Abstract
Purpose
We investigated the developmental changes in the unaffected contralateral lungs of patients with isolated left-sided congenital diaphragmatic hernia (CDH) using signal intensity ratios on prenatal magnetic resonance imaging (MRI) and determined whether these changes correlated with clinical outcomes.
Methods
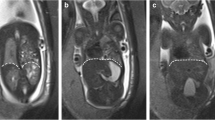
We performed 47 fetal MRI screens on 30 patients with isolated left-sided CDH. A cohort of 88 fetuses was selected as the control. We calculated the lung-to-liver signal intensity ratio (LLSIR) using region of interest analysis and compared LLSIR between the groups and between those in the CDH group with good and poor prognoses.
Results
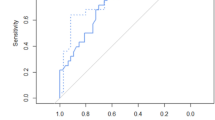
In the control group, LLSIR increased as pregnancy progressed [regression line = 2.232 + 0.135 × (GW—23), r = 0.669]. In the CDH group, especially in the poor prognosis group, LLSIR did not significantly increase as pregnancy progressed [regression line for good prognosis = 1.827 + 0.092 × (gestational week—23), r = 0.733; regression line for poor prognosis = 1.731 + 0.025 × (gestational week—23), r = 0.634].
Conclusion
Fetal LLSIR on T2-weighted MRI is an accurate marker of fetal lung maturity that correlates with postnatal survival and can potentially be used as a prognostic parameter in CDH management.






Similar content being viewed by others
References
Cannie M, Jani J, Chaffiotte C et al (2008) Quantification of intrathoracic liver herniation by magnetic resonance imaging and prediction of postnatal survival in fetuses with congenital diaphragmatic hernia. Ultrasound Obstet Gynecol 32:627–632
Kitano Y, Okuyama H, Saito M et al (2011) Re-evaluation of stomach position as a simple prognostic factor in fetal left congenital diaphragmatic hernia: a multicenter survey in Japan. Ultrasound Obstet Gynecol 37:277–282
Lipshutz GS, Albanese CT, Feldstein VA et al (1997) Prospective analysis of lung-to-head ratio predicts survival for patients with prenatally diagnosed congenital diaphragmatic hernia. J Pediatr Surg 32:1634–1636
Jani J, Nicolaides KH, Keller RL, Antenatal-CDH-Registry Group et al (2007) Observed to expected lung area to head circumference ratio in the prediction of survival in fetuses with isolated diaphragmatic hernia. Ultrasound Obstet Gynecol 30:67–71
Worley KC, Dashe JS, Barber RG et al (2009) Fetal magnetic resonance imaging in isolated diaphragmatic hernia: volume of herniated liver and neonatal outcome. Am J Obstet Gynecol 200:1–6
Cannie M, Jani J, de Keyzer F et al (2009) Diffusion-weighted MRI in lungs of normal fetuses and those with congenital diaphragmatic hernia. Ultrasound Obstet Gynecol 34:678 – 86
Kuwashima S, Nishimura G, Iimura F et al (2001) Low-intensity fetal lungs on MRI may suggest the diagnosis of pulmonary hypoplasia. Pediatr Radiol 31:669–672
Deprest J, Brady P, Nicolaides K et al (2014) Prenatal management of the fetus with isolated congenital diaphragmatic hernia in the era of the TOTAL trial. Semin Fetal Neonatal Med 19:338–348
Jani J, Peralta CF, Van Schoubroeck D et al (2006) Relationship between lung-to-head ratio and lung volume in normal fetuses and fetuses with diaphragmatic hernia. Ultrasound Obstet Gynecol 27:545–550
Rypens F, Metens T, Rocourt N et al (2001) Fetal lung volume: estimation at MR imaging-initial results. Radiology 219:236–241
Graham G, Devine PC (2005) Antenatal diagnosis of congenital diaphragmatic hernia. Semin Perinatol 29:69–76
Nakamura Y, Yamamoto I, Fukuda S et al (1991) Pulmonary acinar development in diaphragmatic hernia. Arch Pathol Lab Med 115:372–376
Kitagawa M, Hislop A, Boyden EA et al (1971) Lung hypoplasia in congenital diaphragmatic hernia. A quantitative study of airway, artery, and alveolar development. Br J Surg 58:342–346
Ting A, Glick PL, Wilcox DT et al (1998) Alveolar vascularization of the lung in a lamb model of congenital diaphragmatic hernia. Am J Respir Crit Care Med 157:31–34
Balassy C, Kasprian G, Brugger PC et al (2007) MRI investigation of normal fetal lung maturation using signal intensities on different imaging sequences. Eur Radiol 17:835–842
Keller TM, Rake A, Michel SC et al (2004) MR assessment of fetal lung development using lung volumes and signal intensities. Eur Radiol 14:984–989
Moshiri M, Mannelli L, Richardson ML et al (2013) Fetal lung maturity assessment with MRI fetal lung-to-liver signal-intensity ratio. AJR Am J Roentgenol 201:1386–1390
Di Fiore JW, Wilson JM (1994) Lung development. Semin Pediatr Surg 3:221–232
Kizilcan F, Tanyel FC, Cakar N et al (1995) The effect of low amniotic pressure without oligohydramnios on fetal lung development in a rabbit model. Am J Obstet Gynecol 173:36–41
Wigglesworth JS, Desai R, Guerrini P (1981) Fetal lung hypoplasia: biochemical and structural variations and their possible significance. Arch Dis Child 56:606–615
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Research involving human participants and/or animals
We received approval from the institutional ethics committee of Shizuoka Children’s Hospital for this study (Approval Number of 2017018).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Yamoto, M., Iwazaki, T., Takeuchi, K. et al. The fetal lung-to-liver signal intensity ratio on magnetic resonance imaging as a predictor of outcomes from isolated congenital diaphragmatic hernia. Pediatr Surg Int 34, 161–168 (2018). https://doi.org/10.1007/s00383-017-4184-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-017-4184-2