Abstract
Purpose
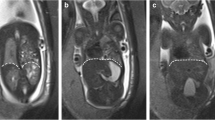
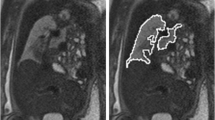
In congenital diaphragmatic hernia (CDH), ultrasound (U/S) measurements of the contralateral lung commonly provide the observed-to-expected lung-to-head ratio (O/E LHR) and are used to determine the severity of pulmonary hypoplasia. Fetal magnetic resonance imaging (MRI) measurement of the observed-to-expected total lung volume (O/E TLV) has been used as an adjunct to O/E LHR in predicting outcomes. Since O/E LHR only measures the contralateral lung, we sought to investigate if MRI measurements of the contralateral lung volume (O/E CLV) can accurately predict outcomes in CDH. We hypothesize that O/E CLV is a better predictor of CDH outcomes than O/E LHR.
Methods
We identified all infants with a prenatal diagnosis of CDH at our fetal center who had both MRI and U/S measurements. Using lung volume ratios of right–left 55:45, we calculated O/E CLV from O/E TLV. We used receiver-operating characteristic (ROC) curves to calculate the area under the curve (AUC) to compare the predictive accuracy of O/E CLV to O/E LHR for ECMO support, as well as survival to both discharge and 1 year.
Results
Seventy-four patients had complete prenatal imaging with 39% requiring ECMO support. The median O/E CLV was 48.0% and the median O/E LHR was 42.3%. O/E CLV was a better predictor of the need for ECMO support (AUC 0.81 vs. 0.74). O/E CLV was a better predictor of survival to discharge (AUC 0.84 vs. 0.64) and 1-year survival (AUC 0.83 vs. 0.63) than O/E LHR.
Conclusion
O/E LHR is a well-validated standard for predicting outcomes and guiding prenatal counseling in CDH. We provide evidence that fetal MRI measurements of the contralateral lung volume corrected for gestational age were more accurate in predicting the need for ECMO and survival. Future prospective studies validating O/E CLV regarding outcomes and ECMO utilization are warranted.
Level of evidence
Level III, retrospective comparative study.



Similar content being viewed by others
Change history
15 October 2021
A Correction to this paper has been published: https://doi.org/10.1007/s00383-021-05033-7
References
Congenital DM, Hernia D (2018) Management & outcomes. Adv in Pediatr 65(1):241
Leeuwen L, Fitzgerald DA (2014) Congenital diaphragmatic hernia. J Pediatr Child Health 50(9):667–673
Harting MT, Lally KP (2014) The congenital diaphragmatic hernia study group registry update. Semin Fetal Neonatal Med 19(6):370–375
Cordier AG, Russo FM, Deprest J, Benachi A (2019) Prenatal diagnosis, imaging, and prognosis in congenital diaphragmatic hernia. Semin Perinatol 44:51163
Metkus AP, Filly RA, Stringer MD, Harrison MR, Adzick NS (1996) Sonographic predictors of survival in fetal diaphragmatic hernia. J Pediatr Surg 31(1):148–152
Jani JC, Benachi A, Nicolaides KH, Allegaert K, Gratacos E, Mazkereth R et al (2009) Prenatal prediction of neonatal morbidity in survivors with congenital diaphragmatic hernia: a multicenter study. Ultrasound Obstet Gynecol 33(1):64–69
Van der Veeken L, Russo FM, De Catte L, Gratacos E, Benachi A, Ville Y et al (2018) Fetoscopic endoluminal tracheal occlusion and reestablishment of fetal airways for congenital diaphragmatic hernia. Gynecol Surg 15(1):9
Senat MV, Bouchghoul H, Stirnemann J, Vaast P, Boubnova J, Begue L et al (2018) Prognosis of isolated congenital diaphragmatic hernia using lung-area-to-head-circumference ratio: variability across centers in a national perinatal network. Ultrasound Obstet Gynecol 51(2):208–213
Hedrick HL, Danzer E, Merchant A, Bebbington M, Zhao H, Flake A et al (2007) Liver position and lung-to-head ratio for prediction of extracorporeal membrane oxygenation and survival in isolated left congenital diaphragmatic hernia. Am J Obstet Gynecol 197(4):422-e1
Victoria T, Danzer E, Oliver ER, Edgar JC, Iyoob S, Partridge EA et al (2018) Right congenital diaphragmatic hernias: is there a correlation between prenatal lung volume and postnatal survival, as in isolated left diaphragmatic hernias? Fetal Diagn Ther 43(1):12–8
Deshmukh S, Rubesova E, Barth R (2010) MR assessment of normal fetal lung volumes: a literature review. Am J Roentgenol 194(2):W212-7
Rypens F, Metens T, Rocourt N, Sonigo P, Brunelle F, Quere MP et al (2001) Fetal lung volume: estimation at MR imaging—initial results. Radiology 219(1):236–41
Cannie M, Jani J, Meersschaert J, Allegaert K, Done’ E, Marchal G et al (2008) Prenatal prediction of survival in isolated diaphragmatic hernia using observed to expected total fetal lung volume determined by magnetic resonance imaging based on either gestational age or fetal body volume. Ultrasound Obstet Gynecol 32(5):633–9
Kastenholz KE, Weis M, Hagelstein C, Weiss C, Kehl S, Schaible T et al (2016) Correlation of observed-to-expected MRI fetal lung volume and ultrasound lung-to-head ratio at different gestational times in fetuses with congenital diaphragmatic hernia. Am J Roentgenol 206(4):856–66
Victoria T, Bebbington MW, Danzer E, Flake AW, Johnson MP, Dinan D et al (2012) Use of magnetic resonance imaging in prenatal prognosis of the fetus with isolated left congenital diaphragmatic hernia. Prenat Diagn 32(8):715–23
Oluyomi-Obi T, Kuret V, Puligandla P, Lodha A, Lee-Robertson H, Lee K et al (2017) Antenatal predictors of outcome in prenatally diagnosed congenital diaphragmatic hernia (CDH). J Pediatr Surg 52(5):881–8
Bebbington M, Victoria T, Danzer E, Moldenhauer J, Khalek N, Johnson M et al (2014) Comparison of ultrasound and magnetic resonance imaging parameters in predicting survival in isolated left-sided congenital diaphragmatic hernia. Ultrasound Obstet Gynecol 43(6):670–4
Kim AG, Norwitz G, Karmakar M, Ladino-Torres M, Berman DR, Kreutzman J et al (2019) Discordant prenatal ultrasound and fetal MRI in CDH: wherein lies the truth? J Pediatr Surg 55:1879
Jani J, Cannie M, Done E, Van Mieghem T, Van Schoubroeck D, Gucciardo L et al (2007) Relationship between lung area at ultrasound examination and lung volume assessment with magnetic resonance imaging in isolated congenital diaphragmatic hernia. Ultrasound Obstet Gynecol 30(6):855–60
Coleman A, Phithakwatchara N, Shaaban A, Keswani S, Kline-Fath B, Kingma P et al (2015) Fetal lung growth represented by longitudinal changes in MRI-derived fetal lung volume parameters predicts survival in isolated left-sided congenital diaphragmatic hernia. Prenat Diagn 35(2):160–6
Lee TC, Lim FY, Keswani SG, Frischer JS, Haberman B, Kingma PS et al (2011) Late gestation fetal magnetic resonance imaging–derived total lung volume predicts postnatal survival and need for extracorporeal membrane oxygenation support in isolated congenital diaphragmatic hernia. J Pediatr Surg 46(6):1165–71
Abbasi N, Ryan G, Johnson A, Sanz Cortes M, Sangi-Haghpeykar H, Ye XY et al (2019) Reproducibility of fetal lung-to-head ratio in left diaphragmatic hernia across the North American fetal therapy network (NAFTNet). Prenat Diagn 39(3):188–94
Meyers ML, Garcia JR, Blough KL, Zhang W, Cassady CI, Mehollin-Ray AR (2018) Fetal lung volumes by MRI: normal weekly values from 18 through 38 weeks’ gestation. Am J Roentgenol 211(2):432–8
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has a conflict of interest to disclose.
Ethical approval
All of the procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
The study was evaluated and approved by the Colorado Multiple Institution Review Board (COMIRB), and a waiver of informed consent was obtained due to the retrospective nature of the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Phillips, R., Shahi, N., Meier, M. et al. The novel fetal MRI O/E CLV versus O/E LHR in predicting prognosis in congenital diaphragmatic hernias: can we teach an old dog new tricks?. Pediatr Surg Int 37, 1499–1504 (2021). https://doi.org/10.1007/s00383-021-04936-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-021-04936-9