Abstract
The relationships between maternal exposure to endocrine-disrupting chemicals (EDCs) and congenital heart diseases (CHD) are not elucidated yet. The exposure levels of EDCs are generally estimated based on self-reported questionnaires or occupational exposure evaluations in the literature. Therefore, a study based on epidemiological data from human biospecimens is required to provide stronger evidence between maternal exposure to EDC and CHD. Embase, Pubmed, Scopus, and the Cochrane Library databases were searched for related research which provided risk estimates regarding the relationships between maternal EDC exposure and CHD in human offspring. Baseline characteristics and outcomes of CHD were extracted from each included study. Odds ratios (ORs) with 95% confidence intervals (CIs) were pooled to calculate the overall estimates of CHD. Subgroup and meta-regression analyses were performed to identify the sources of heterogeneity. Bootstrapping techniques were used in analyses where several studies originated from a similar population. A total of seventeen studies were involved in the meta-analyses. Maternal EDC exposure was significantly related to CHD in offspring (OR 2.15; 95%CI 1.64 to 2.83). EDC exposure was significantly associated with septal defects (OR 2.34; 95%CI 1.77 to 3.10), conotruncal defects (OR 2.54; 95%CI 1.89 to 3.43), right ventricular outflow tract obstruction (OR 2.65; 95%CI 1.73 to 4.07), left ventricular outflow tract obstruction (OR 3.58; 95%CI 2.67 to 4.79), anomalous pulmonary venous return (OR 2.31; 95%CI 1.34 to 4.00), and other heart defects (OR 2.49; 95%CI 1.75 to 3.54). In addition, maternal exposure to heavy metals, which included lead (OR 2.19; 95%CI 1.29 to 3.71), cadmium (OR 1.81; 95%CI 1.28 to 2.56), mercury (OR 2.23; 95%CI 1.13 to 4.44), and manganese (OR 2.65; 95%CI 1.48 to 4.74), increased risks for CHD significantly. In conclusion, based on the latest evidence, maternal EDC exposure may increase CHD risks in human offspring, especially in heavy metal exposure conditions.






Similar content being viewed by others
Data Availability
The datasets during and/or analyzed during the current study available from the corresponding author on reasonable request.
References
Kabir ER, Rahman MS, Rahman I (2015) A review on endocrine disruptors and their possible impacts on human health. Environ Toxicol Pharmacol 40(1):241–258
Yilmaz B, Terekeci H, Sandal S, Kelestimur F (2020) Endocrine disrupting chemicals: exposure, effects on human health, mechanism of action, models for testing and strategies for prevention. Rev Endocr Metab Disord 21(1):127–147
Wu Y, Wang J, Wei Y, Chen J, Kang L, Long C, Wu S, Shen L, Wei G (2022) Maternal exposure to endocrine disrupting chemicals (EDCs) and preterm birth: a systematic review, meta-analysis, and meta-regression analysis. Environ Pollut 292(Pt A):118264
Lucas A, Herrmann S, Lucas M (2022) The role of endocrine-disrupting phthalates and bisphenols in cardiometabolic disease: the evidence is mounting. Curr Opin Endocrinol Diabetes Obes 29(2):87–94
Mariana M, Feiteiro J, Verde I, Cairrao E (2016) The effects of phthalates in the cardiovascular and reproductive systems: a review. Environ Int 94:758–776
Hirke A, Varghese B, Varade S, Adela R (2023) Exposure to endocrine-disrupting chemicals and risk of gestational hypertension and preeclampsia: a systematic review and meta-analysis. Environ Pollut 317:120828
Osorio-Yáñez C, Sanchez-Guerra M, Cardenas A, Lin PD, Hauser R, Gold DR, Kleinman KP, Hivert MF, Fleisch AF, Calafat AM, Webster TF, Horton ES, Oken E (2021) Per- and polyfluoroalkyl substances and calcifications of the coronary and aortic arteries in adults with prediabetes: results from the diabetes prevention program outcomes study. Environ Int 151:106446
Zhang S, Zhang B, Wu J, Luo J, Shi H, Qi J, Yang H (2023) The prevalence of congenital heart disease among school-age children in China: a meta-analysis and systematic review. Congenit Heart Dis 18(2):127–150.
Snijder CA, Vlot IJ, Burdorf A, Obermann-Borst SA, Helbing WA, Wildhagen MF, Steegers EA, Steegers-Theunissen RP (2012) Congenital heart defects and parental occupational exposure to chemicals. Hum Reprod 27(5):1510–1517
Li YF, Canário AVM, Power DM, Campinho MA (2019) Ioxynil and diethylstilbestrol disrupt vascular and heart development in zebrafish. Environ Int 124:511–520
Zhou R, Cheng W, Feng Y, Wei H, Liang F, Wang Y (2017) Interactions between three typical endocrine-disrupting chemicals (EDCs) in binary mixtures exposure on myocardial differentiation of mouse embryonic stem cell. Chemosphere 178:378–383
Rocheleau CM, Bertke SJ, Lawson CC, Romitti PA, Sanderson WT, Malik S, Lupo PJ, Desrosiers TA, Bell E, Druschel C, Correa A, Reefhuis J. Maternal occupational pesticide exposure and risk of congenital heart defects in the National Birth Defects Prevention Study. Birth Defects Res A Clin Mol Teratol. 2015, 103(10):823–33.
Hayama-Terada M, Aochi Y, Ikehara S, Kimura T, Yamagishi K, Sato T, Iso H (2023) Paternal occupational exposures and infant congenital heart defects in the Japan Environment and Children’s Study. Environ Health Prev Med 28:12
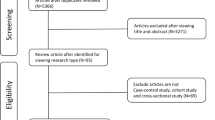
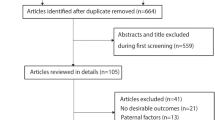
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71
Bonde JP, Flachs EM, Rimborg S, Glazer CH, Giwercman A, Ramlau-Hansen CH, Hougaard KS, Høyer BB, Hærvig KK, Petersen SB, Rylander L, Specht IO, Toft G, Bräuner EV (2016) The epidemiologic evidence linking prenatal and postnatal exposure to endocrine disrupting chemicals with male reproductive disorders: a systematic review and meta-analysis. Hum Reprod Update 23(1):104–125
Sterne JAC, Hernan MA, Reeves BC, Savovic J, Berkman ND, Viswanathan M et al (2016) ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 355:i4919
Hu H, Liu Z, Li J, Li S, Tian X, Lin Y, Chen X, Yang J, Deng Y, Li N, Wang Y, Yuan P, Li X, Zhu J (2014) Correlation between congenital heart defects and maternal copper and zinc concentrations. Birth Defects Res A Clin Mol Teratol 100(12):965–972
Liu Z, Yu Y, Li X, Wu A, Mu M, Li N, Deng Y, Jin X, Li S, Lin Y, Chen X, Wang F, Zhu J (2015) Maternal lead exposure and risk of congenital heart defects occurrence in offspring. Reprod Toxicol 51:1–6
Jin X, Tian X, Liu Z, Hu H, Li X, Deng Y, Li N, Zhu J (2016) Maternal exposure to arsenic and cadmium and the risk of congenital heart defects in offspring. Reprod Toxicol 59:109–116
Liu Z, Lin Y, Tian X, Li J, Chen X, Yang J, Li X, Deng Y, Li N, Liang J, Li S, Zhu J (2016) Association between maternal aluminum exposure and the risk of congenital heart defects in offspring. Birth Defects Res A Clin Mol Teratol 106(2):95–103
Ou Y, Bloom MS, Nie Z, Han F, Mai J, Chen J, Lin S, Liu X, Zhuang J (2017) Associations between toxic and essential trace elements in maternal blood and fetal congenital heart defects. Environ Int 106:127–134
Li N, Mu Y, Liu Z, Deng Y, Guo Y, Zhang X, Li X, Yu P, Wang Y, Zhu J (2018) Assessment of interaction between maternal polycyclic aromatic hydrocarbons exposure and genetic polymorphisms on the risk of congenital heart diseases. Sci Rep 8(1):3075
Liu Z, He C, Chen M, Yang S, Li J, Lin Y, Deng Y, Li N, Guo Y, Yu P, Li X (2018) The effects of lead and aluminum exposure on congenital heart disease and the mechanism of oxidative stress. Reprod Toxicol 81:93–98
Zhang N, Liu Z, Tian X, Chen M, Deng Y, Guo Y, Li N, Yu P, Yang J, Zhu J (2018) Barium exposure increases the risk of congenital heart defects occurrence in offspring. Clin Toxicol 56(2):132–139
Zhang N, Chen M, Li J, Deng Y, Li SL, Guo YX, Li N, Lin Y, Yu P, Liu Z, Zhu J (2019) Metal nickel exposure increase the risk of congenital heart defects occurrence in offspring: a case-control study in China. Medicine 98(18):e15352
Zhang N, Yang S, Yang J, Deng Y, Li S, Li N, Chen X, Yu P, Liu Z, Zhu J (2020) Association between metal cobalt exposure and the risk of congenital heart defect occurrence in offspring: a multi-hospital case-control study. Environ Health Prev Med 25(1):38
Ou Y, Zeng X, Lin S, Bloom MS, Han F, Xiao X, Wang H, Matala R, Li X, Qu Y, Nie Z, Dong G, Liu X (2021) Gestational exposure to perfluoroalkyl substances and congenital heart defects: a nested case-control pilot study. Environ Int 154:106567
Salehi F, Darmiani K, Nakhaee S, Zadeh AA, Javadmoosavi SY, Faghihi V, Mehrpour O (2022) Comparison of blood lead concentrations in mothers of children with congenital heart disease and mothers of healthy children. Biol Trace Elem Res 200(5):2001–2007
Sun J, Mao B, Wu Z, Jiao X, Wang Y, Lu Y, Ma X, Liu X, Xu X, Cui H, Lin X, Yi B, Qiu J, Liu Q (2022) Relationship between maternal exposure to heavy metal titanium and offspring congenital heart defects in Lanzhou, China: a nested case-control study. Front Public Health 10:946439
Wang C, Pi X, Yin S, Liu M, Tian T, Jin L, Liu J, Li Z, Wang L, Yuan Z, Wang Y, Ren A (2022) Maternal exposure to heavy metals and risk for severe congenital heart defects in offspring. Environ Res 212(Pt C):113432
Wang M, Tian Y, Yu P, Li N, Deng Y, Li L, Kang H, Chen D, Wang H, Liu Z, Liang J (2022) Association between congenital heart defects and maternal manganese and iron concentrations: a case-control study in China. Environ Sci Pollut Res Int 29(18):26950–26959
Huang L, Mao B, Li J, Nan N, He L, Qiu J, Yi B, Liu Q (2023) Associations between the lead level in maternal blood and umbilical cord blood and congenital heart diseases in offspring. Biol Trace Elem Res 201(5):2191–2199
Luan YL, Ou YQ, Liu XQ, Lin S, Guo Y (2023) Triclosan in paired-maternal and cord blood, and their relationships with congenital heart disease of baby. Sci Total Environ 857(Pt 1):159205
Gunter TE, Gerstner B, Lester T, Wojtovich AP, Malecki J, Swarts SG, Brookes PS, Gavin CE, Gunter KK (2010) An analysis of the effects of Mn2+ on oxidative phosphorylation in liver, brain, and heart mitochondria using state 3 oxidation rate assays. Toxicol Appl Pharmacol 249(1):65–75
Thompson J, Bannigan J (2008) Cadmium: toxic effects on the reproductive system and the embryo. Reprod Toxicol 25(3):304–315
Gollenberg AL, Hediger ML, Lee PA, Himes JH, Louis GM (2010) Association between lead and cadmium and reproductive hormones in peripubertal U.S. girls. Environ Health Perspect. 118(12):1782–7
Gorini F, Chiappa E, Gargani L, Picano E (2014) Potential effects of environmental chemical contamination in congenital heart disease. Pediatr Cardiol 35(4):559–568
Li S, Wang Q, Luo W, Jia S, Liu D, Ma W, Gu H, Wei X, He Y, Cao S, Yuan Z (2022) Relationship between maternal heavy metal exposure and congenital heart defects: a systematic review and meta-analysis. Environ Sci Pollut Res Int 29(37):55348–55366
Acknowledgements
None.
Funding
Chongqing Medical University Program for Youth Innovation in Future Medicine (W0204) and Natural Science Foundation Project of Chongqing, Chongqing Science and Technology Commission (CSTB2023NSCQ-BHX0010).
Author information
Authors and Affiliations
Contributions
Study conception and design: Jiangtao Dai and Yuhao Wu; Data acquisition: Gang Wang and Chun Wu; Analysis and data interpretation: Zhengxia Pan and Hongbo Li; Drafting of the manuscript: Lianju Shen; Critical revision: Yuhao Wu.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical Approval and Consent to Participate
Ethics approval was waived by the Institutional Review Board (IRB) of the Children’s Hospital of Chongqing Medical University. Consent to participate was not applicable.
Consent for Publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dai, J., Wang, G., Wu, C. et al. Exposure to Endocrine-Disrupting Chemicals and Congenital Heart Diseases: The Pooled Results Based on the Current Evidence. Pediatr Cardiol (2024). https://doi.org/10.1007/s00246-024-03478-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00246-024-03478-w