (2012) The cBio cancer genomics portal: an open platform for exploring multidimensional cancer genomics data. Cancer Discov 2(5):401–404. https://doi.org/10.1158/2159-8290.Cd-12-0095
Almand B, Resser JR, Lindman B, Nadaf S, Clark JI, Kwon ED, Carbone DP, Gabrilovich DI (2000) Clinical significance of defective dendritic cell differentiation in cancer. Clin Cancer Res 6(5):1755–1766
Gajewski TF, Meng Y, Harlin H (2006) Immune suppression in the tumor microenvironment. J Immunother 29(3):233–240. https://doi.org/10.1097/01.cji.0000199193.29048.56
Remark R, Becker C, Gomez JE, Damotte D, Dieu-Nosjean M-C, Sautès-Fridman C, Fridman W-H, Powell CA, Altorki NK, Merad M, Gnjatic S (2015) The non-small cell lung cancer immune contexture. A major determinant of tumor characteristics and patient outcome. Am J Respir Crit Care Med 191(4):377–390. https://doi.org/10.1164/rccm.201409-1671pp
Chae M, Peterson TE, Balgeman A, Chen S, Zhang L, Renner DN, Johnson AJ, Parney IF (2015) Increasing glioma-associated monocytes leads to increased intratumoral and systemic myeloid-derived suppressor cells in a murine model. Neuro Oncol 17(7):978–991. https://doi.org/10.1093/neuonc/nou343
Gustafson MP, Lin Y, New KC, Bulur PA, O’Neill BP, Gastineau DA, Dietz AB (2010) Systemic immune suppression in glioblastoma: the interplay between CD14(+)HLA-DR(lo/neg) monocytes, tumor factors, and dexamethasone. Neuro-Oncol 12(7):631–644. https://doi.org/10.1093/neuonc/noq001
Vuk-Pavlovic S, Bulur PA, Lin Y, Qin R, Szumlanski CL, Zhao X, Dietz AB (2010) Immunosuppressive CD14+ HLA-DRlow/- monocytes in prostate cancer. Prostate 70(4):443–455. https://doi.org/10.1002/pros.21078
Liyanage UK, Moore TT, Joo HG, Tanaka Y, Herrmann V, Doherty G, Drebin JA, Strasberg SM, Eberlein TJ, Goedegebuure PS, Linehan DC (2002) Prevalence of regulatory T cells is increased in peripheral blood and tumor microenvironment of patients with pancreas or breast adenocarcinoma. J Immunol 169(5):2756–2761
Yu H, Boyle TA, Zhou C, Rimm DL, Hirsch FR (2016) PD-L1 expression in lung cancer. J Thorac Oncol 11(7):964–975
Dong H, Strome SE, Salomao DR, Tamura H, Hirano F, Flies DB, Roche PC, Lu J, Zhu G, Tamada K, Lennon VA, Celis E, Chen L (2002) Tumor-associated B7-H1 promotes T-cell apoptosis: a potential mechanism of immune evasion. Nat Med 8(8):793–800. https://doi.org/10.1038/nm730
Mauer J, Chaurasia B, Goldau J, Vogt MC, Ruud J, Nguyen KD, Theurich S, Hausen AC, Schmitz J, Bronneke HS, Estevez E, Allen TL, Mesaros A, Partridge L, Febbraio MA, Chawla A, Wunderlich FT, Bruning JC (2014) Signaling by IL-6 promotes alternative activation of macrophages to limit endotoxemia and obesity-associated resistance to insulin. Nat Immunol 15(5):423–430. https://doi.org/10.1038/ni.2865
Haura EB, Livingston S, Coppola D (2006) Autocrine interleukin-6/interleukin-6 receptor stimulation in non-small-cell lung cancer. Clin Lung Cancer 7(4):273–275
Caetano MS, Zhang H, Cumpian AM, Gong L, Unver N, Ostrin EJ, Daliri S, Chang SH, Ochoa CE, Hanash S, Behrens C, Wistuba II, Sternberg C, Kadara H, Ferreira CG, Watowich SS, Moghaddam SJ (2016) IL6 blockade reprograms the lung tumor microenvironment to limit the development and progression of K-ras-mutant lung cancer. Cancer Res 76(11):3189–3199. https://doi.org/10.1158/0008-5472.Can-15-2840
Song L, Smith MA, Doshi P, Sasser K, Fulp W, Altiok S, Haura EB (2014) Antitumor efficacy of the anti-interleukin-6 (IL-6) antibody siltuximab in mouse xenograft models of lung cancer. J Thorac Oncol 9(7):974–982. https://doi.org/10.1097/JTO.0000000000000193
Bichsel CA, Wang L, Froment L, Berezowska S, Müller S, Dorn P, Marti TM, Peng R-W, Geiser T, Schmid RA, Guenat OT, Hall SRR (2017) Increased PD-L1 expression and IL-6 secretion characterize human lung tumor-derived perivascular-like cells that promote vascular leakage in a perfusable microvasculature model. Sci Rep 7(1):10636. https://doi.org/10.1038/s41598-017-09928-1
Jayatilaka H, Tyle P, Chen JJ, Kwak M, Ju J, Kim HJ, Lee JSH, Wu P-H, Gilkes DM, Fan R, Wirtz D (2017) Synergistic IL-6 and IL-8 paracrine signalling pathway infers a strategy to inhibit tumour cell migration. Nat Commun 8:15584. https://doi.org/10.1038/ncomms15584
Shen MJ, Xu LJ, Yang L, Tsai Y, Keng PC, Chen Y, Lee SO, Chen Y (2017) Radiation alters PD-L1/NKG2D ligand levels in lung cancer cells and leads to immune escape from NK cell cytotoxicity via IL-6-MEK/Erk signaling pathway. Oncotarget 8(46):80506–80520. https://doi.org/10.18632/oncotarget.19193
Kim M-Y, Oskarsson T, Acharyya S, Nguyen DX, Zhang XHF, Norton L, Massagué J (2009) Tumor self-seeding by circulating cancer cells. Cell 139(7):1315–1326. https://doi.org/10.1016/j.cell.2009.11.025
De Vita F, Orditura M, Auriemma A, Infusino S, Roscigno A, Catalano G (1998) Serum levels of interleukin-6 as a prognostic factor in advanced non-small cell lung cancer. Oncol Rep 5(3):649–652
Hao CC, Fu HC, Min YY, Chen CG, Huang TY, Min CY, Shyan HM, Ling CH, Jen LY, Chyr YP, Jen CC, Hsiung CA, Chou SW (2013) Circulating interleukin-6 level is a prognostic marker for survival in advanced nonsmall cell lung cancer patients treated with chemotherapy. Int J Cancer 132(9):1977–1985. https://doi.org/10.1002/ijc.27892
Silva EM, Mariano VS, Pastrez PRA, Pinto MC, Castro AG, Syrjanen KJ, Longatto-Filho A (2017) High systemic IL-6 is associated with worse prognosis in patients with non-small cell lung cancer. PLoS One 12(7):e0181125. https://doi.org/10.1371/journal.pone.0181125
Acknowledgements
The authors would like to thank the Nervous System Tumor Bank at Northwestern University, without which the current study would not be possible. Imaging work was performed at the Northwestern University Center for Advanced Microscopy generously supported by NCI CCSG P30 CA060553 awarded to the Robert H Lurie Comprehensive Cancer Center.
Funding
This work was supported by the Howard Hughes Medical Institute Medical Student Research Fellows program (Yuping D. Li) as well as by the NIH/National Cancer Institute (NCI) Ruth L. Kirschtein National Research Service Award F30 (CA206413; Jonathan B Lamano), NIH/NCI R01 (CA164714; Orin Bloch), and NIH/National Institute of Neurological Disorders and Stroke (NINDS) R00 (NS078055; Orin Bloch).
Author information
Authors and Affiliations
Contributions
YDL took part in conceptualization, experimental design, data curation, formal analysis, funding acquisition, methodology, validation, and writing the manuscript. JBL took part in conceptualization, experimental design, data curation and formal analysis. JBL took part in data curation, formal analysis, methodology, and validation. JQ-S and DV took part in experimental design and data curation. GK, and DB took part in data curation. DU took part in formal analysis. OB took part in conceptualization, funding acquisition, investigation, methodology, and supervision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval and ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the Institutional Review Board of Northwestern University, Feinberg School of Medicine (STU00204920).
Informed consent
Written informed consent was obtained from all individual participants included in the study for the use of their blood and tumor specimen for research. Consent was not required for collection of patient characteristics as information was de-identified. Consent was not required for TCGA data collection as the TCGA is a de-identified, public database.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This work was previously published as an abstract at the 2018 American Association of Neurological Surgeons (AANS) Annual Scientific Meeting in New Orleans, LA, USA on April 29-May 2, 2018 [1].
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Li, Y.D., Lamano, J.B., Lamano, J.B. et al. Tumor-induced peripheral immunosuppression promotes brain metastasis in patients with non-small cell lung cancer. Cancer Immunol Immunother 68, 1501–1513 (2019). https://doi.org/10.1007/s00262-019-02384-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00262-019-02384-y