Abstract
Background
Adverse outcomes for infants born with left congenital diaphragmatic hernia (CDH) have been correlated with fetal imaging findings.
Objective
We sought to corroborate these correlations in a high-risk cohort and describe a predictive mortality algorithm combining multiple imaging biomarkers for use in prenatal counseling.
Materials and methods
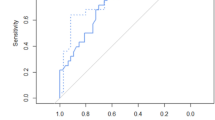
We reviewed fetal MRI examinations at our institution from 2004 to 2016 demonstrating left-side CDH. MRI findings, hospital course and outcomes were recorded and analyzed using bivariate and multivariable analysis. We generated a receiver operating curve (ROC) to determine a cut-off relation for mortality. Finally, we created a predictive mortality calculator.
Results
Of 41 fetuses included in this high-risk cohort, 41% survived. Per bivariate analysis, observed-to-expected total fetal lung volume (P=0.007), intrathoracic position of the stomach (P=0.049), and extracorporeal membrane oxygenation (ECMO) requirement (P<0.001) were significantly associated with infant mortality. Youden J statistic optimized the ROC for mortality at 24% observed-to-expected total fetal lung volume (sensitivity 64%, specificity 82%, area under the curve 0.72). On multivariable analysis, observed-to-expected total fetal lung volume ± 24% was predictive of mortality (adjusted odds ratio, 95% confidence interval: 0.09 [0.02, 0.55]; P=0.008). We derived a novel mortality prediction calculator from this analysis.
Conclusion
In this high-risk cohort, decreased observed-to-expected total fetal lung volume and stomach herniation were significantly associated with mortality. The novel predictive mortality calculator utilizes information from fetal MR imaging and provides prognostic information for health care providers. Creation of similar predictive tools by other institutions, using their distinct populations, might prove useful in family counseling, especially where there are discordant imaging findings.





Similar content being viewed by others
References
Langham M, Kays D, Ledbetter D et al (1996) Congenital diaphragmatic hernia: epidemiology and outcome. Clin Perinatol 23:671–687
Dingeldein M (2018) Congenital diaphragmatic hernia: management & outcomes. Adv Pediatr Infect Dis 65:241–247
Oliver ER, DeBari SE, Adams SE et al (2019) Congenital diaphragmatic hernia sacs: prenatal imaging and associated postnatal outcomes. Pediatr Radiol 11:1–7
Pugliandla PS, Grabowski J, Austin M et al (2015) Management of congenital diaphragmatic hernia: a systemic review from the APSA outcomes and evidence based practice committee. J Pediatr Surg 50:1958–1970
Snoek KG, Reiss IK, Greenough A et al (2016) Standardized postnatal management of infants with congenital diaphragmatic hernia in Europe: the CDH EURO consortium consensus — 2015 update. Neonatology 110:66–74
Snoek KG, Capolupo I, van Rosmalen J et al (2016) Conventional mechanical ventilation versus high-frequency oscillatory ventilation for congenital diaphragmatic hernia: a randomized clinical trial (the VICI-trial). Ann Surg 263:867–874
Abman SH, Hansmann G, Archer SL et al (2015) Pediatric pulmonary hypertension: guidelines from the American Heart Association and American Thoracic Society. Circulation 132:2037–2099
Roberts JD, Fineman JR, Morin FC et al (1997) Inhaled nitric oxide and persistent pulmonary hypertension of the newborn. The Inhaled Nitric Oxide Study Group. N Engl J Med 336:605–610
Bialkowski A, Moenkenmeyer F, Patel N (2015) Intravenous sildenafil in the management of pulmonary hypertension associated with congenital diaphragmatic hernia. Eur J Pediatr Surg 25:171–176
Lakshminrusimha S, Steinhorn RH (2013) Inodilators in nitric oxide resistant persistent pulmonary hypertension of the newborn. Pediatr Crit Care Med 14:107–109
Canadian Congenital Diaphragmatic Hernia Collaborative, Puligandla PS, Skarsgard ED et al (2018) Diagnosis and management of congenital diaphragmatic hernia: a clinical practice guideline. CMAJ 190:103–112
Bereford MS, Shaw NJ (2000) Outcome of congenital diaphragmatic hernia. Pediatr Pulmonol 30:249–256
Mah VK, Zamakshary M, Mah DY et al (2009) Absolute vs relative improvements in congenital diaphragmatic hernia survival: what happened to “hidden mortality.” J Pediatr Surg 44:877–882
Brownlee EM, Howatson AG, Davis CF, Sabharwal AJ (2009) The hidden mortality of congenital diaphragmatic hernia: a 20-year review. J Pediatr Surg 44:317–320
Peralta CFA, Cavoretto P, Csapo B et al (2005) Assessment of lung area in normal fetuses at 12–32 weeks. Ultrasound Obstet Gynecol 26:718–724
Jani J, Keller RL, Benacji A et al (2006) Prenatal prediction of survival in isolated left-sided diaphragmatic hernia. Ultrasound Obstet Gynecol 27:18–22
Jani J, Nicolaides KH, Keller RL et al (2007) Observed to expected lung area to head circumference ratio in the prediction of survival in fetuses with isolated diaphragmatic hernia. Ultrasound Obstet Gynecol 32:793–799
Jani J, Cannie M, Sonigo P et al (2008) Value of prenatal magnetic resonance imaging in the prediction of postnatal outcome in fetuses with diaphragmatic hernia. Ultrasound Obstet Gynecol 32:793–799
Albanese CT, Lopoo J, Goldstein RB et al (1998) Fetal liver position and perinatal outcome for congenital diaphragmatic hernia. Prenat Diagn 11:1138–1142
Fluke S, Kanzaki T, Mu J et al (2003) Antenatal prediction of pulmonary hypoplasia by acceleration time/ejection time ratio of fetal pulmonary arteries by Doppler blood flow velocity entry. Am J Obstet Gynecol 188:228–233
Sokol J, Shimizu N, Bohn D et al (2006) Fetal pulmonary artery diameter measurements as a predictor of morbidity in antenatally diagnosed congenital diaphragmatic hernia: a prospective study. Am J Obstet Gynecol 195:470–477
Spaggiari E, Stirnemann J, Bernard JP et al (2013) Prognostic value of a hernia sac in congenital diaphragmatic hernia. Ultrasound Obstet Gynecol 41:286–290
Zamora IJ, Cass DL, Lee TC et al (2013) The presence of a hernia sac in congenital diaphragmatic hernia is associated with better fetal lung growth and outcomes. J Pediatr Surg 48:1165–1171
Chiu LW, Desai J, Shanti C et al (2016) SNAPPE II score as a predictor of survival in neonates with congenital diaphragmatic hernia: a single center experience. Eur J Pediatr Surg 26:316–321
Lally KP (2013) Standardized reporting for congenital diaphragmatic hernia — an international consensus. J Pediatr Surg 48:2408–2415
Leon R, Li K, Brown BP (2018) A retrospective segmentation analysis of placental volume by magnetic resonance imaging from first trimester to term gestation. Pediatr Radiol 48:1936–1944
Rypens F, Metens T, Roucourt N et al (2001) Fetal lung volume: estimation at MR imaging-initial results. Radiology 219:236–241
Kitano Y (2011) Re-evaluation of stomach position as a simple prognostic factor in fetal left congenital diaphragmatic hernia: a multicenter survey in Japan. Ultrasound Obstet Gynecol 37:277–282
Youden WJ (1950) Index for rating diagnostic tests. Cancer 3:32–35
Faraggi D (2000) The effect of random measurement error on receiver operating characteristic (ROC) curves. Stat Med 19:61–70
Reiser B (2000) Measuring the effectiveness of diagnostic markers in the presence of measurement error through the use of ROC curves. Stat Med 19:2115–2129
Ruopp MD, Perkins NJ, Whitcomb BW, Schisterman EF (2008) Youden index and optimal cut-point estimated from observations affected by a lower limit of detection. Biom J 50:419–430
Victoria T, Bebbington MW, Danzer E et al (2012) Use of magnetic resonance imaging in prenatal prognosis of the fetus with isolated left congenital diaphragmatic hernia. Prenat Diagn 32:715–723
Oluyomi-Obi T, Kuret V, Puligandla P et al (2017) Antenatal predictors of outcome in prenatally diagnosed congenital diaphragmatic hernia (CDH). J Pediatr Surg 52:881–888
Hatch EI Jr, Kendall J, Blumhagen J (1992) Stomach position as an in utero predictor of neonatal outcome in left-sided diaphragmatic hernia. J Pediatr Surg 27:778–779
Cordier AG, Jani JC, Cannie MM et al (2015) Stomach position in prediction of survival in left-sided congenital diaphragmatic hernia with or without fetoscopic endoluminal tracheal occlusion. Ultrasound Obstet Gynecol 46:155–161
Le LD, Keswani SG, Biesiada J et al (2012) The congenital diaphragmatic hernia composite prognostic index correlates with survival in left-sided congenital diaphragmatic hernia. J Pediatr Surg 47:57–62
Berman L, Jackson J, Miller K et al (2018) Expert surgical consensus for prenatal counseling using the Delphi method. J Pediatr Surg 53:1592–1599
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Brown, B.P., Clark, M.T., Wise, R.L. et al. A multifactorial severity score for left congenital diaphragmatic hernia in a high-risk population using fetal magnetic resonance imaging. Pediatr Radiol 49, 1718–1725 (2019). https://doi.org/10.1007/s00247-019-04478-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-019-04478-2