Abstract
Purpose
The purposes of this study are to study the impact of deep brain involvement on overall survival (OS) and progression-free survival (PFS) in intracranial primary CNS lymphoma (PCNSL), and to explore possible mechanisms for this impact using advanced MRI techniques.
Methods
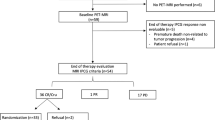
Seventy-nine patients with histologically verified PCNSL were identified from a prospective clinical database of patients treated at Oslo University Hospital between 2003 and 2014. Patients were treated per standard chemotherapeutic regimens (N = 57) or no chemotherapy (N = 22). Anatomical MRIs were available in all patients to assess tumor load and location based on contrast agent enhancement visible on T1-weighted images. Diffusion MRIs were available in 33 (42%) patients and perfusion MRI in 13 (16%) patients that received active treatment.
Results
Across all patients, OS and PFS were 16.4 and 9.8 months, respectively. In multivariate analysis, MRI-based deep brain involvement (80%) was the only negative significant factor of OS (OR = 14.2; P < 0.005). While a reduced Karnofsky performance status was associated with deep brain involvement (P < 0.05), neither chemotherapy regimen, neurologic status, nor patient age were independent significant factors for OS or PFS in this setting. Compared to other tumors and healthy tissue levels, MRI perfusion showed more pathologic hemodynamic flow signatures in tumors with deep brain involvement.
Conclusion
In intracranial PCNSL, the only significant prognostic factor for OS and PFS in multivariate analysis was age and deep brain involvement. While contingent on a small study sample, we hypothesize this may in part be explained by regional differences in vascular supply and delivery from a dysfunctional perfusion signature.




Similar content being viewed by others

References
Norden AD, Drappatz J, Wen PY, Claus EB (2010) Survival among patients with primary central nervous system lymphoma, 1973-2004. J Neuro-Oncol 101(3):487–493
Ferreri AJ, Blay JY, Reni M, Pasini F, Spina M, Ambrosetti A et al (2003) Prognostic scoring system for primary CNS lymphomas: the international extranodal lymphoma study group experience. J Clin Oncol 21(2):266–272
Bessell EM, Graus F, Lopez-Guillermo A, Lewis SA, Villa S, Verger E, Petit J (2004) Primary non-Hodgkin’s lymphoma of the CNS treated with CHOD/BVAM or BVAM chemotherapy before radiotherapy: long-term survival and prognostic factors. Int J Radiat Oncol Biol Phys 59(2):501–508
Jahr G, Da Broi M, Holthe Jr H, Beiske K, Meling TR (2018) Evaluation of MSKCC and IELSG prognostic scoring systems to predict overall survival in intracranial primary CNS lymphoma. Brain Behav in press
Ghesquieres H, Drouet Y, Sunyach MP, Sebban C, Chassagne-Clement C, Jouanneau E et al (2013) Evidence of time-dependent prognostic factors predicting early death but not long-term outcome in primary CNS lymphoma: a study of 91 patients. Hematol Oncol 31(2):57–64
Schorb E, Kasenda B, Atta J, Kaun S, Morgner A, Hess G, Elter T, von Bubnoff N, Dreyling M, Ringhoffer M, Krause SW, Derigs G, Klimm B, Niemann D, Fritsch K, Finke J, Illerhaus G (2013) Prognosis of patients with primary central nervous system lymphoma after high-dose chemotherapy followed by autologous stem cell transplantation. Haematologica 98(5):765–770
Ghesquières H, Ferlay C, Sebban C, Perol D, Bosly A, Casasnovas O et al (2010) Long-term follow-up of an age-adapted C5R protocol followed by radiotherapy in 99 newly diagnosed primary CNS lymphomas: a prospective multicentric phase II study of the Groupe d'Etude des Lymphomes de l'Adulte (GELA). Ann Oncol 21(4):842–850
Abrey LE, Ben-Porat L, Panageas KS, Yahalom J, Berkey B, Curran W, Schultz C, Leibel S, Nelson D, Mehta M, DeAngelis LM (2006) Primary central nervous system lymphoma: the Memorial Sloan-Kettering Cancer Center prognostic model. J Clin Oncol 24(36):5711–5715
Viallon M, Cuvinciuc V, Delattre B, Merlini L, Barnaure-Nachbar I, Toso-Patel S, Becker M, Lovblad KO, Haller S (2015) State-of-the-art MRI techniques in neuroradiology: principles, pitfalls, and clinical applications. Neuroradiology 57(5):441–467
Covarrubias DJ, Rosen BR, Lev MH (2004) Dynamic magnetic resonance perfusion imaging of brain tumors. Oncologist 9(5):528–537
Xu W, Wang Q, Shao A, Xu B, Zhang J (2017) The performance of MR perfusion-weighted imaging for the differentiation of high-grade glioma from primary central nervous system lymphoma: a systematic review and meta-analysis. PLoS One 12(3):e0173430
Blasel S, Jurcoane A, Bahr O, Weise L, Harter PN, Hattingen E (2013) MR perfusion in and around the contrast-enhancement of primary CNS lymphomas. J Neuro-Oncol 114(1):127–134
Lister A, Abrey LE, Sandlund JT (2002) Central nervous system lymphoma. Hematology Am Soc Hematol Educ Program 2002(1):283–296
Hasan KM, Ali H, Shad MU (2013) Atlas-based and DTI-guided quantification of human brain cerebral blood flow: feasibility, quality assurance, spatial heterogeneity and age effects. Magn Reson Imaging 31(8):1445–1452
Baraniskin A, Deckert M, Schulte-Altedorneburg G, Schlegel U, Schroers R (2012) Current strategies in the diagnosis of diffuse large B-cell lymphoma of the central nervous system. Br J Haematol 156(4):421–432
Pulczynski EJ, Kuittinrn O, Erlanson M, Hagberg H, Nordstrøm M, Østenstad B et al (2015) Successful change of treatment strategy in elderly patients with primary central nervous system lymphoma by de-escalating induction and introducing temozolomide maintenance: results from a phase II study by the Nordic lymphoma group. Haematologica 100:534–540
Hrabe J, Kaur G, Guilfoyle DN (2007) Principles and limitations of NMR diffusion measurements. J Med Phys 32(1):34–42
Emblem KE, Pinho MC, Zollner FG, Due-Tonnessen P, Hald JK, Schad LR et al (2015) A generic support vector machine model for preoperative glioma survival associations. Radiology 275(1):228–234
Neska-Matuszewska M, Bladowska J, Sasiadek M, Zimny A (2018) Differentiation of glioblastoma multiforme, metastases and primary central nervous system lymphomas using multiparametric perfusion and diffusion MR imaging of a tumor core and a peritumoral zone-searching for a practical approach. PLoS One 13(1):e0191341
Abrey LE, Batchelor TT, Ferreri AJ, Gospodarowicz M, Pulczynski EJ, Zucca E, Smith JR, Korfel A, Soussain C, DeAngelis L, Neuwelt EA, O'Neill BP, Thiel E, Shenkier T, Graus F, van den Bent M, Seymour JF, Poortmans P, Armitage JO, Cavalli F, International Primary CNS Lymphoma Collaborative Group (2005) Report of an international workshop to standardize baseline evaluation and response criteria for primary CNS lymphoma. J Clin Oncol 23(22):5034–5043
Elder JB, Chen TC (2006) Surgical interventions for primary central nervous system lymphoma. Neurosurg Focus 21(5):E13
Blasel S, Vorwerk R, Kiyose M, Mittelbronn M, Brunnberg U, Ackermann H, Voss M, Harter PN, Hattingen E (2018) New MR perfusion features in primary central nervous system lymphomas: pattern and prognostic impact. J Neurol 265(3):647–658
Kim YS, Choi SH, Yoo RE, Kang KM, Yun TJ, Kim JH, Sohn CH, Park SH, Won JK, Kim TM, Park CK, Kim IH (2018) Leakage correction improves prognosis prediction of dynamic susceptibility contrast perfusion MRI in primary central nervous system lymphoma. Sci Rep 8(1):456
Jespersen SN, Ostergaard L (2012) The roles of cerebral blood flow, capillary transit time heterogeneity, and oxygen tension in brain oxygenation and metabolism. J Cereb Blood Flow Metab 32(2):264–277
Shin W, Horowitz S, Ragin A, Chen Y, Walker M, Carroll TJ (2007) Quantitative cerebral perfusion using dynamic susceptibility contrast MRI: evaluation of reproducibility and age- and gender-dependence with fully automatic image postprocessing algorithm. Magn Reson Med 58(6):1232–1241
Bjornerud A, Emblem KE (2010) A fully automated method for quantitative cerebral hemodynamic analysis using DSC-MRI. J Cereb Blood Flow Metab 30(5):1066–1078
Digernes I, Bjornerud A, Vatnehol SAS, Lovland G, Courivaud F, Vik-Mo E et al (2017) A theoretical framework for determining cerebral vascular function and heterogeneity from dynamic susceptibility contrast MRI. J Cereb Blood Flow Metab 37(6):2237–2248
Wilhelm I, Nyul-Toth A, Suciu M, Hermenean A, Krizbai IA (2016) Heterogeneity of the blood-brain barrier. Tissue Barriers 4(1):e1143544
Schultz C, Scott C, Sherman W, Donahue B, Fields J, Murray K, Fisher B, Abrams R, Meis-Kindblom J (1996) Preirradiation chemotherapy with cyclophosphamide, doxorubicin, vincristine, and dexamethasone for primary CNS lymphomas: initial report of radiation therapy oncology group protocol 88-06. J Clin Oncol 14(2):556–564
Gavrilovic IT, Hormigo A, Yahalom J, DeAngelis LM, Abrey LE (2006) Long-term follow-up of high-dose methotrexate-based therapy with and without whole brain irradiation for newly diagnosed primary CNS lymphoma. J Clin Oncol 24(28):4570–4574
Batchelor T, Carson K, O’Neill A, Grossman SA, Alavi J, New P et al (2003) Treatment of primary CNS lymphoma with methotrexate and deferred radiotherapy: a report of NABTT 96-07. J Clin Oncol 21(6):1044–1049
Fraser E, Gruenberg K, Rubenstein JL (2015) New approaches in primary central nervous system lymphoma. Chin Clin Oncol 4(1):11
Hoang-Xuan K, Bessell E, Bromberg J, Hottinger AF, Preusser M, Rudà R, Schlegel U, Siegal T, Soussain C, Abacioglu U, Cassoux N, Deckert M, Dirven CM, Ferreri AJ, Graus F, Henriksson R, Herrlinger U, Taphoorn M, Soffietti R, Weller M, European Association for Neuro-Oncology Task Force on Primary CNS Lymphoma (2015) Diagnosis and treatment of primary CNS lymphoma in immunocompetent patients: guidelines from the European Association for Neuro-Oncology. Lancet Oncol 16(7):e322–e332
Ferreri AJ, Reni M, Foppoli M, Martelli M, Pangalis GA, Frezzato M et al (2009) High-dose cytarabine plus high-dose methotrexate versus high-dose methotrexate alone in patients with primary CNS lymphoma: a randomised phase 2 trial. Lancet 374(9700):1512–1520
Ly KI, Crew LL, Graham CA, Mrugala MM (2016) Primary central nervous system lymphoma treated with high-dose methotrexate and rituximab: a single-institution experience. Oncol Lett 11(5):3471–3476
Madle M, Kramer I, Lehners N, Schwarzbich M, Wuchter P, Herfarth K et al (2015) The influence of rituximab, high-dose therapy followed by autologous stem cell transplantation, and age in patients with primary CNS lymphoma. Ann Hematol 94(11):1853–1857
Morris PG, Correa DD, Yahalom J, Raizer JJ, Schiff D, Grant B, Grimm S, Lai RK, Reiner AS, Panageas K, Karimi S, Curry R, Shah G, Abrey LE, DeAngelis LM, Omuro A (2013) Rituximab, methotrexate, procarbazine, and vincristine followed by consolidation reduced-dose whole-brain radiotherapy and cytarabine in newly diagnosed primary CNS lymphoma: final results and long-term outcome. J Clin Oncol 31(31):3971–3979
Houillier C, Ghesquieres H, Chabrot C, Soussain C, Ahle G, Choquet S et al (2017) Rituximab, methotrexate, procarbazine, vincristine and intensified cytarabine consolidation for primary central nervous system lymphoma (PCNSL) in the elderly: a LOC network study. J Neuro-Oncol 133(2):315–320
Hitchcock SA, Pennington LD (2006) Structure-brain exposure relationships. J Med Chem 49(26):7559–7583
Baetke SC, Lammers T, Kiessling F (2015) Applications of nanoparticles for diagnosis and therapy of cancer. Br J Radiol 88(1054):20150207
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this study.
Conflict of interest
KEE has intellectual property rights at NordicNeuroLab AS, Bergen, Norway.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required.
Informed consent
For this type of retrospective study formal consent is not required.
Rights and permissions
About this article
Cite this article
Meling, T.R., Latysheva, A., Da Broi, M. et al. Is deep brain involvement in intracranial primary central nervous system lymphoma of importance for penetration of chemotherapeutic agents?. Neuroradiology 60, 703–713 (2018). https://doi.org/10.1007/s00234-018-2038-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-018-2038-9