Abstract
Purpose
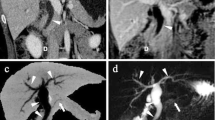
To determine sensitivity and specificity of the “duct-interrupted,” “corona,” and “attraction” signs on MR cholangio-pancreatography (MRCP) in distinguishing pancreatic head ductal adenocarcinoma (PDAC) from inflammatory pancreatic pseudomass (IPP).
Materials and methods
This study included 53 adults (33 men and 20 women, mean age, 55 years; range, 17–87 years) with a pancreatic head mass who underwent MRCP. Three blinded radiologists independently reviewed each MRCP exam and three signs were assessed: (1) the “duct-interrupted” sign, deemed positive for PDAC if the duct within the mass demonstrated complete interruption with upstream dilation; (2) the “corona” sign, considered positive for PDAC if dilated side-branches were located exclusively outside the mass; and (3) the “attraction” sign, deemed positive for IPP if the dilated common bile duct showed attraction and angulation towards the mass. Sensitivity, specificity, and positive and negative predictive values of the signs were calculated, as well as interobserver agreement.
Results
Out of 53 masses, 17 (32%) were PDAC and 36 (68%) were IPP. Sensitivity, specificity, and positive and negative predictive values of the “duct-interrupted” sign to differentiate between PDAC from IPP for the three readers were 29–53%, 89–95%, 56–82% and 73–81%, respectively (κ = 0.41); for the “corona” sign, they were 29–53%, 81–100%, 56–100%, and 75–78%, respectively (κ = 0.4), and for the “attraction” sign, they were 20–25%, 71–82%, 64–75%, and 31–34%, respectively (κ = 0.54).
Conclusion
The “duct-interrupted” and “corona” MRCP signs have high specificity for diagnosing PDAC, while the “attraction” sign has good specificity for identifying IPP.








Similar content being viewed by others
References
Lee ES, Lee JM. Imaging diagnosis of pancreatic cancer: A state-of-the-art review WJG 20 th Anniversary Special Issues (14): Pancreatic cancer. World J Gastroenterol [Internet]. 2014 [cited 2018 Jan 23];20(24):7864–77. Available from: http://www.wjgnet.com/1007-9327/full/
Ichikawa T, Sou H, Araki T, et al. (2001) Duct-penetrating sign at MRCP: usefulness for differentiating inflammatory pancreatic mass from pancreatic carcinomas. Radiology 221(1):107–116
Neff CC, Simeone JF, Wittenberg J, Mueller PR, Joseph Ferrucci IT. Inflammatory Pancreatic Masses Problems in Differentiating Focal Pancreatitis from Carcinoma’. [cited 2018 Jan 10]; Available from: http://pubs.rsna.org.ezp-prod1.hul.harvard.edu/doi/pdf/10.1148/radiology.150.1.6689784
Schima W, Függer R (2002) Evaluation of focal pancreatic masses: comparison of mangafodipir-enhanced MR imaging and contrast-enhanced helical CT. Eur Radiol. 12:2998–3008
Lammer J, Herlinger H, Zalaudek G, Hofler H. Pseudotumorous Pancreatitis. Gastrointest Radiol [Internet]. 1985 [cited 2018 Jan 10];10:59–67. Available from: https://link-springer-com.ezp-prod1.hul.harvard.edu/content/pdf/10.1007%2FBF01893072.pdf
Abraham Susan, Wilentz Robb, Yeo Charles, Sohn Taylos, Cameron John, Boitnott John HR. Pancreaticoduodenectomy (Whipple Resections) in Patients Without Malignancy Are They All “Chronic Pancreatitis”? [Internet]. American Journal of Surgical Patholology. 2003 [cited 2018 Jan 10]. p. 110–20. Available from: http://ovidsp.tx.ovid.com.ezp-prod1.hul.harvard.edu/sp-3.27.2b/ovidweb.cgi?WebLinkFrameset=1&S=CGNNFPOMHKDDJKLONCFKKBMCABIBAA00&returnUrl=ovidweb.cgi%3F%26Full%2BText%3DL%257cS.sh.22.23%257c0%257c00000478-200301000-00012%26S%3DCGNNFPOMHKDDJKLONCFKKBMCABIB
Kennedy T, Preczewski L, Stocker SJ, Rao SM, Parsons WG, Wayne JD, et al. Incidence of benign inflammatory disease in patients undergoing Whipple procedure for clinically suspected carcinoma: a single-institution experience. [cited 2018 Jan 10]; Available from: https://ac-els-cdn-com.ezp-prod1.hul.harvard.edu/S0002961005009335/1-s2.0-S0002961005009335-main.pdf?_tid=bc50e71a-f61b-11e7-ae4c-00000aacb35d&acdnat=1515598644_1aa840aaa0af7babbcee5f97f76f5cc7
Schima W (2006) MRI of the pancreas: tumours and tumour-simulating processes. Cancer Imaging. 6:199–203
Choi S-Y, Kim SH, Kang TW, Song KD, Park HJ, Choi Y-H. Differentiating Mass-Forming Autoimmune Pancreatitis From Pancreatic Ductal Adenocarcinoma on the Basis of Contrast-Enhanced MRI and DWI Findings. Am J Roentgenol [Internet]. 2016 Feb [cited 2016 Aug 3];206(2):291–300. Available from: http://www.ajronline.org/doi/10.2214/AJR.15.14974
Chen FM, Ni JM, Zhang ZY, Zhang L, Li B, Jiang CJ. Presurgical evaluation of pancreatic cancer: A comprehensive imaging comparison of CT versus MRI. Am J Roentgenol. 2016;
Griffin N, Charles-Edwards G, Grant LA (2012) Magnetic resonance cholangiopancreatography: The ABC of MRCP. Insights into Imaging 3:11–21
Kim HJ, Kim YK, Jeong WK, Lee WJ, Choi D (2015) Pancreatic duct “Icicle sign” on MRI for distinguishing autoimmune pancreatitis from pancreatic ductal adenocarcinoma in the proximal pancreas. Eur Radiol. 25(6):1551–1560
Massey LA, Jäger HR, Paviour DC, O ’sullivan SS, Ling H, Williams DR, et al. The midbrain to pons ratio. [cited 2018 Jun 8]; Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3908351/pdf/WNL205033.pdf
Corwin MT, Gerscovich EO, Lamba R, Wilson M, McGahan JP. Differentiation of Ovarian Endometriomas from Hemorrhagic Cysts at MR Imaging: Utility of the T2 Dark Spot Sign. Radiology [Internet]. 2014;271(1):126–32. Available from: http://pubs.rsna.org/doi/10.1148/radiol.13131394
Genders TSS, Spronk S, Stijnen T, Steyerberg EW, Lesaffre E, Hunink MGM. Methods for calculating sensitivity and specificity of clustered Data: A Tutorial 1. Radiol n Radiol [Internet]. 2012 [cited 2018 Jun 8];265. Available from: http://radiology.rsna.org/lookup
Negrelli R, Manfredi R, Pedrinolla B, Boninsegna E, Ventriglia A, Mehrabi S, et al. Pancreatic duct abnormalities in focal autoimmune pancreatitis: MR/MRCP imaging findings. Eur Radiol [Internet]. 2015 [cited 2016 Aug 3];25(2):359–67. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25106489
Kim M, Mi Jang K, Kim J-H, Kyoung Jeong W, Hyun Kim S, Wook Kang T, et al. Differentiation of mass-forming focal pancreatitis from pancreatic ductal adenocarcinoma: value of characterizing dynamic enhancement patterns on contrast-enhanced MR images by adding signal intensity color mapping. Eur Radiol. 2017;27:1722–1732
Patnana M, Sevrukov AB, Elsayes KM, Viswanathan C, Lubner M, Menias CO. Inflammatory pseudotumor: The great mimicker. Am J Roentgenol. 2012;198(3):W217–W227
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Beker, K., Lee, K.S., Tsai, L.L. et al. Differentiation of pancreatic head ductal adenocarcinoma from inflammatory pancreatic pseudomass by MR cholangio-pancreatography: utility of the duct-interrupted, corona, and attraction signs. Abdom Radiol 44, 4048–4056 (2019). https://doi.org/10.1007/s00261-019-02155-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-019-02155-4