Abstract
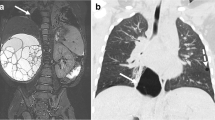
Fetal lung lesions include common lesions such as congenital pulmonary airway malformation (CPAM), bronchopulmonary sequestration (BPS) and combined CPAM–BPS hybrid lesions, as well as less common entities including congenital lobar emphysema/obstruction, bronchial atresia, bronchogenic cysts and rare malignant pulmonary lesions such as pleuropulmonary blastoma. Fetal lung lesions occur in approximately 1 in 15,000 live births and are thought to arise from a spectrum of abnormalities related to airway obstruction and malformation, with the lesion type depending on the timing of insult, level of bronchial tree involvement, and severity of obstruction. Lesions vary from small and asymptomatic to large and symptomatic with significant mass effect on surrounding structures. Accurate diagnosis and characterization of these anomalies is crucial for guiding patient counseling as well as perinatal and postnatal management. The goal of this review is to provide an overview of normal fetal lung appearance and imaging features of common and uncommon lesions on both ultrasound and MR imaging, and to discuss key aspects in reporting and evaluating the severity of these lesions.




















Similar content being viewed by others
References
Epelman M, Kreiger PA, Servaes S et al (2010) Current imaging of prenatally diagnosed congenital lung lesions. Semin Ultrasound CT MR 31:141–157
Cass DL, Olutoye OO, Cassady CI et al (2011) Prenatal diagnosis and outcome of fetal lung masses. J Pediatr Surg 46:292–298
Kunisaki SM, Fauza DO, Nemes LP et al (2006) Bronchial atresia: the hidden pathology within a spectrum of prenatally diagnosed lung masses. J Pediatr Surg 41:61–65
Peranteau WH, Boelig MM, Khalek N et al (2016) Effect of single and multiple courses of maternal betamethasone on prenatal congenital lung lesion growth and fetal survival. J Pediatr Surg 51:28–32
Adzick NS (2009) Management of fetal lung lesions. Clin Perinatol 36:363–376
Bulas D, Egloff AM (2011) Fetal chest ultrasound and magnetic resonance imaging: recent advances and current clinical applications. Radiol Clin N Am 49:805–823
Kasprian G, Balassy C, Brugger PC, Prayer D (2006) MRI of normal and pathological fetal lung development. Eur J Radiol 57:261–270
Crombleholme TM, Coleman B, Hedrick H et al (2002) Cystic adenomatoid malformation volume ratio predicts outcome in prenatally diagnosed cystic adenomatoid malformation of the lung. J Pediatr Surg 37:331–338
Victoria T, Johnson AM, Edgar JC et al (2016) Comparison between 1.5-T and 3-T MRI for fetal imaging: is there an advantage to imaging with a higher field strength? AJR Am J Roentgenol 206:195–201
Victoria T, Bebbington MW, Danzer E et al (2012) Use of magnetic resonance imaging in prenatal prognosis of the fetus with isolated left congenital diaphragmatic hernia. Prenat Diagn 32:715–723
Danzer E, Victoria T, Bebbington MW et al (2012) Fetal MRI-calculated total lung volumes in the prediction of short-term outcome in giant omphalocele: preliminary findings. Fetal Diagn Ther 31:248–253
Meyers ML, Garcia JR, Blough KL et al (2018) Fetal lung volumes by MRI: normal weekly values from 18 through 38 weeks' gestation. AJR Am J Roentgenol 211:432–438
Rypens F, Metens T, Rocourt N et al (2001) Fetal lung volume: estimation at MR imaging-initial results. Radiology 219:236–241
Yamoto M, Iwazaki T, Takeuchi K et al (2018) The fetal lung-to-liver signal intensity ratio on magnetic resonance imaging as a predictor of outcomes from isolated congenital diaphragmatic hernia. Pediatr Surg Int 34:161–168
Cannie M, Jani J, De Keyzer F et al (2009) Diffusion-weighted MRI in lungs of normal fetuses and those with congenital diaphragmatic hernia. Ultrasound Obstet Gynecol 34:678–686
Werner H, Dos Santos JR, Fontes R et al (2011) Virtual bronchoscopy in the fetus. Ultrasound Obstet Gynecol 37:113–115
Werner H, Lopes dos Santos JR, Fontes R et al (2013) Virtual bronchoscopy for evaluating cervical tumors of the fetus. Ultrasound Obstet Gynecol 41:90–94
Langston C (2003) New concepts in the pathology of congenital lung malformations. Semin Pediatr Surg 12:17–37
Barth RA (2012) Imaging of fetal chest masses. Pediatr Radiol 42:S62–S73
Stocker JT, Madewell JE, Drake RM (1977) Congenital pulmonary airway malformation — a new name for and an expanded classification of congenital cystic adenomatoid malformation of the lung. Classification and morphologic spectrum. Hum Pathol 8:155–171
Stocker JT, Dehner LP, Inc OT (2002) Pediatric pathology. Lippincott Williams & Wilkins, Philadelphia
Daltro P, Werner H, Gasparetto TD et al (2010) Congenital chest malformations: a multimodality approach with emphasis on fetal MR imaging. Radiographics 30:385–395
Stocker JT (2009) Cystic lung disease in infants and children. Fetal Pediatr Pathol 28:155–184
Annunziata F, Bush A, Borgia F et al (2019) Congenital lung malformations: unresolved issues and unanswered questions. Front Pediatr 7:239
Adzick NS, Harrison MR, Crombleholme TM et al (1998) Fetal lung lesions: management and outcome. Am J Obstet Gynecol 179:884–889
Victoria T, Srinivasan AS, Pogoriler J et al (2018) The rare solid fetal lung lesion with T2-hypointense components: prenatal imaging findings with postnatal pathological correlation. Pediatr Radiol 48:1556–1566
Oliver ER, DeBari SE, Giannone MM et al (2018) Going with the flow: an aid in detecting and differentiating bronchopulmonary sequestrations and hybrid lesions. J Ultrasound Med 37:371–383
Johnson AM, Hubbard AM (2004) Congenital anomalies of the fetal/neonatal chest. Semin Roentgenol 39:197–214
Riley JS, Urwin JW, Oliver ER et al (2018) Prenatal growth characteristics and pre/postnatal management of bronchopulmonary sequestrations. J Pediatr Surg 53:265–269
Newman B (2006) Congenital bronchopulmonary foregut malformations: concepts and controversies. Pediatr Radiol 36:773–791
Cass DL, Crombleholme TM, Howell LJ et al (1997) Cystic lung lesions with systemic arterial blood supply: a hybrid of congenital cystic adenomatoid malformation and bronchopulmonary sequestration. J Pediatr Surg 32:986–990
Mani H, Suarez E, Stocker JT (2004) The morphologic spectrum of infantile lobar emphysema: a study of 33 cases. Paediatr Respir Rev 5:S313–S320
Seo T, Ando H, Kaneko K et al (2006) Two cases of prenatally diagnosed congenital lobar emphysema caused by lobar bronchial atresia. J Pediatr Surg 41:e17–e20
Oliver ER, DeBari SE, Horii SC et al (2019) Congenital lobar overinflation: a rare enigmatic lung lesion on prenatal ultrasound and magnetic resonance imaging. J Ultrasound Med 38:1229–1239
Alamo L, Reinberg O, Vial Y et al (2013) Comparison of foetal US and MRI in the characterisation of congenital lung anomalies. Eur J Radiol 82:e860–e866
Peranteau WH, Merchant AM, Hedrick HL et al (2008) Prenatal course and postnatal management of peripheral bronchial atresia: association with congenital cystic adenomatoid malformation of the lung. Fetal Diagn Ther 24:190–196
Parikh D, Samuel M (2005) Congenital cystic lung lesions: is surgical resection essential? Pediatr Pulmonol 40:533–537
Reiss A, Goldberg Y, Monichor M, Drugan A (2005) Congenital pulmonary myofibroblastic tumor — pathology and prenatal sonographic appearance. Prenat Diagn 25:1064–1066
Calvo-Garcia MA, Lim FY, Stanek J et al (2014) Congenital peribronchial myofibroblastic tumor: prenatal imaging clues to differentiate from other fetal chest lesions. Pediatr Radiol 44:479–483
Waelti SL, Garel L, Soglio DD et al (2017) Neonatal congenital lung tumors — the importance of mid-second-trimester ultrasound as a diagnostic clue. Pediatr Radiol 47:1766–1775
Zhang H, Xu CW, Wei JG et al (2015) Infant pleuropulmonary blastoma: report of a rare case and review of literature. Int J Clin Exp Pathol 8:13571–13577
Coleman A, Kline-Fath B, Stanek J, Lim FY (2016) Pleuropulmonary blastoma in a neonate diagnosed prenatally as congenital pulmonary airway malformation. Fetal Diagn Ther 39:234–237
Miniati DN, Chintagumpala M, Langston C et al (2006) Prenatal presentation and outcome of children with pleuropulmonary blastoma. J Pediatr Surg 41:66–71
Dishop MK, McKay EM, Kreiger PA et al (2010) Fetal lung interstitial tumor (FLIT): a proposed newly recognized lung tumor of infancy to be differentiated from cystic pleuropulmonary blastoma and other developmental pulmonary lesions. Am J Surg Pathol 34:1762–1772
Phillips J, Blask A, DiPoto BA et al (2019) Fetal lung interstitial tumor: prenatal presentation of a rare fetal malignancy. J Neonatal Perinatal Med 12:473–477
Colleran GC, Ryan CE, Lee EY et al (2017) Computed tomography and upper gastrointestinal series findings of esophageal bronchi in infants. Pediatr Radiol 47:154–160
Partridge EA, Victoria T, Coleman BG et al (2015) Prenatal diagnosis of esophageal bronchus — first report of a rare foregut malformation in utero. J Pediatr Surg 50:306–310
Mong A, Johnson AM, Kramer SS et al (2008) Congenital high airway obstruction syndrome: MR/US findings, effect on management, and outcome. Pediatr Radiol 38:1171–1179
Farnaghi S, Kothari A (2013) The value of early recognition of fetal lymphangioma. Australas J Ultrasound Med 16:147–152
Goldstein I, Leibovitz Z, Noi-Nizri M (2006) Prenatal diagnosis of fetal chest lymphangioma. J Ultrasound Med 25:1437–1440
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Adams, N.C., Victoria, T., Oliver, E.R. et al. Fetal ultrasound and magnetic resonance imaging: a primer on how to interpret prenatal lung lesions. Pediatr Radiol 50, 1839–1854 (2020). https://doi.org/10.1007/s00247-020-04806-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-020-04806-x