Abstract
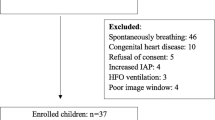
Proper assessment of fluid responsiveness using accurate predictors is crucial to guide fluid therapy and avoid the serious adverse effects of fluid overload. The main objective of this study was to investigate the accuracy of respiratory variations in inferior vena cava diameter (∆IVC) to predict fluid responsiveness in mechanically ventilated children. This prospective single-center study included 32 children (median age and weight of 17 months and 10 kg, respectively) who received a fluid infusion of 10 ml kg–1 of crystalloid solutions over 10 min. ∆IVC and respiratory variation in aortic blood flow peak velocity (∆Vpeak) were determined over one controlled respiratory cycle before and after fluid loading. Thirteen (41%) participants were fluid-responders. ∆IVC, ∆Vpeak, stroke volume index, and cardiac index were found to be predictors of fluid responsiveness. However, the area under the ROC curve of ∆IVC was smaller when compared to ∆Vpeak (0.709 vs. 0.935, p < 0.012). The best cut-off values were 7.7% for ∆IVC (sensitivity, 69.2%; specificity 78.9%, positive predictive value, 69.2%; and negative predictive value, 78.9%) and 18.2% for ∆Vpeak (sensitivity, 84.6%; specificity, 89.5%; positive predictive value, 84.6%; negative predictive value, 89.5%). Changes in stroke volume were positively correlated with ∆IVC (ρ = 0.566, p < 0.001) and ∆Vpeak (ρ = 0.603, p < 0.001). A significant correlation was also found between changes in MAP and ∆Vpeak (ρ = 0.382; p = 0.031), but the same was not observed with ∆IVC (ρ = 0.011; p = 0.951). In conclusion, ∆IVC was found to have a moderate accuracy in predicting fluid responsiveness in mechanically ventilated children and is an inferior predictor when compared to ∆Vpeak.


Similar content being viewed by others
Data Availability
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
Code Availability
Not applicable.
Abbreviations
- ΔIVC:
-
Respiratory variation of inferior vena cava diameters
- ∆Vpeak:
-
Respiratory variation in aortic blood flow peak velocity
- AUROC:
-
Area under the ROC curve
- Ci:
-
Cardiac index
- Da:
-
Aortic diameter
- IQR:
-
Interquartile range
- IVC:
-
Inferior vena cava
- MAP:
-
Mean arterial pressure
- NPV:
-
Negative predictive value
- PICU:
-
Pediatric intensive care unit
- POCUS:
-
Point-of-care ultrasound
- PPV:
-
Positive predictive value
- ROC curve:
-
Receiver operating characteristic curve
- SV:
-
Stroke volume
- SVi:
-
Stroke volume index
- TTE:
-
Transthoracic echocardiography
- VTI:
-
Velocity–time integral
References
Alobaidi R, Morgan C, Basu RK et al (2018) Association between fluid balance and outcomes in critically ill children: a systematic review and meta-analysis. JAMA Pediatr 172:257–268. https://doi.org/10.1001/jamapediatrics.2017.4540
Gan H, Cannesson M, Chandler JR, Ansermino JM (2013) Predicting fluid responsiveness in children: a systematic review. Anesth Analg 117:1380–1392. https://doi.org/10.1213/ANE.0b013e3182a9557e
Luo D, Liu F, Dai W et al (2021) Diagnostic accuracy of stroke volume variation for predicting fluid responsiveness in children undergoing cardiac surgery: a systematic review and meta-analysis. Pediatr Anesth 31:755–762. https://doi.org/10.1111/PAN.14195
Yi L, Liu Z, Qiao L et al (2017) Does stroke volume variation predict fluid responsiveness in children: a systematic review and meta-analysis. PLoS One 12:e0177590. https://doi.org/10.1371/JOURNAL.PONE.0177590
Feissel M, Michard F, Faller J-P, Teboul J-L (2004) The respiratory variation in inferior vena cava diameter as a guide to fluid therapy. Intensive Care Med 30:1834–1837. https://doi.org/10.1007/s00134-004-2233-5
Barbier C, Loubieres Y, Schmit C et al (2004) Respiratory changes in inferior vena cava diameter are helpful in predicting fluid responsiveness in ventilated septic patients. Intensive Care Med 30:1740–1746. https://doi.org/10.1007/s00134-004-2259-8
Orso D, Paoli I, Piani T et al (2018) Accuracy of ultrasonographic measurements of inferior vena cava to determine fluid responsiveness: a systematic review and meta-analysis. J Intensive Care Med. https://doi.org/10.1177/0885066617752308
de Souza TH, Giatti MP, Nogueira RJN et al (2020) Inferior vena cava ultrasound in children: comparing two common assessment methods. Pediatr Crit Care Med 21:E186–E191. https://doi.org/10.1097/PCC.0000000000002240
Ranjit S, Natraj R, Kissoon N et al (2020) Variability in the physiologic response to fluid bolus in pediatric patients following cardiac surgery. Crit Care Med 48:E1062–E1070. https://doi.org/10.1097/CCM.0000000000004621
Ranjit S, Natraj R, Kissoon N et al (2021) Variability in the hemodynamic response to fluid bolus in pediatric septic shock. Pediatr Crit Care Med 22:E448–E458. https://doi.org/10.1097/PCC.0000000000002714
DeLong ER, DeLong DM, Clarke-Pearson DL (1988) Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 44:837–845
Choi YA, Kwon H, Lee JH et al (2018) Comparison of sonographic inferior vena cava and aorta indexes during fluid administered in children. Am J Emerg Med 36:1529–1533. https://doi.org/10.1016/J.AJEM.2018.01.010
Byon H-J, Lim C-W, Lee J-H et al (2013) Prediction of fluid responsiveness in mechanically ventilated children undergoing neurosurgery. Br J Anaesth 110:586–591. https://doi.org/10.1093/bja/aes467
El-Halimi K, Negadi M, Bouguetof H et al (2015) Respiratory variations in aortic blood flow velocity and inferior vena cava diameter as predictors of fluid responsiveness in mechanically ventilated children using transthoracic echocardiography in a pediatric PICU. Crit Care 19:S62–S63. https://doi.org/10.1186/CC14261
Weber T, Wagner T, Neumann K, Deusch E (2015) Low predictability of three different noninvasive methods to determine fluid responsiveness in critically ill children. Pediatr Crit Care Med 16:e89-94. https://doi.org/10.1097/PCC.0000000000000364
Achar SK, Sagar MS, Shetty R et al (2016) Respiratory variation in aortic flow peak velocity and inferior vena cava distensibility as indices of fluid responsiveness in anaesthetised and mechanically ventilated children. Indian J Anaesth 60:121–126. https://doi.org/10.4103/0019-5049.176285
Long E, Duke T, Oakley E et al (2018) Does respiratory variation of inferior vena cava diameter predict fluid responsiveness in spontaneously ventilating children with sepsis. Emerg Med Australas 30:556–563. https://doi.org/10.1111/1742-6723.12948
El-Nawawy AA, Omar OM, Hassouna HM (2021) Role of inferior vena cava parameters as predictors of fluid responsiveness in pediatric septic shock: a prospective study. J Child Sci 11:E49–E54. https://doi.org/10.1055/S-0041-1724034
Shostak E, Shochat T, Manor O et al (2021) Fluid responsiveness predictability in immediate postoperative pediatric cardiac surgery. Is the old slandered central venous pressure back again? Shock 56:927–932. https://doi.org/10.1097/SHK.0000000000001786
Singh A, Kumar B, Puri GD et al (2022) Utility of transfontanelle ultrasound in predicting the fluid responsiveness in children after repair of congenital heart diseases: a prospective observational study. J Cardiothorac Vasc Anesth. https://doi.org/10.1053/J.JVCA.2022.01.035
Xiong Z, Zhang G, Zhou Q et al (2022) Predictive value of the respiratory variation in inferior vena cava diameter for ventilated children with septic shock. Front Pediatr. https://doi.org/10.3389/FPED.2022.895651
Blehar DJ, Resop D, Chin B et al (2012) Inferior vena cava displacement during respirophasic ultrasound imaging. Crit Ultrasound J 4:18. https://doi.org/10.1186/2036-7902-4-18
Wallace DJ, Allison M, Stone MB (2010) Inferior vena cava percentage collapse during respiration is affected by the sampling location: an ultrasound study in healthy volunteers. Acad Emerg Med 17:96–99. https://doi.org/10.1111/J.1553-2712.2009.00627.X
Finnerty NM, Panchal AR, Boulger C et al (2017) Inferior vena cava measurement with ultrasound: what is the best view and best mode? West J Emerg Med 18:496. https://doi.org/10.5811/WESTJEM.2016.12.32489
Yamanoʇlu NGÇ, Yamanoʇlu A, Parlak I et al (2015) The role of inferior vena cava diameter in volume status monitoring; the best sonographic measurement method? Am J Emerg Med 33:433–438. https://doi.org/10.1016/J.AJEM.2014.12.014
Long E, Oakley E, Duke T, Babl FE (2017) Does respiratory variation in inferior vena cava diameter predict fluid responsiveness: a systematic review and meta-analysis. Shock 47:550–559. https://doi.org/10.1097/SHK.0000000000000801
Carioca FL, de Souza FM, de Souza TB et al (2022) Point-of-care ultrasonography to predict fluid responsiveness in children: A systematic review and meta-analysis. Pediatr Anaesth 00:1–14. https://doi.org/10.1111/PAN.14574
Ibarra-Estrada M, López-Pulgarín JA, Mijangos-Méndez JC et al (2015) Respiratory variation in carotid peak systolic velocity predicts volume responsiveness in mechanically ventilated patients with septic shock: a prospective cohort study. Crit Ultrasound J 7:1–9. https://doi.org/10.1186/S13089-015-0029-1
Pierrakos C, Velissaris D, Scolletta S et al (2012) Can changes in arterial pressure be used to detect changes in cardiac index during fluid challenge in patients with septic shock? Intensive Care Med 38:422–428. https://doi.org/10.1007/S00134-011-2457-0
de Souza TB, Rubio AJ, de Siqueira FI et al (2022) Carotid doppler ultrasonography as a method to predict fluid responsiveness in mechanically ventilated children. Pediatr Anesth. https://doi.org/10.1111/PAN.14513
Chew MS, Poelaert J (2003) Accuracy and repeatability of pediatric cardiac output measurement using doppler: 20-year review of the literature. Intensive Care Med 29:1889–1894. https://doi.org/10.1007/s00134-003-1967-9
Acknowledgements
Thanks to Carolina Grotta Ramos Telio for her review of the article. We also thank the nursing, technical staff, and the pediatric intensive care residents.
Funding
No external funding for this manuscript.
Author information
Authors and Affiliations
Contributions
NC and LdL: responsible for data collection, drafting and critical revision of the manuscript. IF, RN, and MB: responsible for critical revision of the manuscript for important intellectual content. TdS: responsible for the study concept and design, data collection, analysis and interpretation of data.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest relevant to this study to disclose.
Ethics Approval
The study was approved by the local institutional review board (UNICAMP’s Research and Ethics Committee, approval number 12894719.8.0000.5404).
Informed Consent
Written informed consent was obtained from the participants’ legal guardian.
Consent for Publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Campos, N.B., de Lima, L.B., Ferraz, I.d. et al. Accuracy of Respiratory Variation in Inferior Vena Cava Diameter to Predict Fluid Responsiveness in Children Under Mechanical Ventilation. Pediatr Cardiol (2023). https://doi.org/10.1007/s00246-023-03115-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00246-023-03115-y